What’s My Risk Of Developing A New Primary Melanoma
As far as developing new cancers, it has been estimated that individuals with melanoma have a 9-fold increase in risk in developing new, primary melanomas, as well as a 28% overall increase in risk of developing a new primary cancer that isnt melanoma, also referred to as a second cancer. Specifically, individuals with melanoma are at a higher risk of developing second cancers in the prostate gland, breasts, salivary glands, kidneys, and thyroid glands, as well as a higher risk of developing leukemia and non-Hodgkin lymphoma.4
Factors that contribute to the development of a new primary melanoma include gender, genetics, age, and original melanoma location. For example, the younger an individual is at original diagnosis, the greater their risk is of developing a new melanoma. This could be due to a genetic tendency to developing melanomas, since melanoma diagnosed in individuals 30 years old or younger is often due to genetic factors. Also, women who have had an original melanoma on the head or neck region are at a higher risk of developing subsequent primary melanomas. Additionally, the risk of developing a new primary melanoma decreases each year after diagnosis and treatment, however, individuals with melanoma are a higher risk of developing a new melanoma than the general population for up to 20 years.4
A Dermatologist Can Tell You About Your Risks
If youre still wondering whether you should have genetic testing for melanoma, you may want to talk with your dermatologist. By talking about your concerns and risks, your dermatologist can help you decide whether this test would be helpful.
If genetic testing may be an option for you, your dermatologist can refer you to a qualified genetic counselor. A genetic counselor can talk with you about the benefits and limitations of testing.
1Swetter SM, Tsao H, et al. Guidelines of care for the management of primary cutaneous melanoma. J Am Acad Dermatol. 201. Articles in press.
ImagesGetty Images
ReferencesLeachman SA, Carucci J, et al. Selection criteria for genetic assessment of patients with familial melanoma. J Am Acad Dermatol. 2009 Oct;61:677e1-14.
National Comprehensive Cancer Network. NCCN Guidelines Melanoma. Last accessed March 27, 2017.
Ransohoff KJ, Jaju PD, et al. Familial skin cancer syndromes: Increased melanoma risk. J Am Acad Dermatol. 2016;74:423-34.
Swetter SM, Tsao H, et al. Guidelines of care for the management of primary cutaneous melanoma. J Am Acad Dermatol. 201. Articles in press.
Van Voorhees A. What should you know about hereditary melanoma? Dermatology World. 2016; 26:20-4.
Putative Genes For Basal Cell Carcinoma
BRCA1-associated protein 1
Pathogenic variants in the BAP1 gene are associated with an increased risk of a variety of cancers, including cutaneous melanoma and uveal melanoma. Although the BCC penetrance in individuals with pathogenic variants in BAP1 is not known, there are several BAP1 families that report diagnoses of BCC. In one study, pathogenic variant carriers from four families reported diagnoses of BCC. Tumor evaluation of BAP1 showed loss of BAP1 protein expression by immunohistochemistry in BCCs of two germline BAP1 pathogenic variant carriers but not in 53 sporadic BCCs. A second report noted that four individuals from families with BAP1 germline pathogenic variants were diagnosed with a total of 19 BCCs. Complete loss of BAP1 nuclear expression was observed in 17 of 19 BCCs from these individuals but none of 22 control BCC specimens. Loss of BAP1 nuclear expression was also reported in a series of 7 BCCs from individuals with loss of function BAP1 variants, but only in 1 of 31 sporadic BCCs.
Read Also: Can Melanoma Be Treated Successfully
How To Prevent Melanoma Skin Cancer
Though there are currently no effective treatments for melanoma skin cancer, it is possible to reduce your risk by taking precautions. These include wearing sunscreen and staying outdoors as little as possible during peak sun hours.
The best way to prevent Melanoma skin cancer is to make sure you get the right protection. Wear sunscreen daily , stay out of the sun during peak hours, and always look at your skin every day for new or unusual moles.
What Is Familial Malignant Melanoma
Familial malignant melanoma is a term usually referring to families in which 2 or more first-degree relatives, such as a parent, sibling, and/or child, have a type of skin cancer called melanoma. Cancer begins when healthy cells begin to change and grow, out of control forming a mass called a tumor. Overall, about 8% of people newly diagnosed with melanoma have a first-degree relative with melanoma. A much smaller percentage, about 1% to 2%, has 2 or more close relatives with melanoma.;
Individuals in melanoma-prone families frequently have moles called dysplastic nevi. Dysplastic nevi are large, flat, irregular, asymmetric, variably pigmented moles. They occur primarily on sun-exposed skin, but they also occur in areas that are not exposed to the sun. The moles must be monitored very carefully for any change in size, shape, and color to watch for cancer. In the United States, the average age when melanoma is diagnosed in people with familial melanoma is in the 30s; the average age when melanoma is diagnosed in the general population is in the 50s.
You May Like: Can Skin Cancer Be Cured With Cream
Table 6 Types Of Oculocutaneous Albinism
| African, African American, Native American | Yes | |
| Japanese, Italian, German | Yes | |
| Not in the United States | ||
| OCA Type 6 | Chinese, African, European, Indian | Yes |
| Faroe Islands, Denmark | Yes |
Other albinism syndromes
A subgroup of albinism includes people who exhibit a triad of albinism, prolonged bleeding time, and deposition of a ceroid substance in organs such as the lungs and gastrointestinal tract. This syndrome, known as Hermansky-Pudlak syndrome, is inherited in an autosomal recessive manner but may have a pseudodominant inheritance in Puerto Rican families, owing to the high prevalence in this population. The underlying cause is believed to be a defect in melanosome and lysosome transport. A number of pathogenic variants at disparate have been associated with this syndrome, including HPS1, HPS3, HPS4, HPS5, HPS6, HPS7 , HPS8 , and HPS9 . Pigmentation characteristics can vary significantly in this disorder, particularly among those with HPS1 pathogenic variants, and patients report darkening of the skin and hair as they age. In a small cohort of individuals with HPS1 variants, 3 out of 40 developed cutaneous SCCs, and an additional 3 had BCCs. Hermansky-Pudlak syndrome type 2, which includes increased susceptibility to infection resulting from neutropenia, has been attributed to defects in AP3B1.
Epidermolysis bullosa
Dystrophic epidermolysis bullosa
Epidermodysplasia verruciformis
Fanconi anemia
Risk Factors Biomarkers And Prevention Of Melanoma Of The Skin
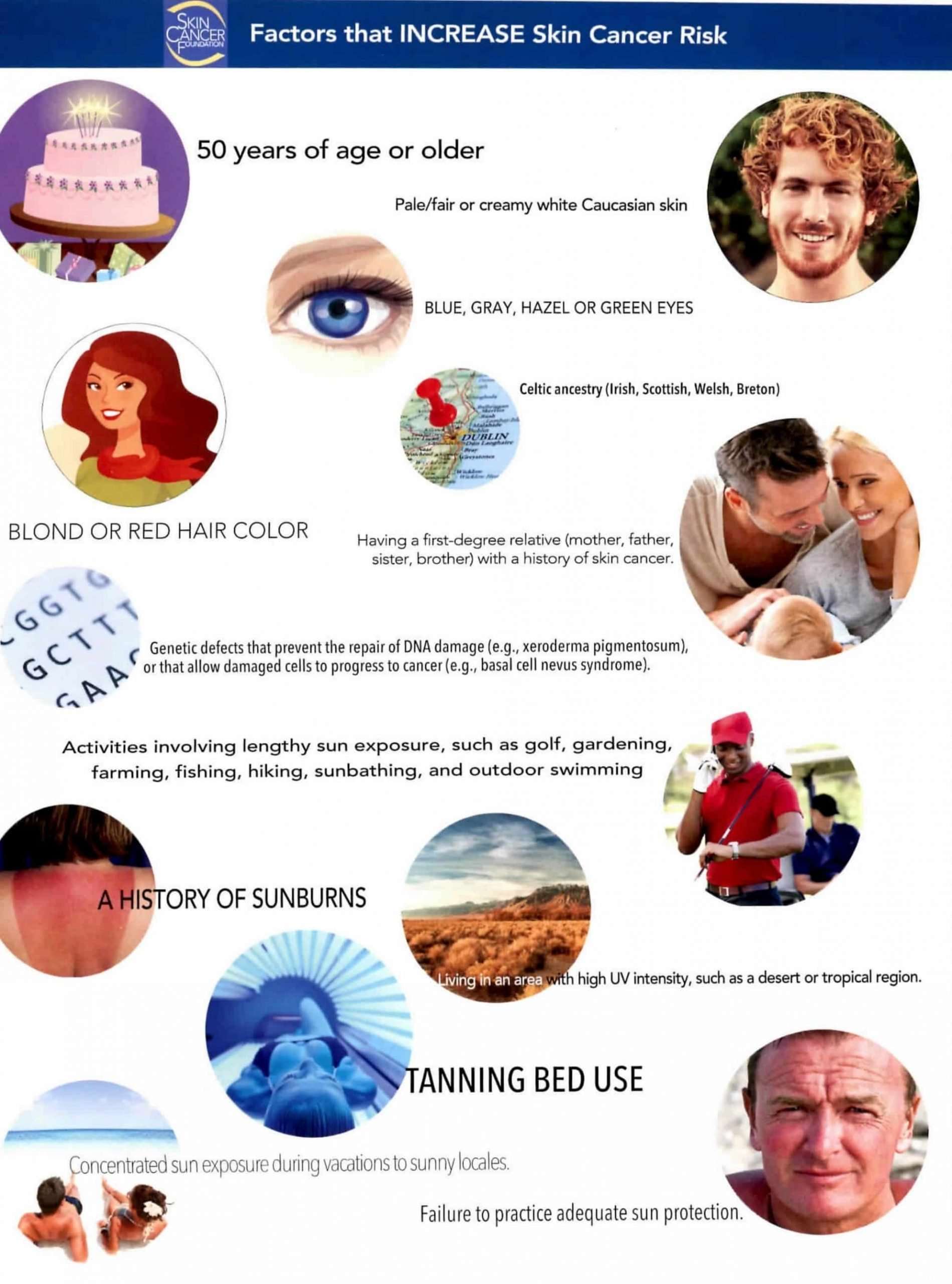
Melanoma of the skin is associated with multiple risk factors besides exposure to UV radiation and age, such as ethnicity , history of blistering sunburns at young age, dysplastic nevi, family history, occupational chemicals exposure , fair skin and hair and immunosuppression . A risk associated with male sex has been described, but postmenopausal women have shown different genetic patterns , which increase the risk of developing melanoma by 1.9 times . Nonetheless, melanoma of the skin can be prevented if the exposure to previous external factors, such as exposure to sun or tanning, is reduced. Several prevention campaigns and educational actions have been put in practice, but changes in behaviours are difficult to implement, even in younger adults . Although also common in younger persons , it is predicted that the incidence of melanoma in this group might stabilise or decrease in forthcoming years .
Read Also: Is Renal Cell Carcinoma Hereditary
How Common Is Familial Melanoma
Most cases of melanoma are sporadic, meaning it occurs by chance. The number of people who have an inherited risk of melanoma is unknown, but the number is thought to be low. It is estimated that about 8% of people with melanoma have a first-degree relative with melanoma and that 1% to 2% of people with melanoma have 2 or more close relatives with melanoma.
Integrated Care For Patients With Skin Cancer
The primary goal of optimal care is not only motivated by mortality reduction but also to provide a better quality of life and long-term management of side effects . As first addressed by Porter and Teisberg , a value-based healthcare approach aims at improving health outcomes and quality of services, measured against the cost spent by providing care to patients. Data collection and evaluation allow patients needs to become aligned with better and standardised treatment outcomes, reducing the impact of the burden caused by cancer . Thus, healthcare provided to cancer patients will be comparable between different institutions.
Several case studies illustrate the pathways for the creation of high-quality IPUs based on specialised, multidisciplinary care in oncology . The retrieved evidence on the best practice pathways for patient centricity and more effective medical care in these organisations is summarised in Table 1. IPUs must be comprised of multidisciplinary teams, scalability, provision for clinical and organisational innovation, greater research and focus on outcomes measures , as well as strong notions of pharmaco-epidemiology, time and costs spending. Overall, the primary goal must be value creation for patients. As described next, to achieve this goal and develop an IPU focused on treating skin cancer, Table 2 presents practical measures for patients with melanoma, considering their different dimensions.
Don’t Miss: What Are The Types Of Skin Cancer
Positive Genetic Test For Melanoma Can Provide Important Information
A genetic test for melanoma can tell you about more than your melanoma risk. People who carry a mutation on a gene known as CDKN2A have a higher risk of developing melanoma, cancer of the pancreas, or a tumor in the central nervous system.
A mutation on the gene called BAP1 means a higher risk of getting melanoma, melanoma of the eye, or cancers like mesothelioma and kidney cancer.
A genetic test cannot tell you whether will develop one of these cancers.
But knowing these risks can be helpful. It can help people get needed cancer screenings.
A positive test for melanoma can also help your dermatologist monitor you for signs of skin cancer. Patients with a high risk may need more frequent skin cancer screenings. Total body photography can show changes to your moles, which can help find a melanoma in its earliest stage.
A positive test also has some drawbacks. It causes some people to feel anxious and worried. Some people worry that an insurance company may discriminate against them.
Syndromes And Genes Associated With A Predisposition For Squamous Cell Carcinoma
Major genes have been defined elsewhere in this summary as genes that are necessary and sufficient for disease, with important pathogenic variants of the gene as causal. The disorders resulting from single-gene pathogenic variants within families lead to a very high risk of disease and are relatively rare. The influence of the environment on the development of disease in individuals with these single-gene disorders is often very difficult to determine because of the rarity of the genetic variant.
Identification of a strong environmental risk factorchronic exposure to UV radiationmakes it difficult to apply genetic causation for SCC of the skin. Although the risk of UV exposure is well known, quantifying its attributable risk to cancer development has proven challenging. In addition, ascertainment of cases of SCC of the skin is not always straightforward. Many registries and other epidemiologic studies do not fully assess the incidence of SCC of the skin owing to: the common practice of treating lesions suspicious for SCC without a diagnostic biopsy, and the relatively low potential for metastasis. Moreover, NMSC is routinely excluded from the major cancer registries such as the Surveillance, Epidemiology, and End Results registry.
With these considerations in mind, the discussion below will address genes associated with disorders that have an increased incidence of skin cancer.
Xeroderma pigmentosum
Multiple self-healing squamous epitheliomata
Oculocutaneous albinism
Don’t Miss: Are There Stages Of Basal Cell Carcinoma
What Is Melanoma Skin Cancer
Melanoma is a type of skin cancer that can occur when melanocytes, cells in the skin that produce the pigment melanin, are damaged. These damaged cells are then called moles. Melanoma arises when an overgrowth occurs on these moles. Melanoma is a type of skin cancer that can affect people of any age. Early detection and prevention are important parts of managing this disease. Here are some facts about melanoma: An estimated 558,000 new cases of melanoma were diagnosed in 2010.
Melanomas account for approximately 9% of skin cancer diagnoses in the United States each year. It is the most serious type of skin cancer because it appears as a mass on the skin.The overall incidence of melanoma is rising, but most cases are found in people over the age of 65.Not all moles are associated with skin cancer. Nearly 20% of people who have a mole on their skin do not have melanoma.
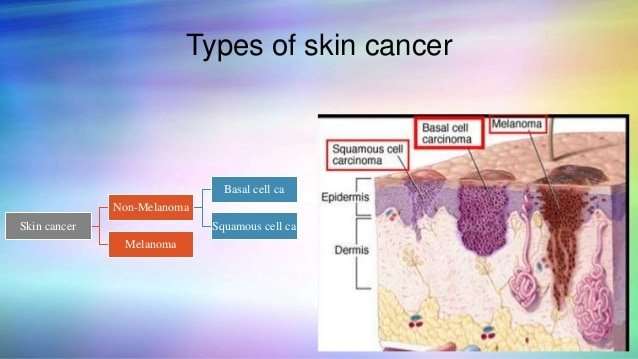
Structure Of The Skin
The genetics of skin cancer is an extremely broad topic. There are more than 100 types of tumors that are clinically apparent on the skin; many of these are known to have familial components, either in isolation or as part of a syndrome with other features. This is, in part, because the skin itself is a complex organ made up of multiple cell types. Furthermore, many of these cell types can undergo malignant transformation at various points in their differentiation, leading to tumors with distinct histology and dramatically different biological behaviors, such as squamous cell carcinoma and basal cell cancer . These have been called nonmelanoma skin cancers or keratinocyte cancers.
Figure 1 is a simple diagram of normal skin structure. It also indicates the major cell types that are normally found in each compartment. Broadly speaking, there are two large compartmentsthe avascular epidermis and the vascular dermiswith many cell types distributed in a connective tissue matrix, largely created by fibroblasts.
The true cytologic origin of BCC remains in question. BCC and basal cell keratinocytes share many histologic similarities, as is reflected in the name. Alternatively, the outer root sheath cells of the hair follicle have also been proposed as the cell of origin for BCC. This is suggested by the fact that BCCs occur predominantly on hair-bearing skin. BCCs rarely metastasize but can invade tissue locally or regionally, sometimes following along nerves.
Also Check: How Fast Does Melanoma Metastasis
Learn More About New Ways To Use Your Dna
Sequencing’s new;DNA Education Center;is your resource for;learning about DNA sequencing, personalized medicine, and genetic discoveries. For example, you can learn about the role of your genes in determining your risk of;medication side effects.
If you’re more interested in how DNA is used in pop culture,;The;Sequencing Blog;provides weekly insights. Our blog includes the latest trends and technological advancements that are integrating DNA into our daily lives including articles on how to use your DNA to personalize your beauty regimen, your lifestyle, and your health.
Table 2 Frequency Of Nonmalignant Findings In Basal Cell Nevus Syndrome
| Usually by age 10 y | |
| Keratogenic jaw cysts | Usually by age 20 y |
| Bridged sella | |
| Usually by age 40 y | |
| Macrocephaly | |
| Osseous lucencies in the hands | 30 |
| 3 | Congenital |
-
Adapted from a report by Kimonis et al. about 105 individuals with BCNS seen at the National Institutes of Health between 1985 and 1997.
Individuals with PTCH2 pathogenic variants may have a milder phenotype of BCNS than those with PTCH1 variants. Characteristic features such as palmar/plantar pits, macrocephaly, falx calcification, hypertelorism, and coarse face may be absent in these individuals.
A 9p22.3 microdeletion syndrome that includes the PTCH1 has been described in ten children. All patients had facial features typical of BCNS, including a broad forehead, but they had other features variably including craniosynostosis, hydrocephalus, macrosomia, and developmental delay. At the time of the report, none had basal cell skin cancer. On the basis of their hemizygosity of the PTCH1 gene, these patients are presumably at an increased risk of basal cell skin cancer.
Rare syndromes
Rombo syndrome
Bazex-Dupré-Christol syndrome
Epidermolysis bullosa simplex, Dowling-Meara
Characteristics of hereditary syndromes associated with a predisposition to BCC are described in below.
Read Also: What Is Melanoma In The Brain
Table 5 Hereditary Syndromes Associated With Squamous Cell Carcinoma Of The Skin
| DKC1 , TERC , TINF2 , NHP2/NOLA2 , NOP10/NOLA3 , TERT , WRAP53 , C16orf57 , RTEL1 | DKC1, TERC, TINF2, NHP2, NOP10, TERT | maintenance and trafficking |
| FANCA , FANCB , FANCC , FANCD1/BRCA2 , FANCD2 , FANCE , FANCF , FANCG/XRCC9 , FANCI , FANCJ/BRIP1/BACH1OMIM), FANCL , FANCM , FANCN/PALB2 , FANCO/RAD51C , FANCP/SLX4/BTBD12 , FANCQ/ERCC4/XPF , FANCS/BRCA1 | Chromosomal breakage testing; BRIP1, FANCA, FANCC, FANCE, FANCF, FANCG, PALB2, BRCA1, BRCA2, ERCC4, RAD51C, SLX4 | |
| MYO5A , RAB27A , MLPH | RAB27A | |
| HPS1 , HPS3 , HPS4 , HPS5 , HPS6 , HPS7/DTNBP1 , HPS8/BLOC1S3 | HPS1, HPS3, HPS4, HPS7 | |
| LAMA3 , LAMB3 , LAMC2 , COL17A1 | LAMA3, LAMB3, LAMC2, COL17A1 | |
| No | Growth factor signaling | |
| TYR , OCA2 , TYRP1 , SLC45A2/MATP/OCA4 , Locus 4q24, SLC24A5 , C10Orf11 | TYR, OCA2, TYRP1 | |
| No | Chromosomal stability | |
| XPA , XPB/ERCC3 , XPC , XPD/ERCC2 , XPE/DDB2 , XPF/ERCC4 , XPG/ERCC5 | XPA, XPC |
-
aFor more information on genetic testing laboratories, refer to the NIH Genetic Testing Registry.
Xeroderma pigmentosum
Xeroderma pigmentosum is a hereditary disorder of excision repair that results in cutaneous malignancies in the first decade of life. individuals have an increased sensitivity to sunlight, resulting in a markedly increased risk of SCCs, BCCs, and melanomas. One report found that NMSC was increased 150-fold in individuals with XP; for those younger than 20 years, the prevalence has been estimated to be 5,000 to 10,000 times what would be expected in the general population.
Oculocutaneous albinism
Ive Heard Of People Who Never Sunbathe Dying Of Melanoma Isnt Sun Prevention Futile
- Melanoma, like many other diseases, has some genetic components. There is variability in how susceptible we may be to certain conditions. Individuals with a family history of melanoma, for example, are at a higher risk of developing this cancer compared to the average person.
- Sun exposure is the most significant environmental factor known to us in causing melanoma. Note that this does not mean that all sunbathers will get melanoma or that people who dont sunbathe as often will never get melanoma. It is, however, a meaningful statistic.
- Choosing not to exercise sun protection in the face of mounting evidence about the dangers of sun exposure is equivalent to arguing that smoking may not be bad because some smokers live until old age.
- We also need to admit that we cant ever truly purport to understand every detail when it comes to disease causes; there will always be an element of chance.
- Sun protection is not futile. It is the most critical environmental factor relating to all skin cancers including melanoma. Overexposure to the sun will also promote symptoms of premature aging such as wrinkling, mottled skin, and pigmentation problems.
Don’t Miss: What Are The Early Stages Of Melanoma