How Often Should You Follow Up With Your Doctor
After your treatment, your doctor will recommend a regular follow-up schedule to monitor your cancer. Theyll be checking to make sure the cancer hasnt come back or new cancerous lesions havent appeared. The types of follow-up include:
A yearly skin check: Skin checks are an important aspect of detecting melanoma in its earliest, most treatable stages. You should also conduct a skin check on yourself once per month. Look everywhere from the bottoms of your feet to behind your neck.
Imaging tests every three months to a year: Imaging studies, such as an X-ray, CT scan, or brain MRI, look for cancer recurrence.
Physical exam as needed: A physical exam to assess your overall health is important when you have had melanoma. For the first two years, youll want to get an exam every three to six months. Then for the next three years, the appointments can be every three months to a year. After the fifth year, the exams can be as needed. Do a monthly self-examination of your lymph nodes to check your progress.
Your doctor may recommend a different schedule based on your overall health.
The Braf Gene Mutation And Melanoma
Roughly half of all documented melanoma cases present with mutations in the BRAF gene. The melanoma cells that have these changes create a BRAF protein, which aids them in their growth. If a person with the BRAF gene mutation has melanoma, knowing about the mutation is of great benefit for treatment because healthcare providers can use targeted therapy to inhibit the BRAF gene mutation from aiding in the growth of the cancer.
If a diagnosis of melanoma is already established, the healthcare provider will look at two factors to determine how advanced a stage 4 melanoma has become: the location of the distant tumors and an elevated level of serum lactate dehydrogenase , which is an enzyme responsible for turning sugar into energy. The higher the LDH level in body fluids, the more damage the cancer has done.
Presentation And Clinical Signs Of Omm
Affected dogs may be asymptomatic. In these cases, an oral mass is often discovered by the owner or during a routine physical examination or dental prophylactic procedure. Clinical signs of OMM include halitosis, excessive drooling, bleeding from the oral cavity, dysphagia, facial swelling, and pain on mouth manipulation.4,7,8 OMMs are often pigmented , but up to 38% can be amelanotic.9 The most common locations are the gingiva, lips, tongue, and hard palate.3,4,10
Recommended Reading: Does Amelanotic Melanoma Blanch When Pressed
How Is Pediatric Melanoma Diagnosed
A proper diagnosis is essential for selecting the best treatment. The diagnosis of skin melanoma can only be made with a biopsy, which is then examined under a microscope by a pathologist. Pathologists who specialize in looking at skin biopsies are called dermatopathologists, but even board-certified dermatopathologists may not have extensive expertise in recognizing melanoma in children. In addition, even expert dermatopathologists sometimes disagree about the classification of a childs mole as benign, atypical or malignant. It is important to be sure that an expert dermatopathologist has looked at your childs biopsy, and you especially need to know if there is some degree of uncertainty about whether the mole is benign, atypical or malignant. Sometimes, highly specialized diagnostic tests like FISH and CGH are used to better classify pediatric lesions.
Because pediatric melanoma is difficult to diagnose, the diagnosis can sometimes be delayed or misdiagnosed. Most doctors dont expect it, and some types of pediatric melanoma look different than adult melanoma. Sometimes pediatric melanoma is misdiagnosed as pyogenic granulomas, atypical melanocytic neoplasms, warts or spitz nevi.
Melanoma does not discriminate NEVER LET A DOCTOR TELL YOU THAT YOUR CHILD IS TOO YOUNG TO GET MELANOMA.
S Of Melanoma That Youve Probably Never Seen

Look over the images. Some are not what youll be expecting.
CDC, Carl Washington, MD, Emory Univ. School of Medicine, Mona Saraiya, MD, MPH
Dr. Mamelakfocuses on the full breadth of dermatologic care, from cosmetic skin solutions to advanced skin cancer removal. Hes founder of the Austin Mohs Surgery Center, which is dedicated to the treatment and management of skin cancer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. Shes also a former ACE-certified personal trainer.
Top image: Cancer Research UK
Recommended Reading: Stage 3 Basal Cell Carcinoma Survival Rate
Where To Find Support For Stage 3 Melanoma
With a melanoma diagnosis, its important to reach out to those close to you during your treatment. In addition to family and friends, there are many support groups and resources who can help answer questions or provide a listening ear.
Find a melanoma support group. The American Melanoma Foundation maintains a list of support groups throughout the country find them by .
Join an online support group. If you feel more comfortable participating in an online support group, the AIM at Melanoma Foundation offers a support community as well as counseling.
Seek financial assistance, if needed. The Melanoma Research Foundation has developed a central resource for patient assistance programs and government entities that offer financial assistance for those with melanoma. For more information, please .
Sign up for a mentoring program. Olympic figure skater Scott Hamiltons charity, 4th Angel, offers a mentoring program for those with cancer. This telephone-based program is designed to provide support and encouragement to those with cancer.
Many organizations provide professional and supportive services when youve been diagnosed with melanoma. Other organizations that provide support for those with skin cancer include the:
What Is The Incidence Of Melanoma
It is the sixth most common cancer in the United States, and currently is the cancer with the most rapid rise in incidence in the United States. The lifetime risk in the year 2000 was 1 in 75 versus 1 in 150 in 1985. Over 59,000 new cases of melanoma are reported each year with more than 8000 deaths from the disease.
Also Check: What Does Merkel Cell Skin Cancer Look Like
You May Like: Soderstrom Skin Cancer Screening
Two Big Warning Signs Of Nail Melanoma
Hutchinsons sign. The Hutchinsons sign is when the pigment in the nail extends to the nail fold , says Dr. Ilyas. This sign is considered ominous for a melanoma of the nail.
Hutchinsons sign. The pigment is leaking into the skin near the cuticle.
Whats even scarier is that a benign pigment in the nail bed can create a pseudo-Hutchinsons sign.
To a layperson, this appears to be a true Hutchinsons sign. But a dermatologist knows what to look for that would indicate a benign finding.
Nevertheless, if you see what seems to be the Hutchinsons sign get to a dermatologist.
Progression and evolution. Dr. Ilyas explains, Pigment or color that extends or spreads over time is concerning for a melanoma.
The obvious progression in this case is the destruction of the top corner of the nail which is right above an obvious Hutchinsons sign. Ann Dermatol. 2018 Feb 30
It is not uncommon for people to present with a benign pigmented streak of the nail.
These tend to have clear defined edges, not extend to the nail fold, and stay stable, says Dr. Ilyas.
If the color of this streak starts to become hazy along the edges or darker over time, this can be suspicious for a cancer and should be evaluated.
Subungual Melanoma: Exact Location of Tumor
The tumor is not literally IN the nail that part of the finger or toe that you trim or paint.
The cancer is actually underneath the nail, in the matrix, and it shows through the nail.
Mixed Red And White Patches
A mixture of red and white patches in your mouth, called erythroleukoplakia, is an abnormal cell growth thats more likely to become cancerous. If red and white patches last more than two weeks, you should see your dentist. You may see these mouth abnormalities before you feel them. In the early stages, mouth cancer may cause no pain.
Bright red patches in your mouth that look and feel velvety are called erythroplakia. They are often precancerous.
Recommended Reading: Can You See Skin Cancer
Recommended Reading: Osteomyoma
What Tests Are Used To Stage Melanoma
There are several tests your doctor can use to stage your melanoma. Your doctor may use these tests:
- Sentinel Lymph Node Biopsy: Patients with melanomas deeper than 0.8 mm, those who have ulceration under the microscope in tumors of any size or other less common concerning features under the microscope, may need a biopsy of sentinel lymph nodes to determine if the melanoma has spread. Patients diagnosed via a sentinel lymph node biopsy have higher survival rates than those diagnosed with melanoma in lymph nodes via physical exam.
- Computed Tomography scan: A CT scan can show if melanoma is in your internal organs.
- Magnetic Resonance Imaging scan: An MRI scan is used to check for melanoma tumors in the brain or spinal cord.
- Positron Emission Tomography scan: A PET scan can check for melanoma in lymph nodes and other parts of your body distant from the original melanoma skin spot.
- Blood work: Blood tests may be used to measure lactate dehydrogenase before treatment. Other tests include blood chemistry levels and blood cell counts.
What Is Metastaticmelanoma
Melanoma is a type of skin cancer that develops from the pigment-producing cells of the skin, mucosa, eye, and rarely other sites. Metastatic melanoma is melanoma that has spread to other sites of the body. The spread occurs through the lymphatic system and/or the blood vessels. Melanoma can spread to the subcutaneous tissue which lies underneath the skin, the lymph nodes, and to other organs such as the lungs, liver, bone or brain.
Metastatic melanoma can be classified into local recurrence, in transit metastasis, nodal metastasis, and haematogenous spread.
Also Check: Basal Skin Cancer Survival Rates
Treating Stage 0 Melanoma
Stage 0 melanoma has not grown deeper than the top layer of the skin . It is usually treated by surgery to remove the melanoma and a small margin of normal skin around it. The removed sample is then sent to a lab to be looked at with a microscope. If cancer cells are seen at the edges of the sample, a second, wider excision of the area may be done.
Some doctors may consider the use of imiquimod cream or radiation therapy instead of surgery, although not all doctors agree with this.
For melanomas in sensitive areas on the face, some doctors may use Mohs surgery or even imiquimod cream if surgery might be disfiguring, although not all doctors agree with these uses.
Treating Stage Ii Melanoma
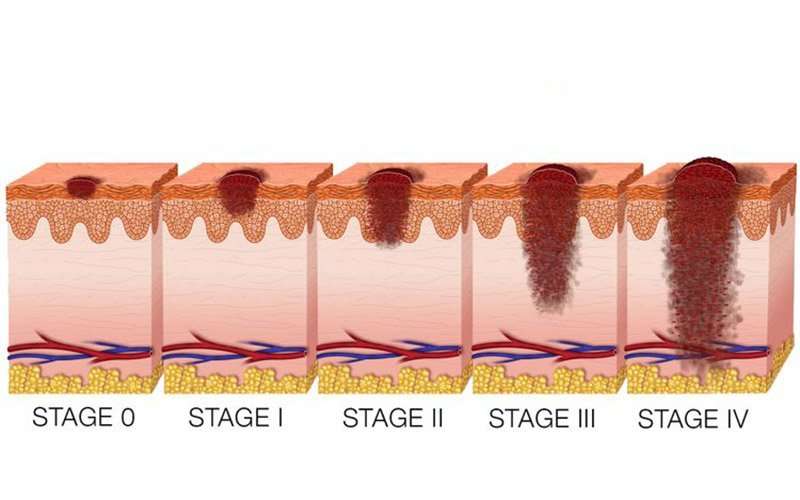
Wide excision is the standard treatment for stage II melanoma. The width of the margin depends on the thickness and location of the melanoma.
Because the melanoma may have spread to nearby lymph nodes, many doctors recommend a sentinel lymph node biopsy as well. This is an option that you and your doctor should discuss.
If an SLNB is done and does not find cancer cells in the lymph nodes, then no further treatment is needed, although close follow-up is still important.
If the SLNB finds that the sentinel node contains cancer cells, then a lymph node dissection will probably be done at a later date. Another option might be to watch the lymph nodes closely by getting an ultrasound of the nodes every few months.
If the SLNB found cancer, adjuvant treatment with an immune checkpoint inhibitor or targeted therapy drugs might be recommended to try to lower the chance the melanoma will come back. Other drugs or perhaps vaccines might also be options as part of a clinical trial.
You May Like: Does Amelanotic Melanoma Blanch When Pressed
Treating Stage I Melanoma
Stage I melanoma is typically treated by wide excision . The width of the margin depends on the thickness and location of the melanoma. Most often, no other treatment is needed.
Some doctors may recommend a sentinel lymph node biopsy to look for cancer in nearby lymph nodes, especially if the melanoma is stage IB or has other characteristics that make it more likely to have spread. You and your doctor should discuss this option.
If the SLNB does not find cancer cells in the lymph nodes, then no further treatment is needed, although close follow-up is still important.
If cancer cells are found on the SLNB, a lymph node dissection might be recommended. Another option might be to watch the lymph nodes closely by getting an ultrasound of the nodes every few months.
If the SLNB found cancer, adjuvant treatment with an immune checkpoint inhibitor or targeted therapy drugs might be recommended to try to lower the chance the melanoma will come back. Other drugs or perhaps vaccines might also be options as part of a clinical trial.
I’ve Been Diagnosed With Melanomawhat Happens Next
Doctors use the TNM system developed by the American Joint Committee on Cancer to begin the staging process. Its a classification based on three key factors:
T stands for the extent of the original tumor, its thickness or how deep it has grown and whether it has ulcerated.
What Is Breslow depth?
Breslow depth is a measurement from the surface of the skin to the deepest component of the melanoma.
Tumor thickness: Known as Breslow thickness or Breslow depth, this is a significant factor in predicting how far a melanoma has advanced. In general, a thinner Breslow depth indicates a smaller chance that the tumor has spread and a better outlook for treatment success. The thicker the melanoma measures, the greater its chance of spreading.
Tumor ulceration: Ulceration is a breakdown of the skin on top of the melanoma. Melanomas with ulceration are more serious because they have a greater risk of spreading, so they are staged higher than tumors without ulceration.
N indicates whether or not the cancer has already spread to nearby lymph nodes. The N category also includes in-transit tumors that have spread beyond the primary tumor toward the local lymph nodes but have not yet reached the lymph nodes.
M represents spread or metastasis to distant lymph nodes or skin sites and organs such as the lungs or brain.
After TNM categories are identified, the overall stage number is assigned. A lower stage number means less progression of the disease.
Recommended Reading: Squamous Cell Carcinoma Skin Metastasis
Oral Cancer Outlook: What To Expect If Youve Been Diagnosed
Life changes all of a sudden after an oral cancer diagnosis. Youll likely be worried about how the diagnosis will affect your physical and emotional health. At the same time, youre also confronted with the need to grasp whats happening and to make decisions about your treatment plan.
Read Also: What Are The Forms Of Skin Cancer
Red Flag #: Headaches Or Visual Changes
Just like the liver, not everyone will notice symptoms of melanoma spreading to the brain. But when symptoms do show up, its usually in the form of headaches, problems with eyesight, paralysis on one side of the body, or seizures. If someone simply has a headache, that doesnt mean they have advanced stage melanoma, Dr. Yushak says. But if its a headache thats not going away after a week, and you never have headaches, then thats something that definitely needs to be checked out.
Read Also: Does Skin Cancer Burn And Itch
Why Should You Seek Out A Dermatologist
Seek a professional opinion to rule out melanoma. If you notice one or more melanoma symptoms, contact Schaumburg Dermatology to set up an appointment. If the pathology lab identifies a pimple or mole as cancerous, we will develop a treatment plan to isolate and remove the skin cancer. Give us a call today at 497-8679 to set up a consultation.
Copyright © 2021 All Rights Reserved Schaumburg DermatologyPowered by Launch Digital Marketing
Visitor policies continue to evolve at Schaumburg Dermatology to ensure a safe, trusted, and comfortable care environment for all patients, visitors, physicians, and staff.
To align with recent changes made by the CDC, Schaumburg Dermatology updated our patient/visitor policy.
Effective 08/03/20211, the following visitor policies are in effect.
Screen for illness, At the point of check-in, patients and companions will be screened for COVID-19 symptoms by answering the screening questions below:
All guests who do not comply with the masking policy may be asked to leave.
Other Things To Know About Acral Lentiginous Melanoma
As an ALM tumor increases in size, it usually becomes more irregular in shape and color .
The surface of the ALM lesion may remain flat, even as the tumor invades deeply into the skin.
Thickening ALM on the sole of the foot can make walking painful and be mistaken for a plantar wart.
The surface of a spot of ALM may also start out smooth and become bumpier or rougher as it evolves. If a tumor begins to grow from the cancerous skin cells, the skin will become more bulbous, discolored, and rough to the touch.
Less advanced cancers and thinner tumors have better survival rates. Raised tumors tend to be more aggressive.
Men are more likely than women to have thick, large tumors at diagnosis.
Read Also: Is Skin Cancer Always Visible
Don’t Miss: Etiology Of Basal Cell Carcinoma
When Is A Mole A Problem
If a new or existing mole begins to change shape, color, size, or becomes flaky, crusty, or begins to bleed, its time to make an appointment with your dermatologist to get it checked out. A mole can turn into melanoma on rare occasions. In early melanoma, the shape of a mole becomes asymmetrical and uneven.
This photo contains content that some people may find graphic or disturbing.
Nodular basal cell carcinoma is a type of skin cancer that is most often found on the head. This type of cancer starts in basal cells, which are tasked with making new skin cells to push the old ones toward the surface of the skin. Nodular basal cell carcinoma is responsible for 60%-80% of all basal cell carcinomas. In the United States, its estimated that 4.3 million cases of basal cell carcinoma are diagnosed every year, with 2.5 to 3.4 million of those cases being nodular basal cell carcinoma.
This type of cancer appears as a pearl-like papule that is round and surrounded by threadlike red lines on the skin made up of tiny blood vessels. The risk of developing nodular basal cell carcinoma can be increased by spending a lot of time out in the sun, living in high-altitude and sunny locations, and radiation therapy.
Other risk factors include:
- Prolonged exposure to arsenic
- Certain rare genetic disorders such as basal cell nevus syndrome
Although this type of cancer is common, it is highly treatable, and the five-year relative survival rate is 100%.