Treatment Of Melanoma With Braf Mutations
BRAF mutations are present in 60% of melanomas. Detection of this mutation is important prior to starting treatment in any melanoma patient. In a multicenter, phase I, dose-escalation trial, 32 patients with metastatic melanoma who had a BRAF mutation were treated with vemurafenib . Two patients had a complete response and 24 had a partial response.
First-line treatment of patients with BRAF V600 wild-type or mutation-positive, unresectable or metastatic melanoma is with nivolumab as a monotherapy or in combination with ipilimumab.
Vemurafenib was approved by the FDA in August 2011. It is an inhibitor of some mutated forms of BRAF serine-threonine kinase, including BRAF -V600E. This agent is indicated for the treatment of unresectable or metastatic melanoma with BRAF-V600 mutation as detected by the cobas 4800 BRAF V600 Mutation Test . Vemurafenib has not been studied with wild-type BRAF melanoma.
In May 2013 the FDA approved dabrafenib , a BRAF inhibitor in the same class as vemurafenib, for patients with unresectable or metastatic melanoma with BRAF V600E mutation confirmed by the THxID BRAF mutation test. In a multicenter, open-label, phase III randomized controlled trial, treatment with dabrafenib significantly improved progression-free survival in patients with BRAF-mutated metastatic melanoma, compared with dacarbazine .
How Immunotherapy Comes Into Play
Immunotherapy helps your natural immune system to attack cancer cells.
One group of immunotherapy drugs in particular has shown great promise for treating advanced-stage melanoma. These drugs are known as checkpoint inhibitors. They help the immune systems T cells recognize and attack melanoma cells.
Studies have found these medications improve survival rates for people with advanced-stage melanoma, report the authors of a review article in the American Journal of Clinical Dermatology. Research published in The Oncologist has also found that people with melanoma can potentially benefit from treatment with these drugs, regardless of their age.
But immunotherapy doesnt work for everyone. According to a research letter published in the journal Nature Medicine, only a portion of people with melanoma benefit from treatment with checkpoint inhibitors. More research is needed to learn which people are most likely to respond well to this treatment.
Where Research Is Headed
A 2017 review of phase III clinical trials found that current targeted therapies and immunotherapy work well to improve overall survival rates in people with advanced-stage melanoma. But the authors say that more research is needed to learn which therapy to try first.
Scientists are developing and testing strategies to identify which patients are most likely to benefit from which treatments. For example, researchers have found that people who have high levels of certain proteins in their blood may respond better than others to checkpoint inhibitors.
Studies are also underway to develop and test new therapies. According to an article in Gland Surgery, early research findings suggest that personalized anti-tumor vaccines may be a safe treatment approach. Scientists are also testing drugs that target melanoma with certain abnormal genes, reports the American Cancer Society.
New combinations of existing treatments might also help improve outcomes for some people with melanoma. Scientists are continuing to study the safety, efficacy, and optimal use of medications that have already been approved to treat this disease.
Also Check: Lobular Breast Cancer Stage 3
Treatment Of Stage I Melanoma
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of stage I melanoma may include the following:
- Surgery to remove the tumor and some of the normaltissue around it. Sometimes lymph node mapping and removal of lymph nodes is also done.
- A clinical trial of new ways to find cancercells in the lymph nodes.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Skin Exam And Physical
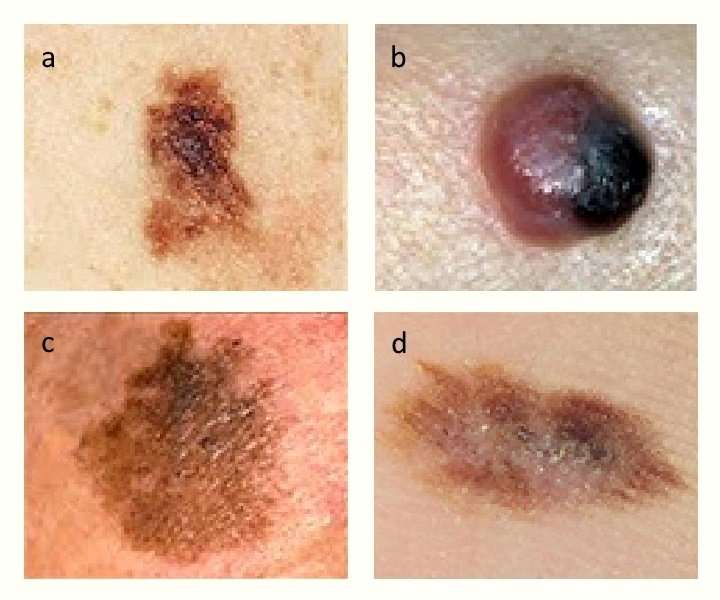
If youve been diagnosed with melanoma, youve already had a skin biopsy. This biopsy was taken when you had part of the suspicious spot removed. After it was removed, a doctor looked at the spot under a microscope to find out if it contained cancer cells. This is currently the only way to tell if someone has skin cancer.
After getting the diagnosis, the next step is to get a complete skin exam and physical.
During the physical, your dermatologist will feel your lymph nodes. This is where melanoma usually goes when it begins to spread. It usually travels to the lymph nodes closest to the melanoma.
If there is a risk the cancer could have spread, your dermatologist may recommend that you have a lymph node biopsy. If a sentinel lymph node biopsy is recommended, it can be performed at the time of your surgery for melanoma.
After the skin exam and physical, your dermatologist may recommend testing, such as a CAT scan, MRI, or a blood test. These can also help detect spread.
Read Also: What Does Stage 3b Melanoma Mean
Treating Stage Ii Melanoma
Wide excision is the standard treatment for stage II melanoma. The width of the margin depends on the thickness and location of the melanoma.
Because the melanoma may have spread to nearby lymph nodes, many doctors recommend a sentinel lymph node biopsy as well. This is an option that you and your doctor should discuss.
If an SLNB is done and does not find cancer cells in the lymph nodes, then no further treatment is needed, although close follow-up is still important.
If the SLNB finds that the sentinel node contains cancer cells, then a lymph node dissection will probably be done at a later date. Another option might be to watch the lymph nodes closely by getting an ultrasound of the nodes every few months.
If the SLNB found cancer, adjuvant treatment with an immune checkpoint inhibitor or targeted therapy drugs might be recommended to try to lower the chance the melanoma will come back. Other drugs or perhaps vaccines might also be options as part of a clinical trial.
Immunotherapy For Advanced Melanoma
Immunotherapy is a cancer treatment that stimulates the immune system to fight cancer anywhere in the body. This treatment may either be systemic, meaning that the drugs travel through the bloodstream, or local, injected into or near an accessible tumor.
Learn more about treatment options using immunotherapy for advanced melanoma.
You May Like: What Is The Survival Rate For Invasive Ductal Carcinoma
Clinical Trials For Melanoma
As part of our commitment to bringing patients new and innovative treatment options for melanoma and other cancers, Cancer Treatment Centers of America® may suggest clinical trials to qualifying patients.
In many cases, clinical trials are intended for patients with advanced cancer, those who have not responded to standard-of-care treatments or patients who may have run out of other treatment options. However, patients may qualify for a clinical trial at any stage of their disease and/or treatment.
Talk to your doctor about whether a clinical trial is an option for you and ask about the risks and requirements involved.
Unusual Moles Exposure To Sunlight And Health History Can Affect The Risk Of Melanoma
Anything that increases your risk of getting a disease is called a risk factor. Having a risk factor does not mean that you will get cancer not having risk factors doesn’t mean that you will not get cancer. Talk with your doctor if you think you may be at risk.
Risk factors for melanoma include the following:
- Having a fair complexion, which includes the following:
- Fair skin that freckles and burns easily, does not tan, or tans poorly.
- Blue or green or other light-colored eyes.
- Red or blond hair.
Being White or having a fair complexion increases the risk of melanoma, but anyone can have melanoma, including people with dark skin.
See the following PDQ summaries for more information on risk factors for melanoma:
Don’t Miss: Skin Cancer Metastasis To Lymph Nodes
Prevention Of Malignant Melanoma
The focus of melanoma prevention is avoidance of sun exposure. Everyone, especially those individuals at high risk of developing a melanoma, should wear protective clothing, avoid peak sun hours, protect children against exposure to ultraviolet radiation, avoid tanning booths, and wear sunscreen with a sun protection factor of at least 15.
This last recommendation is considered somewhat controversial, because no study has shown sunscreen to reduce the incidence of melanoma. Moreover, a systematic review found that sunscreen use leads to longer duration of intentional sun exposure, and sunburns tend to be more frequent among sunscreen users.
In addition, a study of 499 white children who were enrolled at birth or at age 6 and stratified colorimetrically by skin tone found no association between sunscreen use and the overall number of moles at the age of 15 years. The only significant association was for lighter-skinned children who had at least three sunburns at 12 to 14 years old, who had fewer moles if they used sunscreen. However, even that association might have occurred by chance.
First-degree relatives of a patient diagnosed with familial melanoma should be encouraged to have annual skin examinations.
Researchers Identify Possible New Combination Treatment For Advanced Melanoma
by University of California, Los Angeles
A study by researchers at the UCLA Jonsson Comprehensive Cancer Center suggests that using an immunotherapy drug called NKTR-214, also known as bempegaldesleukin, in combination with an infusion of anti-tumor immune cells, or T cells, may produce a stronger immune response that could help fight advanced melanoma.
When tested in mice with melanoma tumors that were unlikely to stimulate an immune response, the approach increased the number of anti-tumor immune cells, and those immune cells lived longer and functioned better than the standard therapy, empowering the cells to destroy the tumor.
Adoptive cell therapy is a type of immunotherapy that has had promising results for treating people with advanced cancers. The approach involves extracting and harvesting immune cells from a patient and engineering them in the laboratory to attack specific antigens on the surface of tumors. One challenge is that it requires giving patients interleukin 2, a protein signaling molecule in the immune system, to promote the development and expansion of the infused immune cells. But interleukin 2 can also activate cells to suppress the immune system, and because it is highly toxic, it can have serious adverse side effects.
Researchers have been seeking ways to produce large number of immune cells without exposing patients to those negative side effectsincluding by combining adoptive cell therapy with other treatments.
Explore further
Read Also: What Stage Is Invasive Lobular Carcinoma
What Are The Signs Of Symptoms Of Metastatic Melanoma
Signs and symptoms depend upon the site of metastasis and the amount of tumor there. Metastases to the brain may first appear as headaches, unusual numbness in the arms and legs, or seizures. Spread to the liver may be first identified by abnormal blood tests of liver function long before the patient has jaundice, a swollen liver, or any other signs of liver failure. Spread to the kidneys may cause pain and blood in the urine. Spread to the lungs may cause shortness of breath, other trouble breathing, chest pain, and continued cough. Spread to bones may cause bone pain or broken bones called pathologic fractures. A very high tumor burden may lead to fatigue, weight loss, weakness and, in rare cases, the release of so much melanin into the circulation that the patient may develop brown or black urine and have their skin turn a diffuse slate-gray color. The appearance of multiple blue-gray nodules in the skin of a melanoma patient may indicate widespread melanoma metastases to remote skin sites.
Remission And The Chance Of Recurrence
A remission is when cancer cannot be detected in the body and there are no symptoms. This may also be called having no evidence of disease or NED.
A remission may be temporary or permanent. This uncertainty causes many people to worry that the cancer will come back. While many remissions are permanent, it is important to talk with your doctor about the possibility of the cancer returning. Understanding your risk of recurrence and the treatment options may help you feel more prepared if the cancer does return. Learn more about coping with the fear of recurrence.
If the melanoma returns after the original treatment, it is called recurrent cancer. It may come back in the same place , nearby , or in another part of the body .
When this occurs, a new cycle of testing will begin to learn as much as possible about the recurrence. After this testing is done, you and your doctor will talk about the treatment options. Often the treatment plan will include the treatments described above, such as surgery, chemotherapy, immunotherapy, targeted therapy, and radiation therapy, but they may be used in a different combination or given at a different pace. Your doctor may suggest clinical trials that are studying new ways to treat this type of recurrent cancer. Whichever treatment plan you choose, palliative care will be important for relieving symptoms and side effects.
Don’t Miss: Can You Die From Basal Cell Skin Cancer
Treating Stage 3 Melanoma
If the melanoma has spread to nearby lymph nodes , further surgery may be needed to remove them.
Stage 3 melanoma may be diagnosed by a sentinel node biopsy, or you or a member of your treatment team may have felt a lump in your lymph nodes.
The diagnosis of melanoma is usually confirmed using a needle biopsy .
Removing the affected lymph nodes is done under general anaesthetic.
The procedure, called a lymph node dissection, can disrupt the lymphatic system, leading to a build-up of fluids in your limbs. This is known as lymphoedema.
Cancer Research UK has more information about surgery to remove lymph nodes.
New Treatments In Clinical Trials
Clinical trials are currently underway to test new treatments for nodular melanoma. These treatments are not yet available to the public.
One treatment that is currently undergoing clinical trials is vaccine therapy. This involves using certain substances to help stimulate the immune system. Once the vaccine therapy has been administered, the stimulated immune system can then locate and kill tumors in the body.
This treatment is being studied for the treatment of stage 3 melanoma that cant be effectively treated through surgery.
In some cases, participating in a clinical trial may be the best treatment option for a person with cancer. In a clinical trial, a cancer patient may be one of the first to receive a new treatment.
If you have advanced nodular melanoma and are interested in participating in a clinical trial, you should speak with your healthcare team about the options being studied and what might work for you.
You May Like: Squamous Cell Carcinoma Scalp Prognosis
Finding Melanoma Clinical Trials
There are many ways you can learn more about available clinical trials, which centers of excellence are participating in clinical trials, and how to enroll in a trials however, two of the easiest are noted below:
1. The MRFs Clinical Trial Finder, hosted through our partner, EmergingMed, can provide you with a free, confidential, personalized service that helps you understand which trials may be an option for you. For best results, we recommend that you register and complete the profile information. This helps ensure you learn of the best possible trials for you.
Biological Therapies And Melanoma
Biological therapies are treatments using substances made naturally by the body. Some of these treatments are called immunotherapy because they help the immune system fight the cancer, or they occur naturally as part of the immune system. There are many biological therapies being researched and trialled, which in the future may help treat people with melanoma. They include monoclonal antibodies and vaccine therapy.
Also Check: Etiology Of Skin Cancer
Thinking About Taking Part In A Clinical Trial
Clinical trials are carefully controlled research studies that are done to get a closer look at promising new treatments or procedures. Clinical trials are one way to get state-of-the art cancer treatment. In some cases they may be the only way to get access to newer treatments. They are also the best way for doctors to learn better methods to treat cancer. Still, they’re not right for everyone.
If you would like to learn more about clinical trials that might be right for you, start by asking your doctor if your clinic or hospital conducts clinical trials.
Neoadjuvant Treatments For Resectable Melanoma
Some stage III and stage IV melanoma tumors are resectable, meaning they can be removed by surgery. In other types of cancer, neoadjuvant treatment of resectable tumors is known to reduce the risk of recurrence after surgery. It took additional time to explore ICI and targeted drugs in the neoadjuvant setting in melanoma. Now, several clinical trials have addressed the potential of using these drugs to prolong relapse-free survival after resection.
A recent analysis of results from six of these trials addressed the rate of pathologic complete response after treatmenta term that describes elimination of cancer cells prior to surgery. pCR has already been associated with better RFS in other cancers. In the six trials evaluated, pCR was achieved in 47% of melanoma patients who received targeted drugs and in 33% of patients receiving ICI. However, RFS at two years after surgery was 79% for patients who received BRAF/MEK inhibitors and 96% for patients who received ICI.
Overall, these data strongly support the use of neoadjuvant treatment in melanoma, and there are now nearly 20 ongoing trials testing this strategy.
Also Check: What Is The Survival Rate For Invasive Ductal Carcinoma