Research Shows Deadly Tumors May Be Vulnerable To Drugs That Block Their Energy Supply
- Date:
- University of Texas M. D. Anderson Cancer Center
- Summary:
- Melanoma tumors that have spread to the brain are equipped to thwart immunotherapies and targeted therapies that succeed against tumors growing in other sites. Researchers report that the heavy reliance of these tumors on a specific metabolic pathway presents a potentially new therapeutic against these lethal tumors.
Melanoma tumors that have spread to the brain are equipped to thwart immunotherapies and targeted therapies that succeed against tumors growing in other sites. Researchers at The University of Texas MD Anderson Cancer Center report in Cancer Discovery that the heavy reliance of these tumors on a specific metabolic pathway presents a potentially new therapeutic against these lethal tumors.
The team’s in-depth analysis of brain metastases and comparison of those tumors to others that had spread to different parts of the body was the first such application of advanced RNA sequencing and uncovered a variety of factors that make tumors in the brain so difficult to treat.
“Brain metastases are increasingly recognized as one of our biggest challenges in cancer,” said senior author Michael Davies, M.D., Ph.D., associate professor of Melanoma Medical Oncology. “Melanoma patients with advanced disease have the highest risk of developing brain metastases among common solid tumors, and they are a leading cause of death from this disease.”
Beyond the blood-brain barrier
OXPHOS metabolism matters
Story Source:
Whole Brain Radiation Therapy
The first use of external beam WBRT for treatment of brain metastases was reported in 1954 by Chao et al and again later in 1961 by Chu et al. It has since become an important treatment modality for brain metastases. One of the fundamental benefits of WBRT is that it is a noninvasive means in which to treat the entire brain and provide palliation of symptoms. Thus, it allows for relatively simple targeting of any and all lesions in the brain with radiation including microscopic ones, micrometastases, which are not detected on neuroimaging. This has been demonstrated in studies which showed that prophylactic and postoperative irradiation of the brain decreases subsequent development of intracranial metastases. This effect is most likely due to elimination of micrometastases that were present at the time. External WBRT is thus advantageous and typically considered the mainstay of treatment for most patients with multiple metastatic deposits from melanoma in the brain. More localized treatment modalities would be less beneficial in such situations because it would require targeting of each lesion individually. However, solitary metastases that are too large for either surgical resection or stereotactic surgery or those that impinge on sensitive areas of the brain are often treated with WBRT.
Survival And Clinical Outcome
Fifty-nine patients had died of melanoma progression at the time of the analysis, among which 32 died with progressing brain metastases. The median overall survival duration from the time of initial brain metastasis was 12.8;months ;, and the median overall survival duration from the time of initial melanoma diagnosis was 60.5;months for all 79 patients. The median overall survival durations from the time of craniotomy and stereotactic radiosurgery were 17.3;months and 15.4;months , respectively. The median survival durations of patients who received anti-CTLA-4 antibody, anti-PD-1 antibody and BRAF inhibitor after the diagnosis of brain metastasis were 19.2;months , 37.9;months and 12.7;months , respectively. Tables; and describe the outcomes of the entire cohort as well as specific subsets of patients. Figures and illustrate the Kaplan-Meier curves of overall survival for all patients and for those who were treated with or without anti-PD-1 therapy, respectively.
Fig. 1
Recommended Reading: How Do You Know If You Have Basal Cell Carcinoma
Metastatic Melanoma Life Expectancy
The 5-year survival rate for a metastatic melanoma is about 15% to 20% 7). The 10-year survival is about 10% to 15% 8). The outlook is better if the spread is only to distant parts of the skin or distant lymph nodes rather than to other organs, and if the blood level of lactate dehydrogenase is normal.
- The survival differences among M categories will be useful for clinical trial stratification; however, the overall prognosis of all patients with stage IV melanoma remains poor, even among patients with M1a. For this reason, the Melanoma Staging Committee recommended no stage groupings for stage IV.
Table 2. American Joint Committee on Cancer TNM system for Stage 4 Melanoma
| M |
|---|
- A sore that doesnt heal
- Spread of pigment from the border of a spot into surrounding skin
- Redness or a new swelling beyond the border of the mole
- Change in sensation, such as itchiness, tenderness, or pain
- Change in the surface of a mole scaliness, oozing, bleeding, or the appearance of a lump or bump
Be sure to show your doctor any areas that concern you and ask your doctor to look at areas that may be hard for you to see. Its sometimes hard to tell the difference between melanoma and an ordinary mole, even for doctors, so its important to show your doctor any mole that you are unsure of.
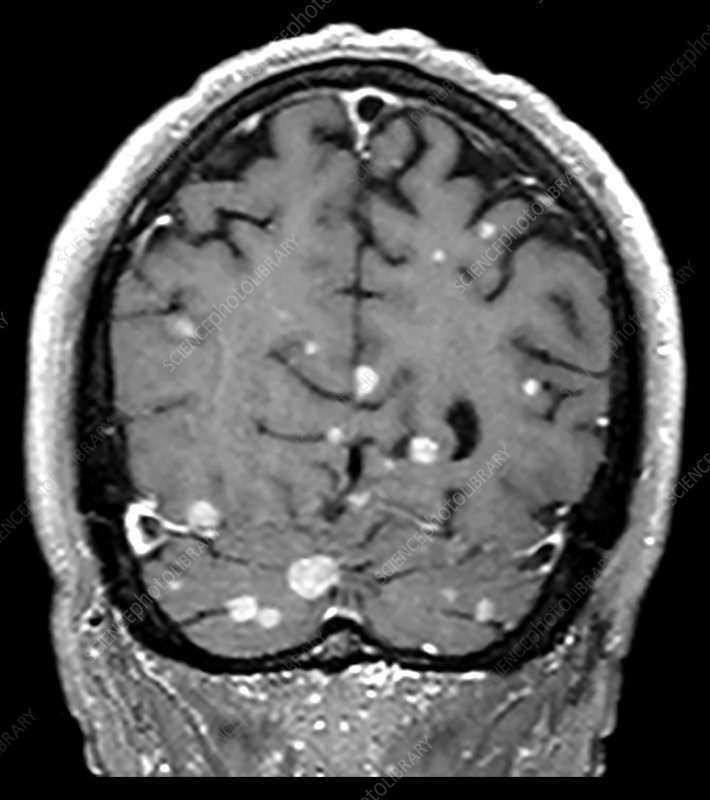
Metastatic melanoma in the brain
Figure 2. Metastatic melanoma in the brain
What Is A Brain Metastasis
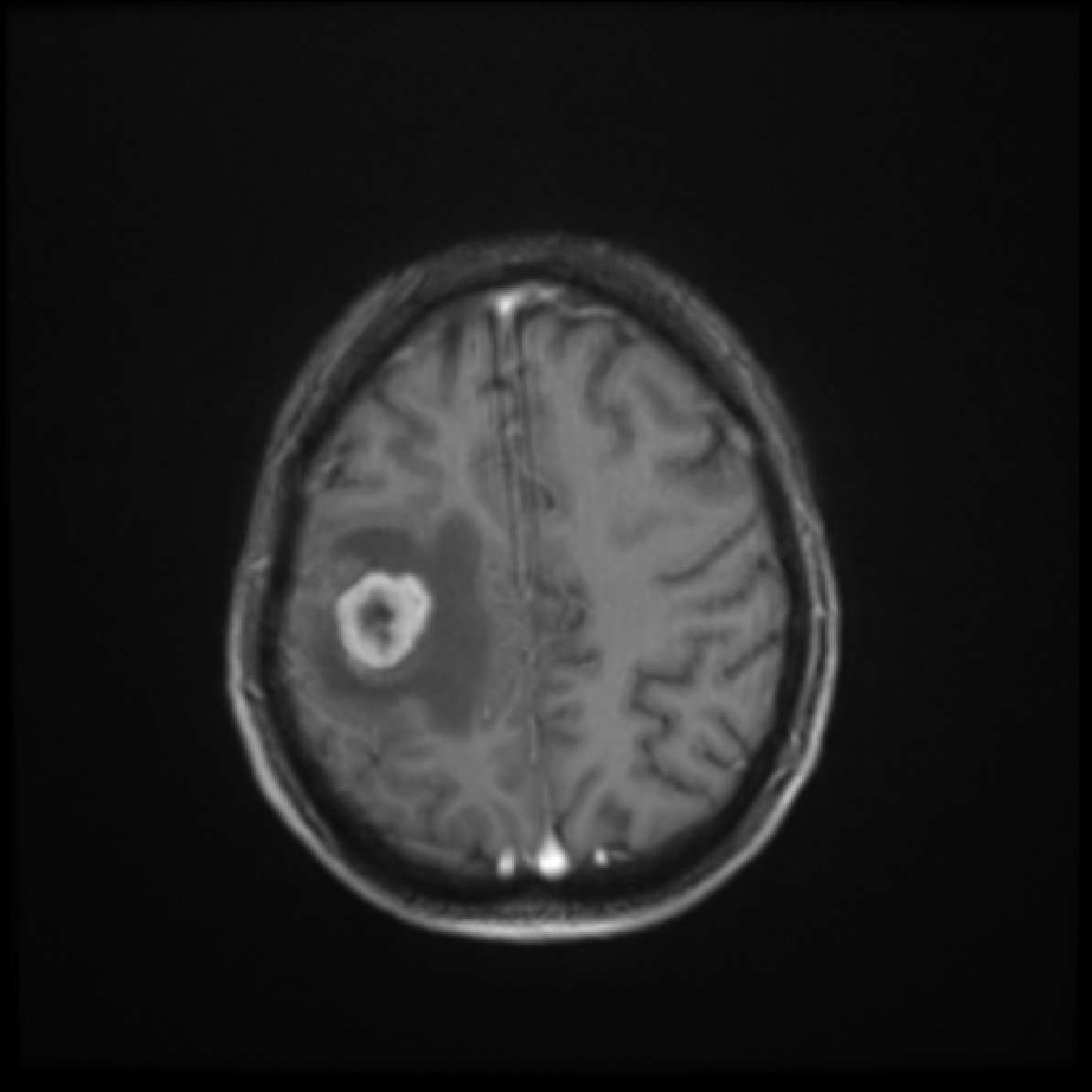
Metastatic brain tumors begin as cancer in another part of the body and spread to the brain through the blood stream. There can be one tumor or multiple tumors . The most common cancers that spread to the brain are lung , breast , skin melanoma , kidney and colon . A metastatic brain tumor may also be referred to as a secondary tumor. When a skin cancer metastasizes to the brain, this “brain tumor” is actually a mass of skin cancer cells .
Some brain metastases appear years after the primary cancer. Others metastasize so quickly that they are discovered before the primary cancer. If the primary cancer cannot be found, it is called an unknown primary. A diagnostic work-up with imaging scans may be done to look for the primary cancer site. Treatment options vary depending on the location and number of brain lesions along with the location and severity of the primary cancer.
You May Like: What Does Advanced Skin Cancer Look Like
Where Melanoma Is Most Likely To Metastasize
According to an article published on Verywell by Timothy Di Chiara, Ph.D., a research scientist specialized in oncology, the likelihood that melanoma will metastasize to each organ is as follows:
- Lymph Nodes: 70-75%
- Other areas of the skin, fat, and muscle: 65-70%
- Lungs and area of the lungs: 70-87%
- Liver and gallbladder: 54-77%
Treatment Of Brain Metastases
Steroid medicines, such as dexamethasone, are often used to reduce swelling in the brain around the metastases. This can often help with symptoms right away while further treatment is planned.
Anti-seizure medicines may also be used if a patient has had a seizure. This can help prevent more seizures.
Radiation therapy is often used to manage brain metastases and control symptoms. For people with several brain metastases or meningitis from cancer, whole brain radiation can be used. This can help improve symptoms and prevent them from getting worse.
Surgery is also sometimes used to treat brain metastases, especially if there are no more than three spots. For some people, a specialized procedure called stereotactic radiosurgery may be used. Either procedure is most often followed by whole brain radiation therapy for the best results.
Chemotherapy is not usually a treatment for brain metastases because these medicines have a hard time getting into the brain. However, for people with meningitis from cancer, chemotherapy may be injected right into the fluid that surrounds the brain and spinal cord. This can be done during a lumbar puncture or through a device called an Ommaya reservoir.
An Ommaya reservoir is a dome-like device that is placed under the skin of the head and accessed with a needle. If the patient has an Ommaya reservoir, they can get chemo into the fluid that surrounds the brain and spinal cord without having to get repeated lumbar punctures.
Also Check: How Quickly Can Melanoma Metastasis
How Fast Does Ocular Melanoma Spread
Ocular melanoma is an eye cancer characterized by overproduction and excess multiplication of pigment making cells in the eyes. It can affect various parts of the eyes, i.e., iris, ciliary body, and choroid. It mostly affects the eyeball. It can also develop in the eyelid or conjunctiva.
Metastatic melanoma is a general term used for cancer that grows beyond its original site. The liver is the most typical site where ocular melanoma tends to metastasize. It is found in clinical studies that when ocular melanoma progresses to metastatic disease, 90% of patients develop liver disease.
Although ocular melanoma is a progressive disease, it spreads slowly to distant parts of the body. Approximately 50% of patients with OM are likely to develop metastases in 10 to 15 years after its diagnosis. A small percentage of people may take 20-25 years after their initial diagnosis to establish metastases. Its metastatic nature shows it is a fatal disease. In most cases, it has a 50% mortality rate, which is not changed despite effective and modern treatment procedures employed for treating the primary eye tumor.
Although ocular melanoma is a rare cancer, it is the most common eye cancer. It is also reported that approximately 50% of people who are diagnosed with this type of cancer will develop metastatic disease. In 95% of the cases, the first organ affected by this cancer is the liver.
Symptoms Of Brain Metastases
Symptoms of brain metastases depend on the location, size and number of growths in the brain, or the amount of swelling. Metastases can push on or cause swelling in specific areas causing specific symptoms. Not everyone with a brain metastasis will have symptoms but most do.
The most common symptoms are:
- Headache
- Not being able to move parts of your body, like an arm or leg
- Sleepiness
- Changes in emotions or how a person acts
- Problems hearing, seeing, or swallowing
- Seizures
- Nausea or vomiting
You May Like: How Severe Is Skin Cancer
What Symptoms Develop When Melanoma Spreads To The Brain
Many patients feel the same. They dont have any symptoms that would indicate the cancer has spread.
If your doctor thinks that you are at risk for melanoma spreading to your brain, you may need an MRI. An MRI can find cancer in the brain before you have symptoms. Not everyone who has melanoma needs to have an MRI.
When melanoma spreads to the brain and symptoms occur, they may include:
-
Headaches
-
Paralysis on one side of your body
-
Problems with your eyesight
Symptoms tends to occur when the cancer has spread to more than one area of the brain. A large tumor can also cause symptoms.
Drug Combo Fights Melanoma That’s Spread To Brain
HealthDay Reporter
THURSDAY, Aug. 23, 2018 — A combination of two drugs that work with the immune system can help beat back melanoma that has moved to the brain, an early clinical trial has found.
The study included 94 patients with advanced melanoma that had invaded the brain. All were treated with two “immunotherapy” drugs — Opdivo and Yervoy — which help the immune system find and destroy tumors.
Overall, 57 percent of the patients saw their brain tumors disappear, shrink or remain stable for at least six months. For most, the responses were still evident at their latest follow-up, at the 14-month mark.
And after one year, more than 80 percent of all patients were still alive.
“That’s really tremendous,” said lead researcher Dr. Hussein Tawbi, of the University of Texas M.D. Anderson Cancer Center in Houston. “Without treatment, that rate would be about 20 percent.”
Experts said the findings represent another step forward against advanced melanoma, the deadliest form of skin cancer. Once melanoma spreads to distant sites in the body, the prognosis has traditionally been grim. When it infiltrates the brain, the typical life expectancy has hovered around four to five months, according to Tawbi.
But in recent years, several new drugs have been approved to fight advanced melanoma. They include Opdivo and Yervoy, which are already used in combination.
But major trials of the drugs, Tawbi said, have excluded patients with brain metastases .
New England Journal of Medicine
Don’t Miss: What Is Soft Tissue Carcinoma
What Else Should I Know About Treatment For Advanced Melanoma
Thanks to research breakthroughs, more patients diagnosed with advanced melanoma are living longer some for years.
Because these breakthrough are relatively recent, its important to:
-
Work with a team of melanoma specialists.
-
Ask your melanoma specialists if any of the newer treatments are appropriate for you.
-
Realize that no one treatment works for everyone, so you may need to try different treatments or combine treatments.
Researchers continue to study advanced melanoma, and next-generation treatments are now being studied in clinical trials. If you want to know whether you are a match for a trial, you can find out if there are any relevant trials at, Clinical Trial Finder.
Related AAD resources
ReferencesChukwueke U, Batchelor T, et al. Management of brain metastases in patients with melanoma. J Oncol Pract. 2016; 12:536-42.
Emory Medical Center. A year in the life: Jimmy Carter shares his cancer experience. Posted July 11, 2016. Last accessed March 26, 2018.
Podlipnik S, Carrera C, et al. Performance of diagnostic tests in an intensive follow-up protocol for patients with American Joint Committee on Cancer stage IIB, IIC, and III localized primary melanoma: A prospective cohort study. J Am Acad Dermatol. 2016; 75:516-24.
Nordmann N, Hubbard M, et al. Effect of gamma knife radiosurgery and programmed cell death 1 receptor antagonists on metastatic melanoma. Cureus. 2017; 9: e1943.
How Do You Treat Stage 4 Melanoma
The good news is that even stage 4 melanoma can be treated. The sooner the cancer is found, the sooner it can be removed and the higher your chances are for recovery. Stage 4 melanoma also has the most treatment options, but these options depend on:
- where the cancer is
- how advanced the cancer has become
- your age and overall health
How you respond to treatment also affects your treatment options. The five standard treatments for melanoma are:
- surgery: to remove the primary tumor and affected lymph nodes
- chemotherapy: a drug treatment to stop growth of cancer cells
- radiation therapy: the application of high-energy X-rays to inhibit growth and cancer cells
- immunotherapy: treatment to boost your immune system
- targeted therapy: the use of drugs or other substances to attack cancer drugs
Other treatments may also depend on where the cancer has spread to. Your doctor will discuss your options with you to help map out a treatment plan.
Don’t Miss: How Dangerous Is Skin Cancer On The Face
What You Need To Know
- Metastatic brain cancer is caused by cancer cells spreading to the brain from a different part of the body.
- The most common types of cancer that can spread to the brain are cancers of the lung, breast, skin , colon, kidney;and thyroid gland.
- Metastatic brain tumors are five times more common than primary brain tumors .
- Metastatic brain tumors can grow rapidly, crowding or destroying nearby brain tissue. Sometimes a patient may have multiple metastatic tumors in different areas of the brain.
Does Ocular Melanoma Spread To The Brain
However, it is found that ocular melanoma can spread to any organ in the body. After the liver, common sites where eye cancer cells can travel are the lung, brain, and bones. Around 50% of ocular melanoma patients will develop metastasis within 15 years of their original medical diagnosis. Once the liver is involved, cancer becomes incurable. However, if metastatic disease is detected in the early phase, there are a few localized and systemic treatment procedures available that may improve the life expectancy of the patient and help in the improvement of the lifestyle for patients.
Regardless of the treatment options selected, ocular melanoma may represent lasting complications, even for patients who have a good prognosis with cancer. Patients can develop glaucoma as its complication, which is caused by the pressure of tumors within the eye, leading to pain. If surgery is conducted to remove these cancer cells, patients may have the risk of full or segmented vision loss as the function of the cranial nerves that control the muscles around the eye may be lost. If the ocular melanoma spreads beyond the eye, the treatment depends on the site it has traveled. It gets more complicated to treat. While it most often affects the liver, in a few cases of metastasis, it can also go to the brain, which becomes more complicated to treat.
Don’t Miss: How Do You Die From Melanoma
Metastatic Brain Cancer Prognosis
Prognosis for metastatic brain cancer varies greatly. Keep in mind that each patient is unique, and with newer treatments, many patients live longer. Speaking with your care team about your unique diagnosis can provide an accurate prognosis.
Palliative Care at Johns Hopkins
Palliative care is specialized medical care that helps patients facing serious illnesses and their families by adding an extra layer of support.
Palliative care teams can help with the symptoms and the stress of living with a serious illness, including controlling pain, providing support for the mental and emotional effects of an illness, and managing other symptoms.
What Determines The Treatment Options And Prognosis For Patients With Brain Metastases
Certain characteristics of both the patient and the cancer will affect the patients prognosis as well as eligibility for treatment. The following factors are associated with better outcomes :
- Younger age: less than 60 years old
- Fewer vs. more brain metastases: fewer than three lesions
- No extracranial disease
- Normal LDH;
- Highgreater than 70Karnofsky Performance Status score
Read Also: What Is The Leading Cause Of Skin Cancer
Predictive Factors For Overall Survival
We analyzed the potential association between several factors and survival using univariate Cox regression of overall survival . Intriguingly, of factors in the primary tumor, increased levels of tumor-infiltrating lymphocytes showed a trend toward improved survival in patients with brain metastasis. Several clinical factors were found to be significantly associated with overall survival in patients with brain metastasis by univariate analysis . Factors associated with shorter overall survival included male sex, cerebellar involvement, higher number of metastatic brain tumors, concurrent presence of adrenal metastasis, or treatment with whole-brain radiation therapy. Factors associated with longer overall survival were treatment with craniotomy, stereotactic radiosurgery, or anti-PD-1 antibody therapy after initial diagnosis of brain metastasis.
Table 4 Univariate Cox regression analysis of association of various clinical factors with overall survival in melanoma patients with brain metastasis
Multivariate analysis of all eight factors revealed cerebellar involvement, craniotomy, and adrenal involvement as independently predictive of survival . There was trend toward significance for treatment with anti-PD-1 antibody .
Table 5 Multivariate Cox regression analysis of association of various clinical factors with overall survival in melanoma patients with brain metastasis