Basal Cell Carcinoma Recurrence
Recommended follow-up. After treatment for basal cell carcinoma , national guidelines recommend having a complete skin examination by your dermatologist every 6 to 12 months for the first 5 years.3 Recurrence may occur more than 5 years after treatment, too. Therefore, the guidelines call for yearly skin examinations for the rest of your life. Ask your doctor what she or he recommends for you.
Can Metastasis Be Prevented
Melanoma can spread âsilently,â meaning that you may not experience any symptoms of metastasis. Therefore, if youâve been treated for early-stage melanoma in the past, it is extremely important to perform regular self-examinations of your skin and lymph nodes, to keep all your appointments for checkups, and practice sun safety. There is nothing else an individual can do to prevent metastasis from being very diligent.
Catching a recurrence early greatly increases your chances of successful treatment. If the melanoma does spread, it is important to remain positive: remember that while the average prognosis is poor, some people do survive stage IV melanoma.
Skin Cancer Doctor Discussion Guide
Get our printable guide for your next doctorâs appointment to help you ask the right questions.
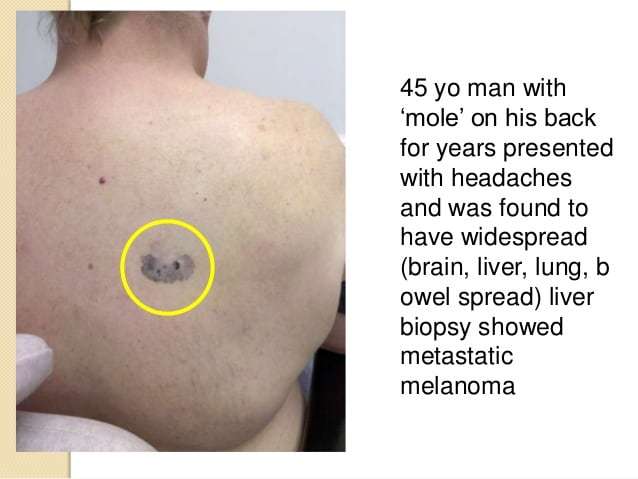
What Are The Signs Of Symptoms Of Metastatic Melanoma
Signs and symptoms depend upon the site of metastasis and the amount of tumor there. Metastases to the brain may first appear as headaches, unusual numbness in the arms and legs, or seizures. Spread to the liver may be first identified by abnormal blood tests of liver function long before the patient has jaundice, a swollen liver, or any other signs of liver failure. Spread to the kidneys may cause pain and blood in the urine. Spread to the lungs may cause shortness of breath, other trouble breathing, chest pain, and continued cough. Spread to bones may cause bone pain or broken bones called pathologic fractures. A very high tumor burden may lead to fatigue, weight loss, weakness and, in rare cases, the release of so much melanin into the circulation that the patient may develop brown or black urine and have their skin turn a diffuse slate-gray color. The appearance of multiple blue-gray nodules in the skin of a melanoma patient may indicate widespread melanoma metastases to remote skin sites.
Don’t Miss: Can You Die From Basal Cell Skin Cancer
Treatment Options For Recurrent Scc
A recurrent skin tumor is treated the same way as a high-risk primary tumor.4 Mohs surgery is the preferred option. Wide excision, radiation therapy, and chemotherapy are alternatives. Your doctor may recommend adjuvant therapy with radiation therapy or additional surgery.
If the cancer recurs in the lymph nodes or distant organs, treatment options include surgery, radiation therapy, and chemotherapy. Treatment options for advanced SCC are limited. Your doctor may recommend participating in a clinical trial.
Medically Reviewed By Dr Ch Weaver Md 8/2020
Since 2011 several new, precision cancer medicines and immunotherapies have completed evaluation in clinical trials and demonstrated improved outcomes for individuals with advanced melanoma leading to their approval by the FDA. Individuals with advanced melanoma now have numerous treatment options and additional clinical studies are ongoing in order to determine the best way to use these new drugs in various combinations.
Patients with recurrent or refractory metastatic melanoma may be divided into 2 groups: patients who have failed initial systemic therapy and experience progression or recurrence after an initial response to treatment or patients who have local recurrences after initial surgery or surgery and adjuvant therapy.
Individuals with metastatic melanoma who have failed initial systemic therapy are infrequently cured with additional therapy but can still experience prolonged survival with additional treatment. There are many choices of therapy and access to newer treatment strategies in clinical trials. These therapeutic choices may prolong survival, reduce symptoms of progressive cancer and/or offer the chance of cure. Patients need to assess the treatment options and consider their individual goals when electing to receive additional treatment.
You May Like: What Is Large Cell Carcinoma
Squamous Cell Carcinoma Recurrence
Recommended follow-up. After treatment for local squamous cell carcinoma , national guidelines recommend a complete skin examination by your dermatologist every 3 to 12 months for the first 2 years.4 The reason for this frequent follow-up schedule is that most SCC recurrences happen within 2 years.1 Follow-up should continue every 6 to 12 months for 3 more years. After that, the guidelines call for yearly skin examinations for the rest of your life.
You may need more frequent follow-up visits if the initial SCC had spread beyond the skin. Ask your doctor what she or he recommends for you.
Surgical Management Of Melanoma
The first-line or standard treatment for most melanomas is surgical excision. Thin tumors generally can be removed during an outpatient surgery, with a centimeter of normal appearing skin surrounding the melanoma. Surgery cures the majority of people with early stages of melanoma when they have early, thin tumors that have not spread from the original site.
Surgery for melanomas that are not very thin may require a wider excision of two centimeters of skin around the melanoma. This is usually performed as an outpatient procedure. Simple surgical procedures can still allow for a primary closure of most wounds, but occasionally, a skin graft or more complex reconstruction is required to close the wound. In cases where the melanoma is known to have spread to the lymph nodes, the lymph nodes may also need to be surgically removed.
During surgery, your doctor will remove the tumor along with an area of surrounding skin in order to lower the risk of a recurrence. How much skin is removed along with the tumor depends on the tumors thickness, which helps determine the stage of melanoma. Johns Hopkins surgical oncology faculty have led studies and chair international committees that have determined the following criteria for the margin of tissue removed during surgery and the classification of melanomas, depending on their size, into specific stages.
Don’t Miss: Can You Cure Stage 4 Melanoma
Other Features To Look Out For
Recurrence of melanoma usually grows rapidly.
The lesions are usually firm and hard. But dont ignore a bump if its soft.
Pink and brown are the going colors, but dont breathe a sigh of relief if new bumps are bluish, grey or black.
The skin lesions of a local recurrence may ulcerate or bleed, says Dr. Shah.
A metastatic recurrence of the in-transit metastatic type looks the same whether its three cm from the excision site or on a different body part.
What Is The Outlook For Patients With Nodular Melanoma
The risk of spread and ultimate death from invasive melanoma depends on several factors, but the main one is the measured thickness of the melanoma at the time it was surgically removed.
The Melanoma Guidelines report that metastases are rare for melanomas < 0.75mm and the risk for tumours 0.751 mm thick is about 5%. The risk steadily increases with thickness so that melanomas > 4 mm have a chance of metastasis of about 40%.
New Zealand statistics gathered by the Cancer Registry between 1994 and 2004 revealed 15,839 invasive melanomas. Of these, 52% were under 0.75 mm in thickness, 22% were between 0.76 and 1.49 mm, 15% were between 1.5 and 3 mm in thickness and 11% were more than 3 mm in thickness. Thicker tumours were slightly more likely to be diagnosed in males and more likely in older people than younger ones.
Read Also: Metastatic Basal Cell Carcinoma Survival Rate
Can I Lower My Risk Of The Melanoma Progressing Or Coming Back
If you have melanoma, you probably want to know if there are things you can do that might lower your risk of the cancer coming back, or of getting a new skin cancer.
At this time, not enough is known about melanoma to say for sure if there are things you can do that will be helpful. We do know that people who have had melanoma are at higher risk for developing another melanoma or other type of skin cancer. Because of this, its very important to limit your exposure to UV rays and to continue to examine your skin every month for signs of melanoma coming back or possible new skin cancers. Skin cancers that are found early are typically much easier to treat than those found at a later stage.
Adopting healthy behaviors such as not smoking, eating well, being active, and staying at a healthy weight might help as well, but no one knows for sure. However, we do know that these types of changes can have positive effects on your health that can extend beyond your risk of melanoma or other cancers.
Living As A Melanoma Skin Cancer Survivor
For many people with melanoma, treatment can remove or destroy the cancer. Completing treatment can be both stressful and exciting. You may be relieved to finish treatment, but find it hard not to worry about cancer growing or coming back. This is very common if youve had cancer.
For some people, the melanoma may never go away completely. These people may get regular treatment with immunotherapy, targeted therapy, chemotherapy, or other treatments to try to help keep the cancer under control for as long as possible. Learning to live with cancer that does not go away can be difficult and very stressful. It has its own type of uncertainty.
Read Also: Lobular Breast Cancer Stage 1
The Warning Signs Of Skin Cancer
Skin cancers â including melanoma, basal cell carcinoma, and squamous cell carcinoma â often start as changes to your skin. They can be new growths or precancerous lesions â changes that are not cancer but could become cancer over time. An estimated 40% to 50% of fair-skinned people who live to be 65 will develop at least one skin cancer. Learn to spot the early warning signs. Skin cancer can be cured if itâs found and treated early.
Specific Toxicities And Management

Regional toxicities from HILP are caused by sensitivity of normal tissue to the high concentrations of toxic agents, hyperthermia, and mild acidemia. These may be in the form of lymphedema, skin blistering, painful neuralgia, or painful myopathy. The latter two conditions are managed conservatively with gabapentin and analgesics. Leg edema is managed with elevation and compression wraps. Skin blistering is self-limiting, and managed conservatively. Muscle injury and swelling is a grave sign because it can lead to compartment syndrome .
Postoperative hypotension resulting from cytokine storm may be observed even in the absence of TNF in the perfusate and requires pressor agents for management. Melphalan left in the tissues of the extremity at the completion of perfusion and wash enters the systemic circulation once limb vascularization is restored. This may cause acute postoperative nausea and emesis, which can be effectively managed with odansetron. Systemic melphalan may also lead to marrow suppression, manifest by neutropenia or pancytopenia 714 days after HILP.
Recommended Reading: Melanoma Bone Cancer Life Expectancy
What’s My Risk Of Developing A New Primary Melanoma
As far as developing new cancers, it has been estimated that individuals with melanoma have a 9-fold increase in risk in developing new, primary melanomas, as well as a 28% overall increase in risk of developing a new primary cancer that isnt melanoma, also referred to as a second cancer. Specifically, individuals with melanoma are at a higher risk of developing second cancers in the prostate gland, breasts, salivary glands, kidneys, and thyroid glands, as well as a higher risk of developing leukemia and non-Hodgkin lymphoma.4
Factors that contribute to the development of a new primary melanoma include gender, genetics, age, and original melanoma location. For example, the younger an individual is at original diagnosis, the greater their risk is of developing a new melanoma. This could be due to a genetic tendency to developing melanomas, since melanoma diagnosed in individuals 30 years old or younger is often due to genetic factors. Also, women who have had an original melanoma on the head or neck region are at a higher risk of developing subsequent primary melanomas. Additionally, the risk of developing a new primary melanoma decreases each year after diagnosis and treatment, however, individuals with melanoma are a higher risk of developing a new melanoma than the general population for up to 20 years.4
Could I Get A Second Cancer After Melanoma Treatment
People whove had melanoma can still get other cancers. In fact, melanoma survivors are at higher risk for getting some other types of cancer:
- Another skin cancer, including melanoma
- Salivary gland cancer
- Non-Hodgkin lymphoma
The most common second cancer in survivors of skin melanoma is another skin cancer.
There are steps you can take to lower your risk of getting another cancer and stay as healthy as possible. For example, its important to limit your exposure to UV rays, which can increase your risk for many types of skin cancer. Its also important to stay away from tobacco products. Smoking increases the risk of many cancers.
To help maintain good health, melanoma survivors should also:
- Get to and stay at a healthy weight
- Keep physically active and limit the time you spend sitting or lying down
- Follow a healthy eating pattern that includes plenty of fruits, vegetables, and whole grains, and limits or avoids red and processed meats, sugary drinks, and highly processed foods
- Not drink alcohol. If you do drink, have no more than 1 drink per day for women or 2 per day for men
These steps may also lower the risk of other health problems.
Melanoma survivors should also follow the American Cancer Society guidelines for the early detection of cancer, such as those for colorectal and lung cancer. Most experts dont recommend any other specific tests to look for second cancers unless you have symptoms.
You May Like: What Is Braf Testing In Melanoma
Who Gets Nodular Melanoma
Nodular melanoma accounts for about 15% of melanoma in Australia and New Zealand. Although more common in very fair skin , it may also occur in those who tan quite easily , and occasionally in brown or black skin .
Nodular melanoma is more common in males than in females. Most are over the age of 50 when it is diagnosed.
The main risk factors for nodular melanoma are:
- Increasing age
- Previous invasive melanoma or melanoma in situ
- Many melanocyticnaevi
- Multiple atypical naevi
- Fair skin that burns easily
It is less strongly associated with sun exposure than superficial spreading and lentigo maligna types of melanoma.
Staging With Sentinel Lymph Node Biopsy
Johns Hopkins faculty were some of the first to perform sentinel lymph node biopsies when the technique was introduced in the 1980s. Sentinel lymph node biopsy is now well-established as a staging procedure for patients with newly diagnosed melanoma. Sentinel node biopsy results help us estimate a patients future risk of recurrence and often helps guide treatment choices. Areas of ongoing debate surrounding the procedure involve interpretation of whether residual microscopic disease has an impact on outcomes and whether all patients need complete lymph node dissections upon finding microscopic deposits of melanoma in sentinel lymph nodes.
Multicenter Selective Lymphadenectomy Trial II: Johns Hopkins will be participating in an international study called the Multicenter Selective Lymphadenectomy Trial II to determine whether patients with melanoma in the sentinel node have better survival with complete node dissection as compared to patients who are observed without complete dissection. Patients enrolling in the trial will be randomly assigned to receive either complete dissection or close observation with follow-up ultrasound.
Don’t Miss: Cancer Spread All Over Body
Red Flag #: Unexplained Weight Loss And Loss Of Appetite
Unintentional weight loss is a common side effect of any cancer. When it comes to melanoma, extreme weight loss usually only happens after the cancer has spread from the skin to other parts of the body. Dr. Zaba says she can sometimes tell if a patients melanoma has metastasized because it looks like they have cachexia, a syndrome marked by drastic loss of fat and muscle and increased weakness. Cachexia can also cause loss of appetite, which further contributes to the problem.
Treatment Options For Recurrent Melanoma
Most treatment options are on the table for recurrent melanoma.2 Treatment will be chosen based on stage of the original tumor, previous treatment, and where the cancer recurs.
You may be treated with a primary treatment, followed by adjuvant treatment. Adjuvant treatment kills any cancer cells that remain. You will start with the treatments that are most likely to work . If they are not working or they stop working, âsecond-lineâ therapies are offered. Second-line therapies may be in a different drug class than first-line therapy. They may be less effective or have more severe side effects.
Cancer confined to a skin tumor may be removed with surgery, injected with medication, or treated with radiation therapy or topical medication.2 Melanoma on the arm or leg may be treated with chemotherapy in that limb. If cancer recurs in the lymph nodes, they will be removed with surgery, if possible. Adjuvant treatment options include radiation, interferon-alfa, Yervoy® , or biochemotherapy.
Metastatic disease may be treated with systemic medications:
Don’t Miss: Cancer Lesion Pictures
What Happens At Follow
The primary purpose of follow-up is to detect recurrences early, but it also offers an opportunity to diagnose a new primary melanoma at the first possible opportunity. A second invasive melanoma occurs in 5-10% patients an unrelated melanoma in situ affects in more than 20% of melanoma patients.
The Australian and New Zealand Guidelines for the Management of Melanoma make the following recommendations for follow-up for patients with invasive melanoma.
- Self-skin examination
- Routine skin checks by a patient’s preferred health professional
- Follow-up intervals are preferably six-monthly for five years for patients with stage 1 disease, three-monthly or four-monthly for five years for patients with stage 2 or 3 disease, and yearly after that for all patients.
- Individual patients needs should be considered before an appropriate follow-up is offered
- Provide education and support to help the patient adjust to their illness
The follow-up appointments may be undertaken by the patient’s general practitioner or specialist, or they may be shared.
Follow-up appointments may include:
- A check of the scar where the primary melanoma was removed
- A feel for the regional lymph nodes
- A general skin examination
- A full physical examination
- In those with many moles or atypical moles, baseline whole-body imaging and sequential macro and dermoscopic images of melanocytic lesions of concern
In those with more advanced primary disease, follow-up may include: