Bladder Cancer Clinical Trials
What about Clinical Trials?
You may hear about clinical trials for your bladder cancer. Clinical trials are research studies that test if a new treatment or procedure is safe and effective.
Through clinical trials, doctors find new ways to improve treatments and the quality of life for people with disease. Trials are available for all stages of cancer. The results of a clinical trial can make a major difference to patients and their families. Please visit our clinical trials research webpage to learn more.
Turbt/ Repeat Resection: Timing Technique Goal Indication
Guideline Statement 12
12. In a patient with non-muscle invasive disease who underwent an incomplete initial resection , a clinician should perform repeat transurethral resection or endoscopic treatment of all remaining tumor if technically feasible.
Discussion
Incomplete resection is likely a significant contributing factor to what have been described and diagnosed as early recurrences, as tumors have been noted at the first follow-up cystoscopic evaluation in up to 45% of patients. 57 The Panel recognizes specific, albeit rare, circumstances in which transurethral resection is not likely to impact clinical management and may be omitted for patients with incompletely resected non-muscle invasive disease. Examples of such patients include those with large-volume, high-grade tumors not amenable to complete endoscopic resection for whom immediate radical cystectomy is planned. An additional example includes those patients with a tumor diagnosed within a bladder diverticulum and for whom subsequent surgical resection is planned. However, for the majority of patients, complete resection is essential for adequate staging and optimal clinical management. Although surgeons may utilize BLC for this situation, of note, there is insufficient evidence in this repeat transurethral resection setting to support the routine use of enhanced or BLC versus standard WLC, particularly in light of the noted increase in false positive diagnosis with BLC following recent TURBT. 116-118
Discussion
Radiation And Systemic Chemotherapy
Transitional cell carcinoma of the renal pelvis and ureter is relatively rare, which leads to a paucity of studies analyzing adjuvant radiation and chemotherapy for locally advanced but completely resected upper tract urothelial tumors. Patients who harbor disease beyond the muscularis have a 5-year survival rate between 0 and 34%. Without adjuvant therapy, several studies have reported between 45% and 60% incidence of locoregional recurrence at 5 years after treatment with definitive surgery. This high recurrence rate has been a strong argument for adjuvant therapy for all patients with locally advanced disease even after complete resection. However, the studies that currently exist are of limited numbers of patients because of the rarity of this disease. Studies have both supported,, and rejected, the role of adjuvant radiation treatment for upper tract urothelial malignancies. The role of adjuvant chemotherapy alone for transitional cell carcinoma also remains controversial.
Recommended Reading: Can Skin Cancer Cause Nausea
Standard Treatment Options For Stages Ii And Iii Bladder Cancer
The most common treatments for muscle-invasive bladder cancer are radical cystectomy and radiation therapy. There is no strong evidence from randomized controlled trials to determine whether surgery or radiation therapy is more effective. There is strong evidence that both therapies become more effective when combined with chemotherapy. The treatments with the highest level of evidence supporting their effectiveness are radical cystectomy preceded by multiagent cisplatin-based chemotherapy and radiation therapy with concomitant chemotherapy.
Radical cystectomy
Radical cystectomy is a standard treatment option for stage II and stage III bladder cancer, and its effectiveness at prolonging survival increases if it is preceded by cisplatin-based multiagent chemotherapy. Radical cystectomy is accompanied by pelvic lymph node dissection and includes removal of the bladder, perivesical tissues, prostate, and seminal vesicles in men and removal of the uterus, fallopian tubes, ovaries, anterior vaginal wall, and urethra in women. Studies of outcomes after radical cystectomy report increased survival in patients who had more, rather than fewer, lymph nodes resected whether this represents a therapeutic benefit of resecting additional nodes or stage migration is unknown. There are no randomized controlled trials evaluating the therapeutic benefit of lymph node dissection in this setting.
Evidence :
Evidence :
Segmental cystectomy
Stage Information For Bladder Cancer
The clinical staging of carcinoma of the bladder is determined by the depth of invasion of the bladder wall by the tumor. This determination requires a cystoscopic examination that includes a biopsy and examination under anesthesia to assess the following:
- Size and mobility of palpable masses.
- Degree of induration of the bladder wall.
- Presence of extravesical extension or invasion of adjacent organs.
Clinical staging, even when computed tomographic and/or magnetic resonance imaging scans and other imaging modalities are used, often underestimates the extent of tumor, particularly in cancers that are less differentiated and more deeply invasive. CT imaging is the standard staging modality. A clinical benefit from obtaining MRI or positron emission tomography scans instead of CT imaging has not been demonstrated.
Also Check: Is Basal Cell Carcinoma Slow Growing
Tests To Detect Abnormal Urine Cytology:
- Visual examination: Here, the urethra is seen using a cystoscope it is a thin tube with a small camera at the end. From this device, its easy to see the cells and their structure.
- Dipstick test: A plastic stick containing chemicals is dipped into the urine to test the color change and aberrant condition.
- Microscopic examination: Here, the microscope is used to see the abnormal particles that are causing infection or inflammation.
- FISH: This test is called Fluorescence in situ Hybridization, also popularly known as Fish Urine Cytology. This test is done for diagnosing or monitoring urothelial cancer.
After the procedure
The pathologist diagnoses the samples of the urine and checks for the abnormal signs or warnings that indicate carcinoma. Urine cytology results can take 1-2 or even more days. Understanding the samples may require time and other tests such as routine biopsy is also performed to know the exact conditions of cells. Urine cytology results from pathology lab reports include terms such as unsatisfactory specimen, negative, positive, urine cytology atypical cells or suspicious, which means:
Cells responsible for contamination of urine:
Voided urine cytology bladder cancer, test:
Malignant cells in urine cytology
Complete Blood Count And Chemistry Panel
On the complete blood count , the presence of anemia or an elevated white blood cell count warrants further investigation for an explanation.
The chemistry panel should include liver function studies. Although BCG is administered intravesically, systemic absorption of this agent can produce acute hepatitis. Performing baseline liver function tests before initiating therapy and repeating these tests during the course of therapy is important to help prevent serious adverse events and to determine when therapy should be stopped. In patients with suspected metastasis to liver or bone, liver function tests and measurement of the bony fraction of alkaline phosphatase should be performed.
Kidney function should be evaluated prior to the initiation of therapy because patients with marginal or abnormal kidney function may have an obstruction or some type of renal disease that may worsen with intravesical therapy. Kidney function can be evaluated with serum creatinine measurements or technetium scans of the kidneys.
Also Check: How To Say Squamous Cell Carcinoma
Cystectomy Cystoprostatectomy And Pelvic Exenteration Specimens
Processing of these specimens may be summarized in three steps: orientation of the specimen and identification of relevant anatomic structures , fixation of the specimen and dissection of the specimen. Peritoneum covering the surface of the bladder is a reliable anatomic landmark. In both male and female patients, the peritoneum descends further along the posterior wall of the bladder than it does along the anterior wall. Other pelvic organs, if present, may also be used to orient the specimen. In the male, the bladder adjoins the rectum and seminal vesicles posteriorly, the prostate inferiorly, and the pubis and peritoneum anteriorly. In the female, the vagina is located posteriorly, and the uterus is located superiorly. Once the specimen is oriented, both ureters and, when present, the vasa deferentia should be identified. Location and dissection of the ureters is easier after fixation. The outer dimensions of the urinary bladder, as well as the length and diameter of ureters, should be recorded. The external surface of the bladder should be inked.
The minimum number of sections to be taken are as follows: tumor bladder neck , trigone , anterior wall , posterior wall , lateral walls , dome , ureteral orifices , margins , any abnormal appearing bladder mucosa and any perivesical lymph nodes .
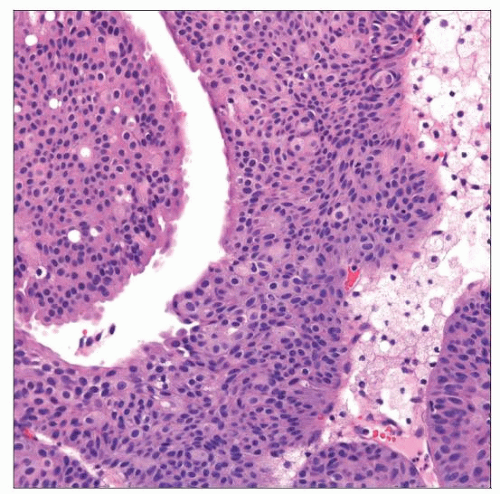
Figure 18
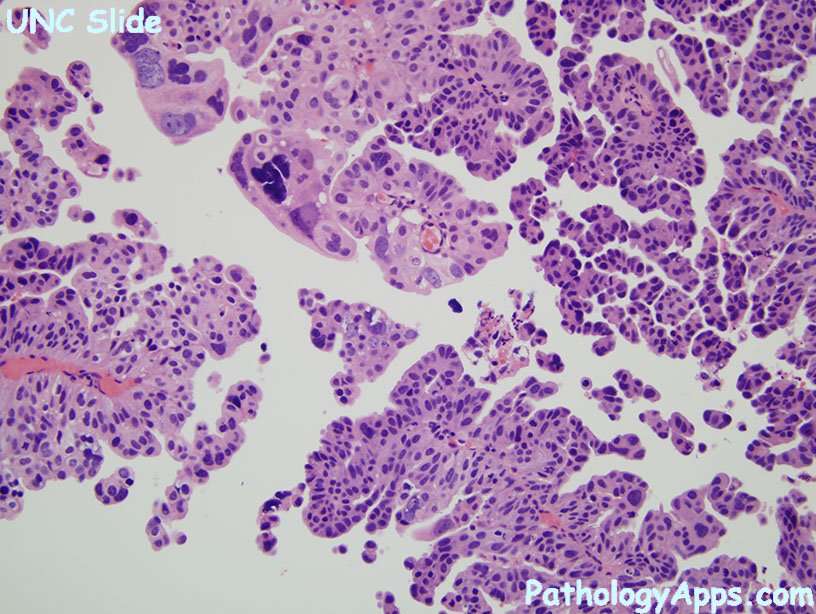
Cellular Classification Of Bladder Cancer
More than 90% of bladder cancers are transitional cell carcinomas derived from the uroepithelium. About 2% to 7% are squamous cell carcinomas, and 2% are adenocarcinomas. Adenocarcinomas may be of urachal origin or nonurachal origin the latter type is generally thought to arise from metaplasia of chronically irritated transitional epithelium. Small cell carcinomas also may develop in the bladder. Sarcomas of the bladder are very rare.
Pathologic grade of transitional cell carcinomas, which is based on cellular atypia, nuclear abnormalities, and the number of mitotic figures, is of great prognostic importance.
References
Recommended Reading: How Fast Does Squamous Cell Skin Cancer Spread
Urine Cytology Collection Report:
A report consisting of values of carcinoma-in-situ , low-grade urothelial neoplasm , high-grade urothelial neoplasm , positive predictive value . Also, the number of atypical urothelial cells and suspicious for high-grade urothelial carcinoma is called a urine cytology report.
High-grade cancer cells that become tumor after growing at a particular extent is called high-grade urothelial neoplasm . These cells multiply and are predicted to have a worse condition.
Low-grade urothelial neoplasm is linked to atypical urothelial cells. Low-grade urothelial carcinoma is also reported where the cells grow very slowly as a result of low malignant potential of the tumor.
Sometimes there may be cancer cells detected in high-grade urothelial neoplasm, but the number of cancer cells may be not as much as required for a malignancy. Therefore, the report indicates suspicion for high-grade urothelial neoplasm.
Types Of Bladder Cancer
The type of bladder cancer depends on how the tumors cells look under the microscope. The 3 main types of bladder cancer are:
-
Urothelial carcinoma. Urothelial carcinoma accounts for about 90% of all bladder cancers. It also accounts for 10% to 15% of kidney cancers diagnosed in adults. It begins in the urothelial cells found in the urinary tract. Urothelial carcinoma is sometimes also called transitional cell carcinoma or TCC.
-
Squamous cell carcinoma. Squamous cells develop in the bladder lining in response to irritation and inflammation. Over time, these cells may become cancerous. Squamous cell carcinoma accounts for about 4% of all bladder cancers.
-
Adenocarcinoma. This type accounts for about 2% of all bladder cancers and develops from glandular cells.
There are other, less common types of bladder cancer, including sarcoma of the bladder and small cell bladder cancer, among others. Sarcomas of the bladder often begin in the fat or muscle layers of the bladder. Small cell bladder cancer is a rare type of bladder cancer that is likely to spread to other parts of the body.
Recommended Reading: Can You Get Skin Cancer On Your Scalp
Standardization Of The Reporting System
Anatomic pathologists serve as consultants to their clinical colleagues and patients, and pathology reports officially document this communication. To help clinicians choose the optimal management options for the patient, reports must accurately and clearly communicate the cytopathologic findings and outcome probability.
Pathologists actively use the terms suspicious’, indeterminate’, or atypical’ – all too often with resultant failure to provide a clear diagnostic and therapeutic path for clinicians. A survey of pathologists and clinicians performed by Redman et al. documented the need for a more standardized terminology for reporting cytopathology results and for the education of clinicians on that terminology. Although pathologists have paid attention to all elements of the pathology report , they have not focused on the issue of report comprehension. In a study looking at surgical pathology reports, surgeons misunderstood pathologists’ reports 30% of the time . One of the issues shared by patients and their advocates on Web sites dedicated to cancer advocacy is that different pathologists and/or different institutions use different highly technical terms to describe the same entities, predictably confusing to both patients and their clinicians.
Treatment Options Under Clinical Evaluation For Patients With Any T Any N M1 Disease
Prognosis is poor in patients with stage IV disease and consideration of entry into a clinical trial is appropriate.
Other chemotherapy regimens appear to be active in the treatment of metastatic disease. Chemotherapy agents that have shown activity in metastatic bladder cancer include paclitaxel, docetaxel, ifosfamide, gallium nitrate, and pemetrexed.
Read Also: How To Check For Melanoma
What Features Distinguish Urothelial Lesions On Urine Cytology According To The Paris System
Negative for High-Grade Urothelial Carcinoma
Groups of urothelial cells are considered normal unless they meet criteria for atypia. Normal urothelial and squamous cells are the most common cellular elements observed . This category does not rule out LGUC. Rather, it is designed to denote the absence of a high-grade lesion.
Urothelial Cis Without Ihc
All cases of urothelial CIS without IHC were positive for AMACR with a mean intensity of 2.1. The percentage of cases with positive or partially positive AMACR expression was significantly greater for urothelial CIS without IHC compared to urothelial CIS with IHC . The mean intensity was greater in the group urothelial CIS with IHC compared to without IHC, but the difference was not significant . The rate of positivity of AMACR was significantly lower for non-neoplastic urothelium with IHC compared to urothelial CIS without IHC and urothelial CIS with IHC .
You May Like: What Is The Main Cause Of Skin Cancer
What Are The Patients Risk Factors For Urothelial Carcinoma
This patients main risk factors for urothelial carcinoma of the bladder include smoking history, gender, and age. Smoking is the most significant risk factor for UC, contributing to approximately 50% of tumors . Aromatic amines from cigarette smoke are renally cleared and exert their carcinogenic effect on the urinary tract. Both cigarette smoking and environmental exposure to tobacco smoke have been shown to contribute significant risk. The second largest contributor is occupational exposure to aromatic amines in industries involving processing paint, dye, metal, and petroleum products. However, occupational exposures have decreased in recent years due to increased safety measures. Water intake is associated with decreased risk, likely due to the dilution of potential carcinogens in the urinary tract. Additional risk factors include male gender, white race, first-degree relative with UC, arsenic exposure, schistosomiasis, and chronic urinary tract inflammation or dilation, such as in chronic urinary retention. However, female gender and black race are associated with reduced survival.
What Does It Mean When Your Urine Cytology Test Result Says Negative For High
| Umbrella cell of the bladder that looks kind of like an umbrella.Urinary Tract Cytology. . Retrieved February 7, 2015 fromhttp://www.cytologystuff.com/study/section17ng.htm |
almost
| High-grade urothelial carcinoma cells that show highN/C ratio, irregular nuclei, coarse chromatin, hyperchromasia, and irregularnucleoli. Urinary Tract Cytology. . Retrieved July 7, 2019 https://cytologystuff.com/study/non-gyn-atlas/urinary-tract-cytology-high-grade-urothelial-carcinoma/ |
| Umbrella cell of the bladder. Without umbrella cells,urine trouble! Umbrella cells are found in the lining of yourbladder and are among the largest of human epithelial cells. They are calledumbrella cells because they are the superficial cells of the urothelium and extendover smaller cells of the underlying layers. Although large, they have a lownuclear to cytoplasmic ratio and they are often multinucleated. They can alsostretch as needed!Image photographed by IvanAditya |
| A leaky umbrella cell.Image photographed by IvanAditya |
Read Also: Is Melanoma Caused By Sun Exposure
Standard Treatment Options For Stage I Bladder Cancer
Patients with stage I bladder tumors are unlikely to die from bladder cancer, but the tendency for new tumor formation is high. In a series of patients with Ta or T1 tumors who were followed for a minimum of 20 years or until death, the risk of bladder recurrence after initial resection was 80%. Of greater concern than recurrence is the risk of progression to muscle-invasive, locally-advanced, or metastatic bladder cancer. While progression is rare for low-grade tumors, it is common among high-grade cancers.
One series of 125 patients with TaG3 cancers followed for 15 to 20 years reported that 39% progressed to more advanced stage disease, while 26% died of urothelial cancer. In comparison, among 23 patients with TaG1 tumors, none died and 5% progressed. Risk factors for recurrence and progression include the following:
- High-grade disease.
TUR with fulguration followed by an immediate postoperative instillation of intravesical chemotherapy
TUR and fulguration are the most common and conservative forms of management. Careful surveillance of subsequent bladder tumor progression is important. Because most bladder cancers recur after TUR, one immediate intravesical instillation of chemotherapy after TUR is widely used. Numerous randomized, controlled trials have evaluated this practice, and a meta-analysis of seven trials reported that a single intravesical treatment with chemotherapy reduced the odds of recurrence by 39% .
TUR with fulguration
Evidence :
Paris System For Urothelial Neoplasia
Topic Completed:Minor changes:Copyright: Page views in 2020:Page views in 2021 to date:Cite this page:
- Urine Cytology represents a significant portion on non-gynecologic cytology specimens in daily practice, primarily because of the simplicity and ease of specimen procurement and its significant impact on management
- However there was no consensus on the various categories and their cytomorphologic features used for reporting
- Paris System for reporting urinary cytology was an effort to standardize terminology with standardized cytomorphologic criteria for reporting urine cytology
- Paris System is based on the principle that the ultimate goal of urine cytology is detection of high grade urothelial carcinoma
Contributed by Vaishali Pansare, M.D.
Adequacy of urine specimens
- Cytology is useful to detect carcinoma in situ or marked chronic inflammation , carcinoma hidden in diverticula, or for detecting residual tumor from urine specimens
- Cystoscopic biopsy of visible lesions is more sensitive than cytology in most cases
- Bladder irrigation is superior to collecting voided urine
- Most sensitive and highly specific for high grade tumors whether flat , papillary or mixed
- Low sensitivity for papilloma and low malignant potential lesions because they have normal histology
- Follow up examination of urine with FISH may improve sensitivity and specificity of cytology
Voided urine:Instrumented urine:
- Catheterization of the bladder or irrigation of bladder
Ileal conduit urine:
Don’t Miss: Does Insurance Cover Skin Cancer Screening