What Are The 5 Stages Of Skin Cancer
Staging is an important tool used to treat skin cancer. Your stage helps the medical team determine where the tumor is, how large it is, where it has spread, your prognosis, and the most effective treatment plan.
The five stages of squamous cell carcinoma include:
- Stage 0: Also known as carcinoma in situ, in this stage cancer is present in the epidermis. It has not spread to deeper layers.
- Stage 1: The tumor is smaller than 2 centimeters and has not spread to nearby lymph nodes or other organs. The individual has one or fewer risk factors for spread.
- Stage 2: The tumor is wider than 2 centimeters and has not spread to nearby lymph nodes or other organs. This stage also applies to any sized tumor when the individual has two or more risk factors.
- Stage 3: The tumor has spread into nearby facial bones or one lymph node. It has not spread to other organs.
- Stage 4: The tumor is of any size and has metastasized to one or more of the lymph nodes. It may have spread to the bones and other distant organs.
Stage Iii Squamous Cell Carcinoma
The tumor cells may be of any size at the original site. A stage III SCC has begun to invade the nearby lymph nodes on the side of the body of the original cancerous growth. This new growth is still under 3 cm in size. It may also have grown into the facial bones like the bones surrounding the eye or your jaw bone.9 It has not affected any other organs.10
Citation Doi And Article Data
Citation:DOI:Dr Marcin CzarnieckiRevisions:see full revision historySystems: Synonyms:
Squamous cell carcinoma of the penis arises most commonly at the distal end of the penile urethra with local invasion of the glans.
In addition to TNM classification, the following staging is used:
Staging
- stage I: confined to the glans or foreskin
- stage II: invasion of penile shaft
- stage III: invasion of regional lymph nodes
- stage IV: distant metastasis
- 1. www.cancer.gov. Read relevant article. Accessed on 26/12/2015
- 2. Grainger RG, Allison DJ. Grainger and Allison’s diagnostic radiology, a textbook of medical imaging. Churchill Livingstone. ISBN:0443064326. –
You May Like: Invasive Ductal Carcinoma Prognosis
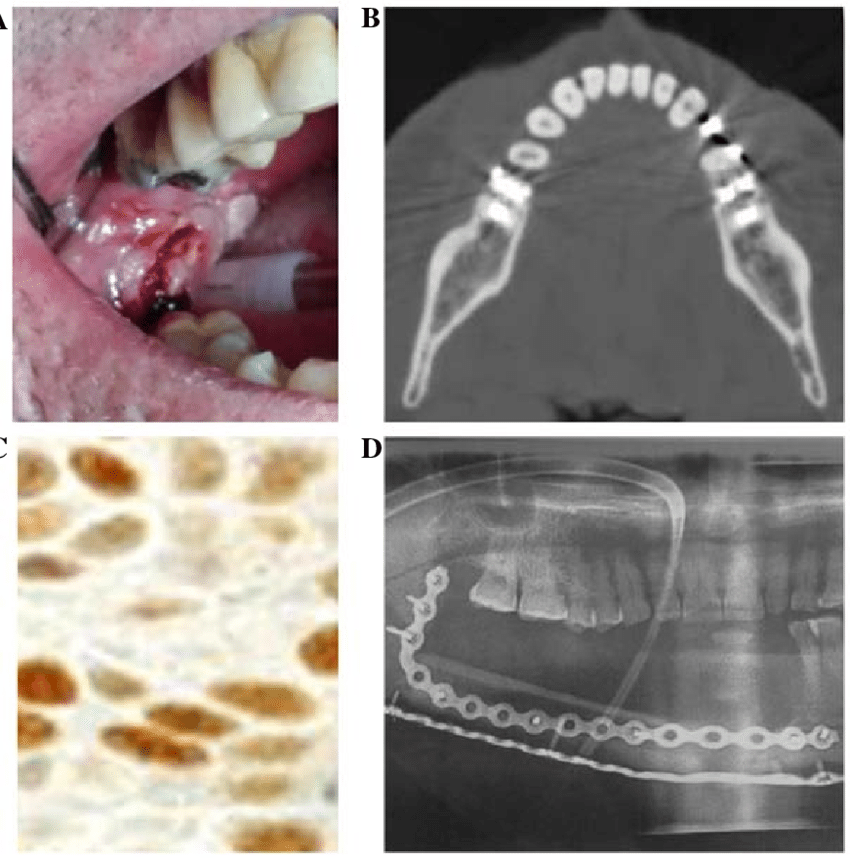
How Is Squamous Cell Carcinoma Of Oral Cavity Treated
Early diagnosis and treatment of Squamous Cell Carcinoma of Oral Cavity is important to avoid complications such as metastasis to other regions. The treatment measures may include:
- In most cases, a wide surgical excision and removal of the entire tumor is the preferred treatment option. This may be followed by radiation therapy and/or chemotherapy
- If the tumor has metastasized , then a combination of chemotherapy, radiation therapy, and invasive procedures may be used to treat the tumor
- Targeted therapy medications are generally used for locally infiltrated or metastatic SCCs. This therapy destroys the tumor cells by acting against the proteins that are responsible for tumor growth
- Reconstructive surgery may be necessary after cancer therapy
- Post-operative care is important: One must maintain minimum activity levels, until the surgical wound heals
- Follow-up care with regular screening and check-ups are important and encouraged
Squamous Cell Carcinoma Survival Rate
In general, the squamous cell carcinoma survival rate is very highwhen detected early, the five-year survival rate is 99 percent. Even if squamous cell carcinoma has spread to nearby lymph nodes, the cancer may be effectively treated through a combination of surgery and radiation treatment. Nevertheless, a patient who has been treated for squamous cell carcinoma in the past always faces the possibility of a recurrence, so lifelong monitoring to increase the chance of early detection is highly encouraged.
Read Also: What Does Stage 3b Melanoma Mean
How Is Squamous Cell Carcinoma Of Oral Cavity Diagnosed
A diagnosis of Squamous Cell Carcinoma of Oral Cavity is made by:
- Complete physical examination with detailed medical history evaluation
- Examination by a dermatologist using a dermoscopy, a special device to examine the skin
- Woodâs lamp examination: In this procedure, the healthcare provider examines the skin using ultraviolet light. It is performed to examine the change in skin pigmentation
Although the above modalities can be used to make an initial diagnosis, a tissue biopsy of the tumor is necessary to make a definitive diagnosis to begin treatment.
Tissue biopsy:
- A tissue biopsy of the tumor is performed and sent to a laboratory for a pathological examination. A pathologist examines the biopsy under a microscope. After putting together clinical findings, special studies on tissues and with microscope findings, the pathologist arrives at a definitive diagnosis. Examination of the biopsy under a microscope by a pathologist is considered to be gold standard in arriving at a conclusive diagnosis
- Biopsy specimens are studied initially using Hematoxylin and Eosin staining. The pathologist then decides on additional studies depending on the clinical situation
- Sometimes, the pathologist may perform special studies, which may include immunohistochemical stains, molecular testing, and very rarely, electron microscopic studies to assist in the diagnosis
In case of metastatic SCC, the following diagnostic procedures can be used to procure the tissue sample:
Features Of T Categories
The T categories describe the main tumor based on its thickness, the presence of high-risk features, and invasion.2 Your doctor begins to gather this information by doing a skin biopsy. If the tumor is invasive, you will need imaging tests.
- Size. The longest dimension of the tumor is measured in centimeters.
- Invasion. The tumor is categorized by how far it has invaded the body. Invasion of the facial bones is categorized as T3. Invasion of bones in the rest of the body or the base of the skull is T4. Your doctor determines this using magnetic resonance imaging or computed tomography scan.
- High-risk features. High-risk features refer to the risk that the cancer returns or spreads . High-risk features of SCC are:2
- > 2 mm thick or Clark level IV
- Growing around a nerve
- Located on the ear or lip
- Poorly differentiated or undifferentiated cells. Differentiation means how much the cancer cells look like the normal tissue that it came from. Poorly differentiated cells grow and spread more quickly.
Recommended Reading: Skin Cancer Metastasis To Lymph Nodes
How To Improve Your Odds
Even if youve exhausted all of your treatment options, you dont have to give up. Researchers are always testing new SCC treatments in clinical trials. Getting into one of these studies could give you access to a drug or therapy that might slow or stop your cancer.
To avoid the worsening of your skin cancer or a new cancer in a different area, protect yourself from the suns damaging UV rays. Wear sun-protective clothing and a wide-brimmed hat whenever you go outdoors. Apply a layer of broad-spectrum sunscreen that protects against both UVA and UVB rays.
Also check your own skin for any new growths on a regular basis. Report any skin changes to your doctor right away.
How Do Doctors Find Out Your Stage
There are different ways to find out your stage. Your doctor might use:
- clinical staging before treatment and if you don’t have surgery
- pathological staging if you do have surgery
- post neoadjuvant staging if you have chemotherapy or radiotherapy before surgery
Clinical staging means the doctor stages you after examining you and looking at test and scan results. Doctors use clinical staging to plan your treatment. Its also the best way to stage people who arent having surgery. You might see your clinical stage written as cTNM.
Pathological staging means the doctor stages you after examining the tissue that the surgeon removes during an operation. This is also called surgical staging. The doctors combine your clinical stage results with the surgical results. Pathological staging is generally a more precise way to find out how far your cancer has spread. Your pathological stage might be different to your clinical stage. You might see your pathological stage written as pTNM.
Post neoadjuvant staging means you have had chemotherapy or radiotherapy before surgery and the doctor stages you again after surgery. You might see your post neoadjuvant stage written as ypTNM.
For oesophageal cancer, the clinical, pathological, and post neoadjuvant staging are all different. In this section we describe the pathological and clinical stages.
You May Like: Can You Die From Basal Cell Skin Cancer
What Is The Outlook For Cutaneous Squamous Cell Carcinoma
Most SCCs are cured by treatment. A cure is most likely if treatment is undertaken when the lesion is small. The risk of recurrence or disease-associated death is greater for tumours that are > 20 mm in diameter and/or > 2 mm in thickness at the time of surgical excision.
About 50% of people at high risk of SCC develop a second one within 5 years of the first. They are also at increased risk of other skin cancers, especially melanoma. Regular self-skin examinations and long-term annual skin checks by an experienced health professional are recommended.
Moffitt Cancer Centers Approach To Squamous Cell Carcinoma
At Moffitt Cancer Center, our multispecialty team of cancer experts takes a highly individualized approach to squamous cell carcinoma treatment. We offer the latest diagnostic and treatment options, and we work closely with each patient to offer customized guidance and help ensure the best possible outcome. For instance, there are many steps a patient can take to improve his or her own squamous cell carcinoma prognosis regardless of the general survival rate such as:
- Performing self-examinations from head to toe, including parts of the body that are not regularly exposed to UV rays, at least monthly, and promptly reporting any suspicious or unusual changes in skin texture or appearance to a physician
- Seeing a physician for a professional skin cancer examination yearly
- Avoiding exposure to the suns ultraviolet rays while outdoors, preventive measures include seeking shade, wearing sunglasses and a brimmed hat, covering up with clothing and using a broad spectrum sunscreen with both UVA and UVB protection
- Never using indoor tanning beds
If youd like to learn more about the squamous cell carcinoma survival rate, the experts at Moffitt can put this information into the proper context for you and help you take appropriate steps to achieve the best possible outcome. Call or complete a new patient registration form online. We see patients with and without referrals.
Read Also: Ductal Carcinoma Survival Rates
Effective Options For Early Stage Scc
Most squamous cell carcinomas of the skin can be cured when found and treated early. Treatment should happen as soon as possible after diagnosis, since more advanced SCCs of the skin are more difficult to treat and can become dangerous, spreading to local lymph nodes, distant tissues and organs. Find out more about treatment options for advanced or recurring SCCs here.
If youve been diagnosed with an SCC that has not spread, there are several effective treatments that can usually be performed on an outpatient basis. The choices available to you depend on the tumor type, size, location and depth, as well as your age and overall health.
Options include:
What Causes Cutaneous Squamous Cell Carcinoma
More than 90% of cases of SCC are associated with numerous DNAmutations in multiple somaticgenes. Mutations in the p53 tumour suppressor gene are caused by exposure to ultraviolet radiation , especially UVB . Other signature mutations relate to cigarette smoking, ageing and immune suppression . Mutations in signalling pathways affect the epidermalgrowth factorreceptor, RAS, Fyn, and p16INK4a signalling.
Beta-genus human papillomaviruses are thought to play a role in SCC arising in immune-suppressed populations. -HPV and HPV subtypes 5, 8, 17, 20, 24, and 38 have also been associated with an increased risk of cutaneous SCC in immunocompetent individuals.
Don’t Miss: Squamous Cell Carcinoma Scalp Prognosis
How The Stage Is Determined
Once you have been diagnosed with squamous cell carcinoma, your doctor will want to determine its stage. While the risk of this type of cancer spreading is low, determining the stage will help your doctor develop the best treatment plan.
The TNM system is a uniform system for staging many types of cancer. TNM stands for:
- T is for tumor: How far has the primary tumor grown through the layers of skin or to nearby tissues?
- N is for nodes: Have cancer cells spread to the lymph nodes near the tumor?
- M is for metastasis: Has the cancer metastasized to distant sites in the body such as the lungs or liver?
Skin Cancer Doctor Discussion Guide
How Skin Cancer Progresses
All cancer starts in one part of your body. With SCC, it starts in your skin. From there, cancer cells can spread.
How far your cancer has spread is known as its stage. Doctors assign skin cancers a stage number between 0 and 4.
Stage 4 means your cancer has spread beyond your skin. Your doctor might call the cancer advanced or metastatic at this stage. It means your cancer has traveled to one or more of your lymph nodes, and it may have reached your bones or other organs.
The stage of your cancer and where it is located will help your doctor find the right treatment for you. At stage 4 your cancer may not be curable, but it is still treatable.
You May Like: What Is Melanoma In The Brain
Basal And Squamous Cell Skin Cancer Stages
After someone is diagnosed with cancer, doctors will try to figure out if it has spread, and if so, how far. This process is called staging. The stage of a cancer describes how much cancer is in the body. It helps determine how serious the cancer is and how best to treat it.
The stage is based on the results of the physical exam, the skin biopsy , and the results of imaging tests if they are done. These exams and tests are described in Tests for Basal and Squamous Cell Skin Cancers.
Determining the stage of basal cell skin cancers is rarely needed, because these cancers are almost always cured before they spread to other parts of the body.
Squamous cell skin cancers are more likely to spread , so determining the stage can be more important, particularly in people who are at higher risk. This includes people with weakened immune systems, such as those who have had organ transplants and people infected with HIV, the virus that causes AIDS. Most squamous cell skin cancers occur in the head and neck region and tend to have a higher risk of recurring or spreading compared to those in other locations.
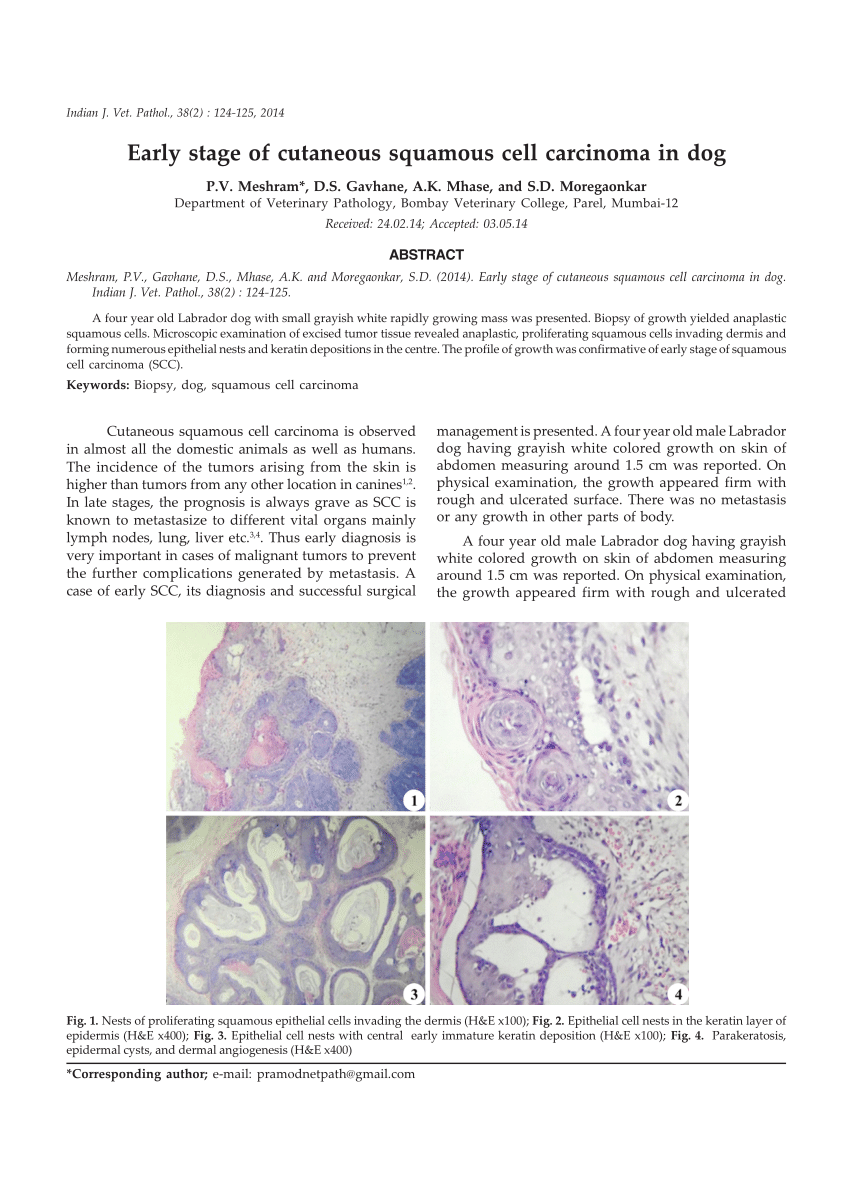
Cancer Squamous Cell Carcinoma
Definition
Squamous cell carcinoma is a malignant condition of the airway epithelium, usually arising from the central portions of the airways and has a strong causative association with smoking. It is the second most common lung cancer, making up 30% of cases.
Structurally squamous cell carcinoma is characterized by its central location and occurs more commonly in the upper lobes. It tends to spread locally to regional nodes and may cavitate which is a characteristic feature of squamous cell carcinomas in general.
The histopathology is characterised by the proliferation of flat fish-scale like cells and may be associated and characterized by the production of keratin and intercellular bridges. Well differentiated SCC contains keratin pearls. The cells have large irregular nuclii, large nucleoli, and coarse chromatin. The cells are arranged in sheets.
Metaplasia, dysplasia, and carcinoma in situ are sometimes present in the tissue surrounding the carcinoma.
Metastatic disease does occur but compared to other lung cancers it is relatively uncommon occurring in < 20% at presentation.
Clinically it often produces symptoms of cough dyspnea or atelectasis, wheezing or hemoptysis since it is more central in its location and affects larger airways. It is also the lung malignancy that is most often associated with hypercalcemia
From a diagnostic point of view, its central location and tendency to exfoliate enables cytological diagnosis from the sputum or bronchial washings.
Don’t Miss: Invasive Ductal Carcinoma Grade 1 Survival Rate
What Is The Prognosis Of Squamous Cell Carcinoma Of Oral Cavity
- In general, Squamous Cell Carcinoma of Oral Cavity is an aggressive form of cancer. If metastasis is observed, then the prognosis is guarded or unpredictable
- Tumors in their early stage with complete excisional treatment typically have good prognosis
- In cases of metastasis, its prognosis depends upon a set of several factors that include:
- Stage of tumor: With lower-stage tumors, when the tumor is confined to site of origin, the prognosis is usually excellent with appropriate therapy. In higher-stage tumors, such as tumors with metastasis, the prognosis is poor
- The surgical respectability of the tumor
- Overall health of the individual: Individuals with overall excellent health have better prognosis compared to those with poor health
- Age of the individual: Older individuals generally have poorer prognosis than younger individuals
- Whether the tumor is occurring for the first time, or is a recurrent tumor. Recurring tumors have a poorer prognosis compared to tumors that do not recur
- Response to treatment: Tumors that respond to treatment have better prognosis compared to tumors that do not respond so well to treatment
What Are The Risk Factors For Squamous Cell Carcinoma Of Tongue
The risk factors for Squamous Cell Carcinoma of Tongue include:
- Smoking and chewing of tobacco are strong risk factors for this type of Tongue Cancer
- Radiation therapy in the region of the tongue
- Arsenic exposure
- Coal tar exposure
- Individuals with weak immune system, which could be due to cancer treatment, AIDS, or those on immunosuppressant drugs after receiving an organ transplant
- Caucasians are more vulnerable compared to other dark-skinned individuals
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases ones chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
You May Like: How To Identify Basal Cell Carcinoma