Papillary Carcinoma And Its Variants
Papillary thyroid carcinoma is the most common malignancy in the thyroid, representing up to 80% of all thyroid carcinomas. Tumors are classified by size as either less than 1 cm or more than 1 cm . There are many histologic variants of papillary carcinoma .
Several distinct molecular mutational events have been identified in PTC, including translocations or intrachromosomal rearrangements between the RET proto-oncogene and various partner genes. The most common partner genes are H4 and ELE1 . These translocations, and particularly RET/PTC3, are more common in radiation-induced tumors.
Another often-identified mutation is in the BRAF gene; this mutation occurs in between 40% and 60% of sporadic PTCs. BRAF mutations were originally designated as V599E, but this was corrected to V600E after discovery of a counting error in the original nucleic acid sequence. The mutation is a thymidine to adenine transition at codon 600 . BRAF mutations are most often found in conventional and tall cell variants and are uncommon in the follicular variant of papillary carcinoma. The RET/PTC translocations and the BRAF mutation are mutually exclusive and together may account for up to 70% of PTCs. The molecular mechanism behind the etiology of the remainder of conventional PTCs remains unclear.
A. Fischer, in, 2014
How Does Esophageal Cancer Form
We know that esophageal adenocarcinoma is linked to a condition called Barretts Esophagus, which is caused by gastroesophageal reflux disease .; People with Barretts Esophagus are much more likely to develop esophageal adenocarcinoma than people without it, with some studies showing 25 times higher risk.
Esophageal squamous cell carcinoma is often linked to smoking and drinking alcohol.
Who Gets Thyroid Cancer
About 2900 people are diagnosed with thyroid cancer each year in Australia. Thyroid cancer can occur at any age. It affects almost three times as many women as men it is the seventh most common cancer affecting Australian women of all ages, and the most common cancer diagnosed in women aged 2024.
Diagnoses of thyroid cancer in Australia have increased in recent years, with almost four times as many cases estimated in 2019 as there were in 1982. Some of this increase is due to the improved quality and greater use of diagnostic scans, such as ultrasounds. This has led to the detection of smaller, often insignificant, thyroid cancers that would otherwise not have been found. Researchers are trying to work out if there are any other causes of the increased rates of thyroid cancer.
Read Also: How Long For Armour Thyroid To Leave System
Read Also: How To Treat Melanoma In Nails
Causes Of Thyroid Cancer
Thyroid cancer happens when there’s a change to the DNA inside thyroid cells;which causes them to grow uncontrollably and produce a lump.
It’s not usually clear what causes this change, but there are a number of things that can increase your risk.
These include:
- other thyroid conditions, such as;an inflamed thyroid or goitre; but not;an overactive thyroid or underactive thyroid
- a family history of thyroid cancer;;your risk is higher if a close relative has had thyroid cancer
- radiation;exposure in childhood;;such as;radiotherapy
- a bowel condition called;familial adenomatous polyposis
- acromegaly; a rare condition where the body produces too much growth hormone
How Does Exposure To Radiation Increase The Risk Of Thyroid Cancer
The effects of radiation exposure depend on the amount of radiation and the age at which a person is exposed: the higher the dose of radiation and the younger the age of exposure, the greater the risk of getting thyroid cancer. ;Exposure during childhood raises the greatest risk.
Most exposure to radiation comes from medical treatments or from the environment .
The amount of radiation in routine medical tests like mammograms, x-rays and CT scans is low and not thought to significantly raise the risk of getting thyroid cancer. ;Still, lead aprons may be used to cover the neck as a precaution, and radiation tests should only be used on children when absolutely necessary. ;
Also Check: What Are The Early Stages Of Melanoma
How Is Papillary Thyroid Carcinoma Diagnosed
Your caregiver will ask you about your health history. This includes information on what signs and symptoms you have, and when they started. You may also be asked about your family’s health. Your caregiver will look and feel for lumps or other signs of problems on your neck. You may also need any of the following tests:
Who Might Have Thyroid Cancer
Women are three times more likely than men to get thyroid cancer. The disease is commonly diagnosed in women in their 40s and 50s, and men in their 60s and 70s. Even children can develop the disease. Risk factors include:
- Exposure to radioactive fallout from nuclear weapons or a power plant accident.
Don’t Miss: How Often Does Melanoma Spread To Lymph Nodes
Papillary Thyroid Cancer: Who Gets It
Papillary thyroid cancer can occur in people of all ages from early childhood to advanced ages although it is most common in people between age 30 and 50. Papillary thyroid cancer affects women more commonly than men, and it is most common in young women. Thyroid cancer is now the fifth most common malignancy among women in the United States. Since it can occur at any age, everybody should be aware of any changes in their thyroid gland and make sure their doctor feels the thyroid gland when getting a routine check-up. For more details on who gets papillary thyroid cancer, the increasing incidence, and ages of patients affected, go to our page on the Incidence of Papillary Thyroid Cancer.
What Is Papillary Renal Cell Carcinoma
Papillary renal cell carcinoma, or PRCC, is a type of kidney cancer. The kidneys work by removing waste products from the blood. Papillary renal cell carcinoma is a cancer of the tubes that filter those waste products from the blood. There are two types of papillary renal cell carcinoma. Type 1 is more common and grows slowly. Type 2 is more aggressive and grows more quickly.;
Read Also: What Does Early Squamous Skin Cancer Look Like
Thyroid Cancer Is A Disease In Which Malignant Cells Form In The Tissues Of The Thyroid Gland
The thyroid is a gland at the base of the throat near the trachea . It is shaped like a butterfly, with a right lobe and a left lobe. The isthmus, a thin piece of tissue, connects the two lobes. A healthy thyroid is a little larger than a quarter. It usually cannot be felt through the skin.
The thyroid uses iodine, a mineral found in some foods and in iodized salt, to help make several hormones. Thyroid hormones do the following:
- Control heart rate, body temperature, and how quickly food is changed into energy .
- Control the amount of calcium in the blood.
Does Prcc Run In Families
PRCC usually occurs randomly, which is called sporadic papillary renal cell carcinoma.
PRCC can also run in families, but this is rare. One form of PRCC that runs in families is called hereditary papillary renal cell carcinoma. Hereditary papillary renal cell carcinoma usually has a mutation in a part of the chromosomes called the MET gene.;
Another form of PRCC that runs in families is called Hereditary Leiomyomatosis and Renal Cell Carcinoma . This is characterized by alterations in a gene called fumarate hydratase. Patients or affected relatives with this condition may also have skin tumors called leiomyomas and uterine fibroids, which usually happen at a young age.
Read Also: What Does Stage 3b Melanoma Mean
Enhancing Healthcare Team Outcomes
Papillary thyroid cancer is ideally managed;by an interprofessional team that consists of an endocrinologist, general surgeon, oncologist, radiation oncologist, nuclear medicine physician, internist, pharmacists, and specialty care nurses. The majority of patients present to the primary provider or nurse practitioner with a painless mass in the neck. Once the FNA is performed, the patient should be referred to an oncologist and a surgeon. Patients need to know that the sole treatment for PTC is surgery. Patients treated with radioactive iodine need to be educated about this therapy and warned about the potential adverse effects. Following surgery, the patient requires long term monitoring for recurrence. Most patients require long term thyroid hormone replacement. Specialty care nurses in oncology assist with treatment, monitor and educate patients, and provide updates to the team. ;
With early diagnosis and prompt treatment, the prognosis for most patients is excellent.
How Will My Doctor Test For It
You’ll need a few different tests to see if a nodule is cancer.
Physical exam. Your doctor will feel for unusual growths in your neck and ask about any symptoms you might have.
Blood tests. You may get your thyroid hormone levels checked. This won’t tell you if you have cancer, but it gives more information about how your thyroid is working.
Ultrasound. You’ll get this test, which uses sound waves to make a picture of things inside your body, to learn more about nodules you have. Your doctor will find out about their shape, size, and other features. That will give important clues to decide how much of a problem they are.
Biopsy. Your doctor will use a very fine needle to take a sample of the nodule to test for cancer. Typically, the most you’ll feel during it is a small pinch.
You’ll likely get this done for any nodule that’s bigger than 1 centimeter . Nodules with calcium buildup, lots of blood vessels, or without clear borders raise red flags. So do unusual-looking nearby lymph nodes — bean-shaped organs that help fight infections.
You May Like: What Is Soft Tissue Carcinoma
Variants Of Papillary Thyroid Carcinoma
Return to:;Papillary Thyroid Carcinoma
Overview
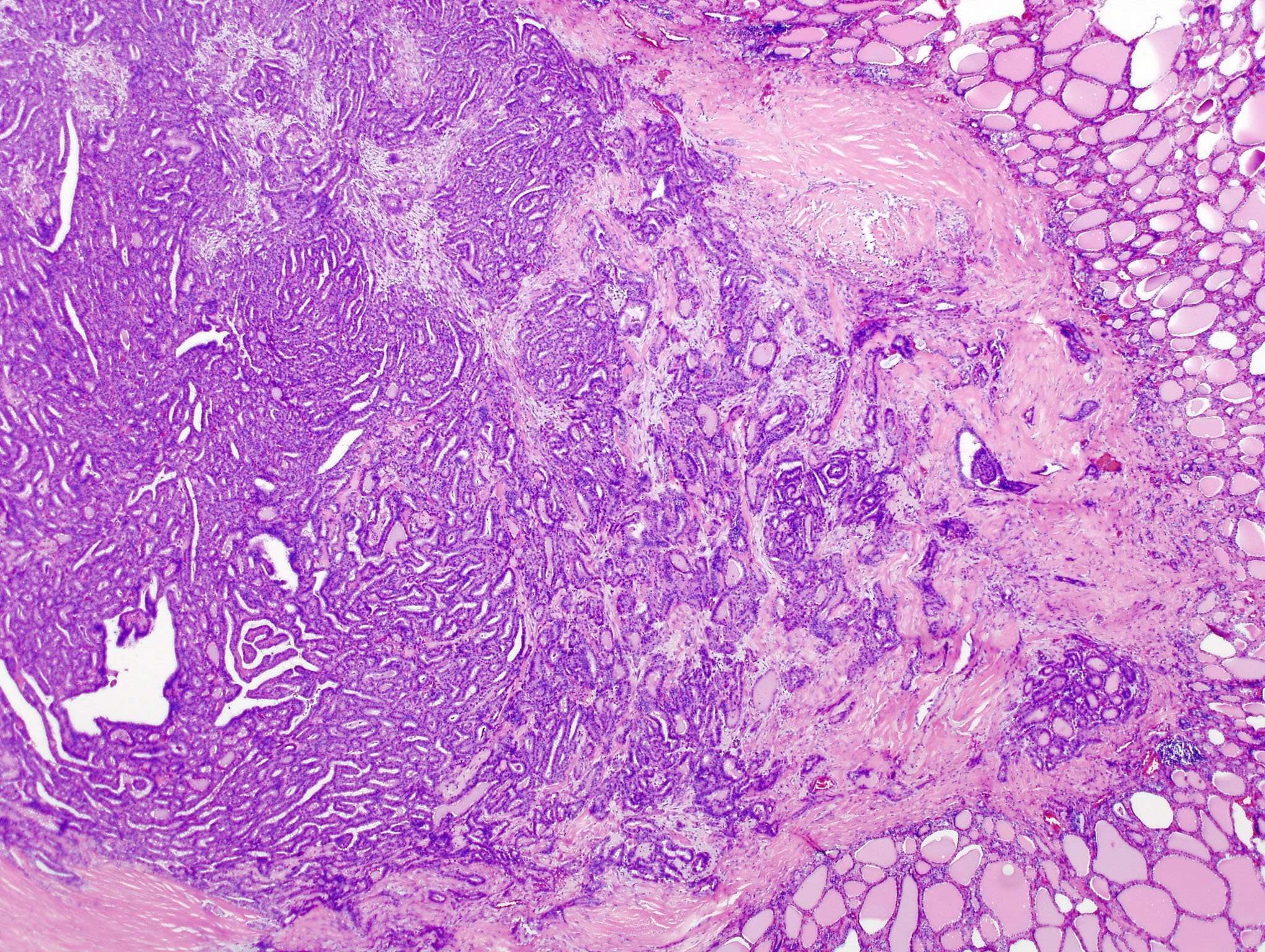
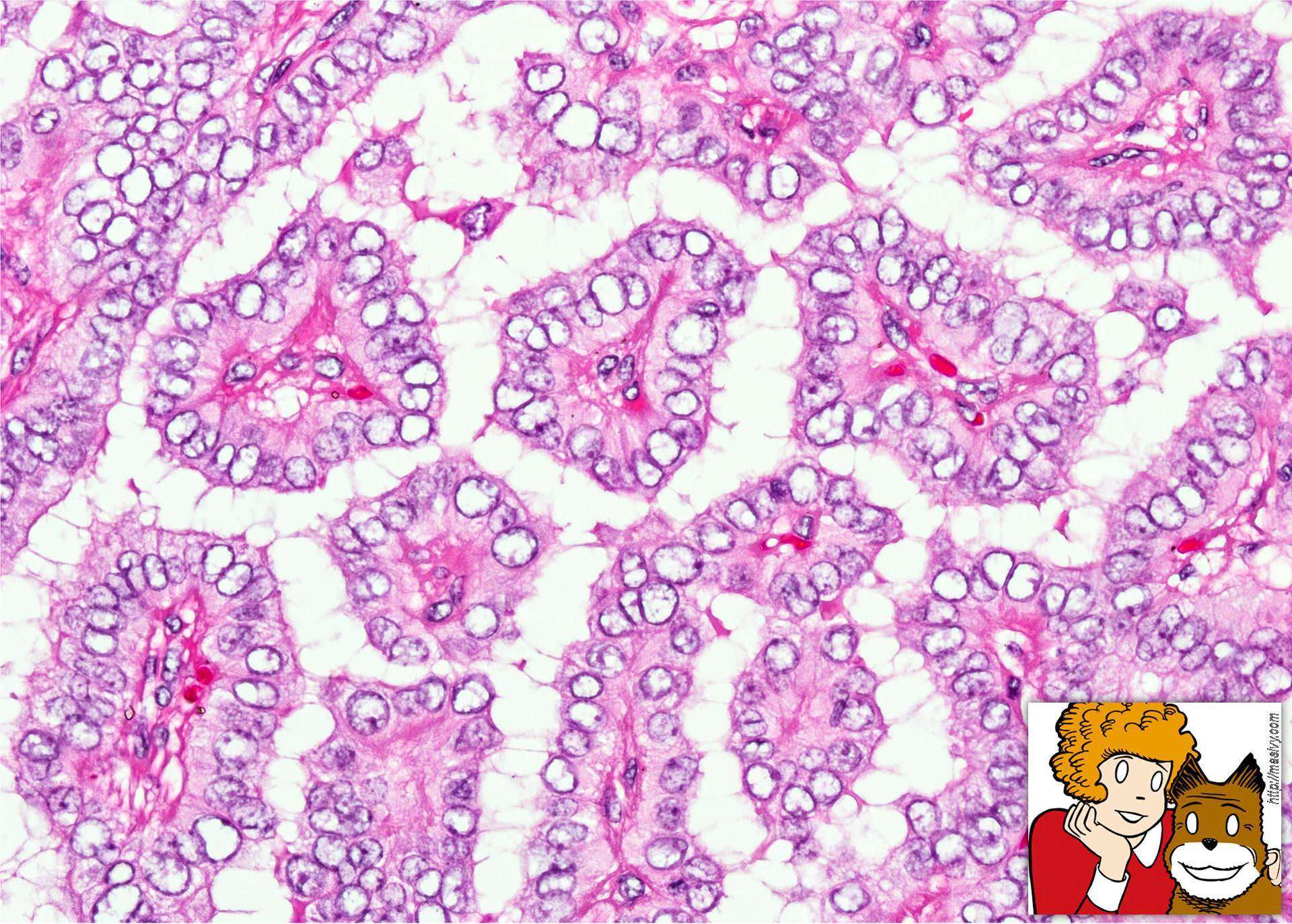
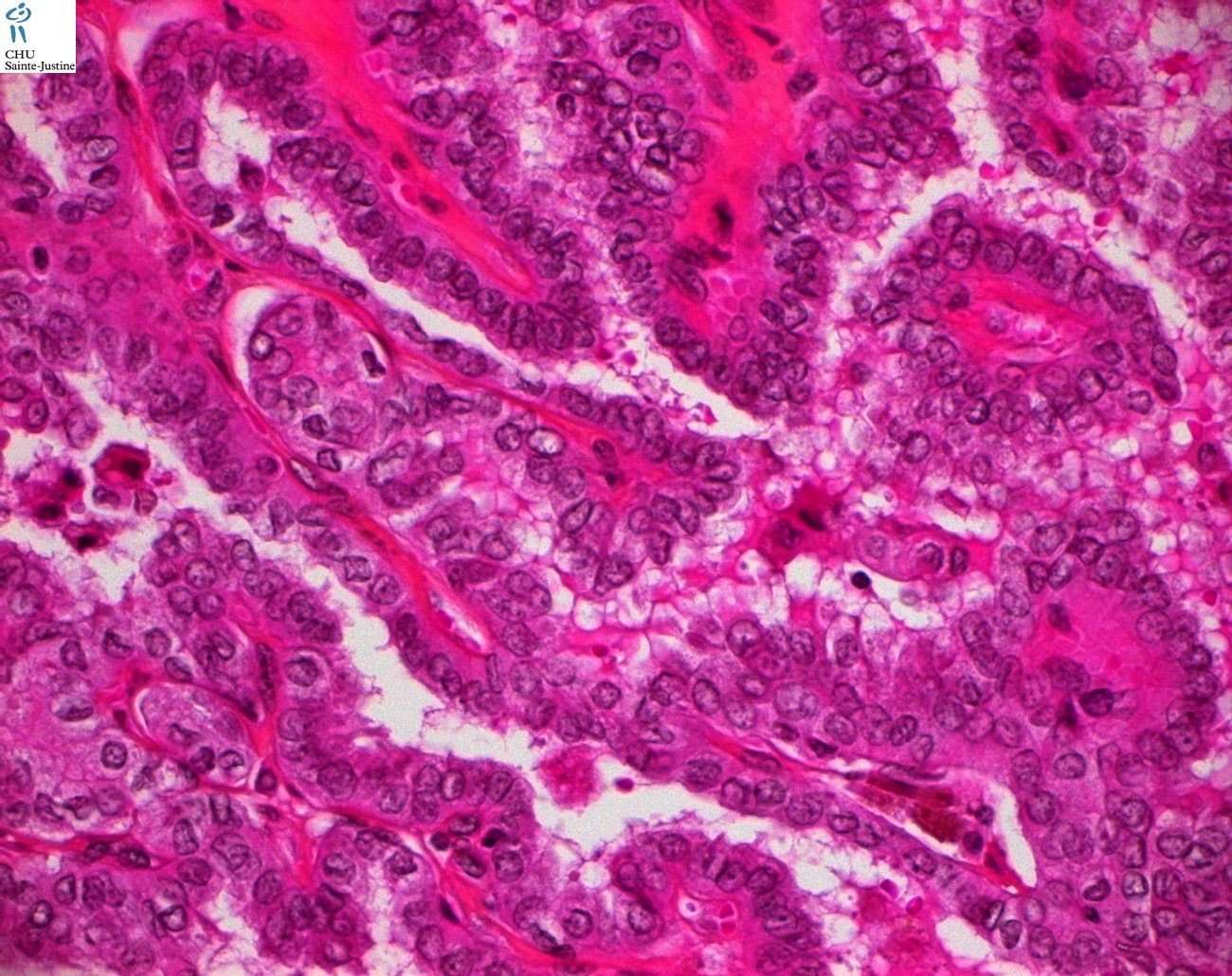
Papillary thyroid carcinoma is the most common malignancy of the thyroid, contributing to over 70% of thyroid cancers.1 These tumors are diagnosed using characteristic nuclear morphology; however, within the classification of “papillary thyroid carcinoma,” there exist several distinct architectural and cytologic subtypes. About;50% of PTC are of the classical subtype, while the other 50% are made up of less common histologic variants.10 Conventional, or classical, papillary thyroid carcinoma , seen below,;is characterized by papillary architecture with fibrovascular cores and psammoma bodies ;and tumor cells containing enlarged, overlapping;nuclei ;with nuclear clearing and nuclear grooves and nuclear membrane irregularities;. While papillary thyroid carcinoma tends to have an excellent prognosis, certain histologic variants have been shown to have more aggressive clinical courses. As such, determining the microscopic subtype of a papillary thyroid cancer is an important step in determining prognosis. Described below are the presentation, pathologic features, and prognostic indications of several of the more common variants of papillary thyroid carcinoma1-4.
Papillary thyroid microcarcinoma
Tall Cell Variant
Columnar Cell Variant
Follicular Variant
How Is Papillary Thyroid Carcinoma Treated
Your treatment will be based on what stage your cancer is in. In most cases, you will need surgery to remove your whole thyroid gland. Lymph nodes may also be removed. In some cases, a part of the thyroid gland may be left in place. Surgery is done to prevent cancer cells from spreading to other body organs. Ask your caregiver for more information about thyroid surgery. You may also need one or more of the following after your surgery:
- Gene therapy: Cancer gene therapy is a procedure that puts normal or changed genes into the cells of your body. This is to replace bad or damaged genes in the treatment of genetic disorders. Ask your caregiver for more information about this treatment.
- Medicines:
- Radioactive iodine: This medicine damages cells in your thyroid gland, decreasing the amount of thyroid hormone in your blood. This may help your body work better. After taking radioactive iodine, your thyroid gland may still make too much or not enough hormone. If this happens, you may still need to take thyroid medicine.
- Thyroid medicine: You are given this medicine to bring your thyroid hormone level back to normal.
Also Check: How Does Skin Cancer Feel
Treatment Of Advanced Thyroid Cancer
Thyroid cancer that spreads outside the neck area is rare, but can be a serious problem. Surgery and radioactive iodine remain the best way to treat such cancers as long as these treatments continue to work. However, for more advanced cancers, or when radioactive iodine therapy is no longer effective, other forms of treatment are needed. External beam radiation directs precisely focused X-rays to areas that need to be treatedoften tumor that has recurred locally or spread to bones or other organs. This can kill or slow the growth of those tumors. Cancer that has spread more widely requires additional treatment.
New chemotherapy agents that have shown promise treating other advanced cancers are becoming more widely available for treatment of thyroid cancer. These drugs rarely cure advanced cancers that have spread widely throughout the body but they can slow down or partially reverse the growth of the cancer. These treatments are usually given by an oncologist and often require care at a regional or university medical center.
What Are The Types Of Thyroid Cancer
Thyroid cancer is classified based on the type of cells from which the cancer grows. Thyroid cancer types include:
- Papillary: Up to 80% of all thyroid cancers are papillary. This cancer type grows slowly. Although papillary thyroid cancer often spreads to lymph nodes in the neck, the disease responds very well to treatment. Papillary thyroid cancer is highly curable and rarely fatal.
- Follicular: Follicular thyroid cancer accounts for up to 15% of thyroid cancer diagnoses. This cancer is more likely to spread to bones and organs, like the lungs. Metastatic cancer can be more challenging to treat.
- Medullary: About 2% of thyroid cancers are medullary. A quarter of people with medullary thyroid cancer have a family history of the disease. A faulty gene may be to blame.
- Anaplastic: This aggressive thyroid cancer is the hardest type to treat. It can grow quickly and often spreads into surrounding tissue and other parts of the body. This rare cancer type accounts for about 2% of thyroid cancer diagnoses.
Don’t Miss: How Can Skin Cancer Kill You
What Are The Symptoms
Often, you won’t have any. You might only find out about it because of an imaging test for another problem. Or, during a routine physical, your doctor might just happen to feel a lump, called a nodule, on your thyroid.
Nodules are growths that may be solid or filled with fluid. They’re very common and often don’t cause any trouble. But about 1 in 20 are cancer.
As a nodule gets bigger, you may start to have symptoms like:
- Lump in your neck that you can see or feel
- Hard time swallowing
- Sore throat or hoarseness that doesn’t go away
- Swollen lymph nodes in your neck
- Trouble breathing, especially when you lie down
What Is The Thyroid Gland
Your thyroid gland is one of many glands that make up your endocrine system. Endocrine glands release hormones that control different bodily functions.
The pituitary gland in your brain controls your thyroid gland and other endocrine glands. It releases thyroid-stimulating hormone . As the name suggests, TSH stimulates your thyroid gland to produce thyroid hormone.
Your thyroid needs iodine, a mineral, to make these hormones. Iodine-rich foods include cod, tuna, dairy products, whole-grain bread and iodized salt.
Recommended Reading: What Causes Renal Cell Carcinoma Cancer
What Is Thyroid Cancer
Thyroid cancer is a malignant tumour that starts in the cells of the thyroid. Malignant means that it can invade, or grow into, and destroy nearby tissue. It can also spread, or metastasize, to other parts of the body.
The thyroid is part of the endocrine system. It is a small gland in the front of the neck below the larynx and near the trachea . It has a right and left lobe, one on each side of the trachea. The lobes are joined by a thin piece of tissue called the isthmus.
The thyroid is mainly made up of follicular cells and C cells. Follicular cells make thyroid hormones. These hormones help break down food into energy. They also help control body functions such as body temperature, heart rate and breathing. C cells make the hormone calcitonin, which helps control the level of calcium in the blood.
Cells in the thyroid sometimes change and no longer grow or behave normally. These changes may lead to non-cancerous, or benign, conditions such as hypothyroidism, hyperthyroidism, thyroid nodules, thyroiditis or goitre.
In some cases, changes to thyroid cells can cause cancer. The most common types of thyroid cancer are papillary carcinoma and follicular carcinoma. They are usually grouped together as differentiated thyroid cancer, which makes up more than 90% of all thyroid cancers.
Thyroid Nodules Are Common But Usually Are Not Cancer
Your doctor may find a lump in your thyroid during a routine medical exam. A thyroid nodule is an abnormal growth of thyroid cells in the thyroid. Nodules may be solid or fluid-filled.
When a thyroid nodule is found, an ultrasound of the thyroid and a fine-needle aspiration biopsy are often done to check for signs of cancer. Blood tests to check thyroid hormone levels and for antithyroid antibodies in the blood may also be done to check for other types of thyroid disease.
Thyroid nodules usually don’t cause symptoms or need treatment. Sometimes the thyroid nodules become large enough that it is hard to swallow or breathe and more tests and treatment are needed. Only a small number of thyroid nodules are diagnosed as cancer.
Don’t Miss: How Fast Does Melanoma Metastasis
What Is Multiple Endocrine Neoplasia Type 2 And Where Does It Come From
MEN2 is a disorder that arises when a family carries changes in the RET gene. Many people with MEN2 will develop MTC. In addition to causing MTC, MEN2 can cause problems in other parts of the body such as the adrenal gland and bones.
There are two types of MEN2:
;People with MEN2A have a high chance of developing MTC as well as tumors of the adrenal and parathyroid glands. As a result, side effects of MEN2A can include high blood pressure and kidney stones. It is also known as MEN2A syndrome, multiple endocrine adenomatosis type 2A, multiple endocrine neoplasia type 2A syndrome, and Sipple syndrome.
Nearly all people with MEN2B will develop MTC. It will also predispose you to tumors of the adrenal gland but not of the parathyroid gland. Often times, MTC will develop at a very early age in people with MEN2B. People with MEN2B also develop abnormal growth of nerve tissue in the mouth or GI tract. In some cases, it may lead to a Marfanoid habitus. It is also known as MEN2B syndrome, multiple endocrine adenomatosis type 2B, and multiple endocrine neoplasia type 2B syndrome.
Read Also: Do Benign Thyroid Nodules Turn Cancerous