How Is Melanoma Staged
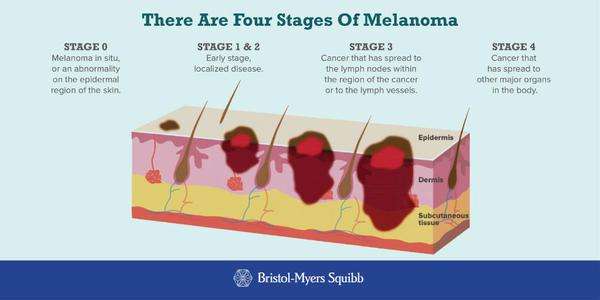
Melanoma stages are assigned using the TNM system.
The stage of the disease indicates how much the cancer has progressed by taking into account the size of the tumor, whether its spread to lymph nodes, and whether its spread to other parts of the body.
A doctor can identify a possible melanoma during a physical exam and confirm the diagnosis with a biopsy, where the tissue is removed to determine if its cancerous.
But more sophisticated technology, such as PET scans and sentinel lymph node biopsies, are necessary to determine the cancers stage or how far its progressed.
There are five stages of melanoma. The first stage is called stage 0, or melanoma in situ. The last stage is called stage 4. Survival rates decrease with later stages of melanoma.
Its important to note that survival rates for each stage are just estimates. Each person with melanoma is different, and your outlook can vary based on a number of different factors.
How Can You Manage Stage 3 Melanoma
Managing stage 3 melanoma can be challenging. With technological and medical advances, this diagnosis may not be as severe as it once was.
After your surgery or if youre unable to undergo surgery, you may need adjuvant treatment to prevent the cancer from coming back. There is adjuvant radiation therapy and adjuvant immunotherapy. These therapies help reduce the risk of melanoma returning, but they dont increase your survival rate.
Clinical Staging And Pathologic Staging
To add to the complexity of staging, the cancer also may have a clinical stage and a pathologic stage.
Clinical staging takes place before surgery, based on blood tests, physical exams or imaging tests such as X-rays, a computed tomography scan, magnetic resonance imaging or positron emission tomography scans.
What doctors discover during surgery may provide more detailed information about the cancers size and spread. Often, some tissue from the surgery will be examined afterward to provide more clues. This process is known as pathologic staging, or surgical staging.
If surgery isnt possible, doctors will use the clinical stage when determining a treatment plan.
Also Check: What Foods Prevent Skin Cancer
Adjuvant Treatment May Represent The Best Opportunity To Cure Patients After Surgery And To Prevent Morbidity From Progression
Following surgery for melanoma with a high risk of relapse and death , melanoma patients currently have two treatment options approved by the US Food and Drug Administration: high-dose IFN- and pegylated IFN . The patterns of relapse in this population show that 51% of the relapses occur at distant sites , so treatment to delay relapse can be a significant benefit to patients, even if the therapy does not increase long-term overall survival . Curing patients in this population at high risk for relapse and death ideally would require the pretreatment ability to identify which patients are destined for relapse and, among those at highest risk, who will benefit from a particular adjuvant intervention which may relate to patient, tumor and therapy.
To answer the first question, years of work have been devoted to evaluating clinical and pathologic risk factors related to the primary melanoma, and the presence or absence of tumor in draining lymph nodes, which is the single most important determinant of survival. The current American Joint Committee on Cancer staging system recognizes the importance of ulceration of the primary tumor, mitotic rate, and the number and size of tumor bearing lymph nodes . Further refinement of this system is needed, because even with a full knowledge of all of these factors, many patients defined as high risk by AJCC criteria are likely cured by surgery and may be receiving adjuvant therapy for no benefit.
Five Types Of Standard Treatment Are Used:
Surgery
Surgery to remove thetumor is the primary treatment of all stages of melanoma. A wide local excision is used to remove the melanoma and some of the normal tissue around it. Skin grafting may be done to cover the wound caused by surgery.
Sometimes, it is important to know whether cancer has spread to the lymph nodes. Lymph node mapping and sentinel lymph node biopsy are done to check for cancer in the sentinel lymph node . It is the first lymph node the cancer is likely to spread to from the primary tumor. A radioactive substance and/or blue dye is injected near the tumor. The substance or dye flows through the lymphducts to the lymph nodes. The first lymph node to receive the substance or dye is removed. A pathologist views the tissue under a microscope to look for cancer cells. If cancer cells are found, more lymph nodes will be removed and tissue samples will be checked for signs of cancer. This is called a lymphadenectomy. Sometimes, a sentinel lymph node is found in more than one group of nodes.
After the doctor removes all the melanoma that can be seen at the time of the surgery, some patients may be given chemotherapy after surgery to kill any cancer cells that are left. Chemotherapy given after the surgery, to lower the risk that the cancer will come back, is called therapy.
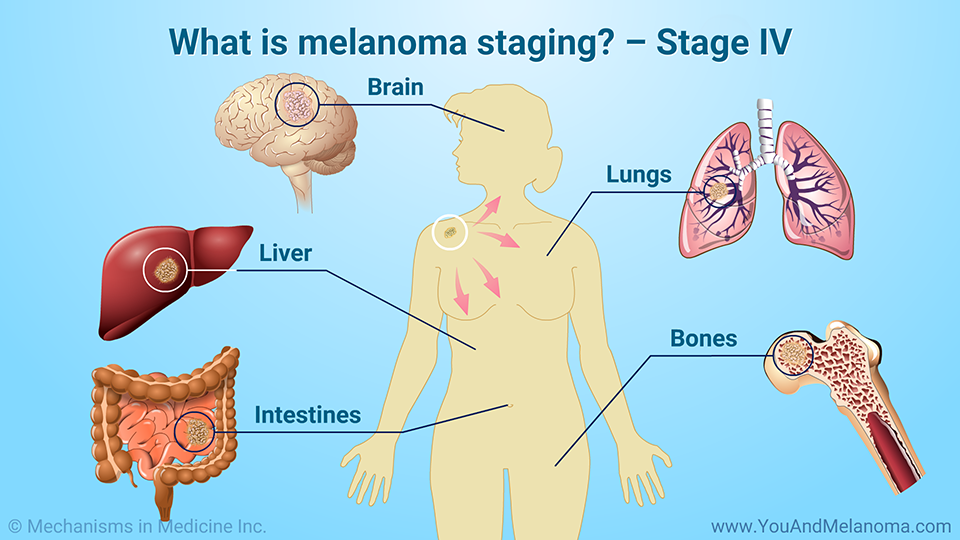
Surgery to remove cancer that has spread to the lymph nodes, lung, gastrointestinal tract, bone, or brain may be done to improve the patients quality of life by controlling symptoms.
Also Check: What Cancer Looks Like On Skin
Red Flag #: Swollen Lymph Nodes
If melanoma spreads, it often goes to the lymph nodes first, says Melinda L. Yushak, M.D., assistant professor of hematology and medical oncology at Emory University School of Medicine in Atlanta. The cancer cells will first travel to the nodes closest to the original tumor, she says. Lymph nodes are located throughout your entire body, but large clusters are found in the neck, underarms, chest, abdomen, and groin. If the cancer has made its way to the lymph nodes, it usually wont be painful, but theyll feel swollen or even hard to the touch, Dr. Zaba says.
Can Stage 3 Melanoma Be Cured
Of the three primary skin cancers, melanoma is the most malignant and resistant to treatment. Due to its dynamic development and the frequency of metastases, the therapy is extremely complicated and requires the participation of multidisciplinary specialists. The effectiveness of treating the disease is closely related to timely diagnosis. Can stage 3 melanoma be cured?
You May Like: When Is Skin Cancer Awareness Month
How To Protect Yourself
Here are the best ways to avoid melanoma recurrence:
To spot signs of melanoma, keep the ABCDE guidelines in mind:
- Asymmetry.
- Borders .
- Color .
Treatment Of Stage Ii Melanoma
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of stage II melanoma may include the following:
- Surgery to remove the tumor and some of the normal tissue around it. Sometimes lymph node mapping and sentinel lymph node biopsy are done to check for cancer in the lymph nodes at the same time as the surgery to remove the tumor. If cancer is found in the sentinel lymph node, more lymph nodes may be removed.
- A clinical trial of new types of treatment to be used after surgery.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Also Check: Can Basal Cell Carcinoma Cause Fatigue
Red Flag #: Bone Pain Or Fractures
The bones are considered a late-stage site of melanoma metastasestypically, it doesnt spread to the bones until its already spread to another area of the body first. Melanoma can cause pain in the bones where its spread, and some peoplethose with very little body fat covering their bonesmay be able to feel a lump or mass. Metastatic melanoma can also weaken the bones, making them fracture or break very easily. This is most common in the arms, legs, and spine. If you feel any sharp, sudden, or new pains that wont go away, talk to your doctor.
Treatment Of Stage Iii Melanoma That Can Be Removed By Surgery
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of stage III melanoma that can be removed by surgery may include the following:
- Surgery to remove the tumor and some of the normal tissue around it. Skin grafting may be done to cover the wound caused by surgery. Sometimes lymph node mapping and sentinel lymph node biopsy are done to check for cancer in the lymph nodes at the same time as the surgery to remove the tumor. If cancer is found in the sentinel lymph node, more lymph nodes may be removed.
- Surgery followed by immunotherapy with immune checkpoint inhibitors if there is a high risk that the cancer will come back.
- Surgery followed by targeted therapy with signal transduction inhibitors if there is a high risk that the cancer will come back.
- A clinical trial of immunotherapy with or without vaccine therapy.
- A clinical trial of surgery followed by therapies that target specific gene changes.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Read Also: What Is Papillary Thyroid Carcinoma
What Is Stage Iii Melanoma
Stage III melanomas are tumors that have spread to regional lymph nodes or have developed in-transit deposits of disease, but there is no evidence of distant metastasis. Stage III melanoma is regional melanoma, meaning it has spread beyond the primary tumor to the closest lymph nodes, but not to distant sites. There are four subgroups of Stage III melanoma: IIIA, IIIB, IIIC, IIID. Stage III is invasive melanoma.
- Subgroups are IIIA, IIIB, IIIC, IIID
- Stage III melanoma is defined by four primary characteristics
- Important distinction within Stage III: whether the spread to lymph nodes can be detected microscopically or macroscopically
- Microscopically, also called clinically occult = seen by pathologist during biopsy or dissection
- Macroscopically, also called clinically detected = seen by naked eye or felt by hand or seen on CT scans or ultrasound
- Risk: Intermediate to high for regional or distant spread
Biological Therapies And Melanoma
Biological therapies are treatments using substances made naturally by the body. Some of these treatments are called immunotherapy because they help the immune system fight the cancer, or they occur naturally as part of the immune system. There are many biological therapies being researched and trialled, which in the future may help treat people with melanoma. They include monoclonal antibodies and vaccine therapy.
Read Also: Is Skin Cancer Always Visible
Treating Stage 4 Melanoma
If melanoma comes back or spreads to other organs it’s called stage 4 melanoma.
In the past, cure from stage 4 melanoma was very rare but new treatments, such as immunotherapy and targeted treatments, show encouraging results.
Treatment for stage 4 melanoma is given in the hope that it can slow the cancer’s growth, reduce symptoms, and extend life expectancy.
You may be offered surgery to remove other melanomas that have grown away from the original site. You may also be able to have other treatments to help with your symptoms, such as radiotherapy and medicine.
If you have advanced melanoma, you may decide not to have treatment if it’s unlikely to significantly extend your life expectancy, or if you do not have symptoms that cause pain or discomfort.
It’s entirely your decision and your treatment team will respect it. If you decide not to receive treatment, pain relief and nursing care will be made available when you need it. This is called palliative care.
What Are The Signs Of Melanoma
Knowing how to spot melanoma is important because early melanomas are highly treatable. Melanoma can appear as moles, scaly patches, open sores or raised bumps.
Use the American Academy of Dermatology’s “ABCDE” memory device to learn the warning signs that a spot on your skin may be melanoma:
- Asymmetry: One half does not match the other half.
- Border: The edges are not smooth.
- Color: The color is mottled and uneven, with shades of brown, black, gray, red or white.
- Diameter: The spot is greater than the tip of a pencil eraser .
- Evolving: The spot is new or changing in size, shape or color.
Some melanomas don’t fit the ABCDE rule, so tell your doctor about any sores that won’t go away, unusual bumps or rashes or changes in your skin or in any existing moles.
Another tool to recognize melanoma is the ugly duckling sign. If one of your moles looks different from the others, its the ugly duckling and should be seen by a dermatologist.
Also Check: Where Does Skin Cancer Start
The Stage Of Melanoma Depends On The Thickness Of The Tumor Whether Cancer Has Spread To Lymph Nodes Or Other Parts Of The Body And Other Factors
To find out the stage of melanoma, the tumor is completely removed and nearby lymph nodes are checked for signs of cancer. The stage of the cancer is used to determine which treatment is best. Check with your doctor to find out which stage of cancer you have.
The stage of melanoma depends on the following:
- The thickness of the tumor. The thickness of the tumor is measured from the surface of the skin to the deepest part of the tumor.
- Whether there are:
- Satellite tumors: Small groups of tumor cells that have spread within 2 centimeters of the primary tumor.
- Microsatellite tumors: Small groups of tumor cells that have spread to an area right beside or below the primary tumor.
- In-transit metastases: Tumors that have spread to lymph vessels in the skin more than 2 centimeters away from the primary tumor, but not to the lymph nodes.
What Happens At Follow
The primary purpose of follow-up is to detect recurrences early.
The Australian and New Zealand Guidelines for the Management of Melanoma make the following recommendations for follow-up for patients with invasive melanoma.
- Self-skin examination
- Routine skin checks by a patient’s preferred health professional
- Follow-up intervals are preferably six-monthly for five years for patients with stage 1 disease, three-monthly or four-monthly for patients with stage 2 or 3 disease, and yearly after that for all patients.
- Individual patients needs should be considered before an appropriate follow-up is offered
- Provide education and support to help the patient adjust to their illness
The follow-up appointments may be undertaken by the patient’s general practitioner or specialist, or they may be shared.
Follow-up appointments may include:
- A check of the scar where the primary melanoma was removed
- A feel for the regional lymph nodes
In those with more advanced primary disease, follow-up may include:
- Blood tests, including LDH
- Imaging: ultrasound, X-ray, CT, MRI and PET scan.
Tests are not typically worthwhile for stage 1/2 melanoma patients unless there are signs or symptoms of disease recurrence or metastasis. And no tests are thought necessary for healthy patients who have remained well for five years or longer after removal of their melanoma, whatever stage.
Read Also: How Do You Know You Have Skin Cancer
Treatment Of Stage Iii Melanoma That Cannot Be Removed By Surgery Stage Iv Melanoma And Recurrent Melanoma
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of stage III melanoma that cannot be removed by surgery, stage IV melanoma, and recurrentmelanoma may include the following:
- Radiation therapy to the brain, spinal cord, or bone.
Treatments that are being studied in clinical trials for stage III melanoma that cannot be removed by surgery, stage IV melanoma, and recurrent melanoma include the following:
- Immunotherapy alone or in combination with other therapies such as targeted therapy.
- For melanoma that has spread to the brain, immunotherapy with nivolumab plus ipilimumab.
- Targeted therapy, such as signal transduction inhibitors, angiogenesis inhibitors, oncolytic virus therapy, or drugs that target certain genemutations. These may be given alone or in combination.
- Surgery to remove all known cancer.
- Systemic chemotherapy.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Braf & Mek Kinase Inhibitors
The BRAF and MEK genes are known to play a role in cell growth, and mutations of these genes are common in several types of cancer. Approximately half of all melanomas carry a specific BRAF mutation known as V600E. This mutation produces an abnormal version of the BRAF kinase that stimulates cancer growth. Some melanomas carry another mutation known as V600K. BRAF and MEK inhibitors block the activity of the V600E and V600K mutations respectively.
Don’t Miss: What Is Metastatic Urothelial Carcinoma