Screening For Skin Cancer
Again, the best way to screen for skin cancer is knowing your own skin. If you are familiar with the freckles, moles, and other blemishes on your body, you are more likely to notice quickly if something seems unusual.
To help spot potentially dangerous abnormalities, doctors recommend doing regular self-exams of your skin at home. Ideally, these self-exams should happen once a month, and should involve an examination of all parts of your body. Use a hand-held mirror and ask friends or family for help so as to check your back, scalp, and other hard-to-see areas of skin. If you or someone else notices a change on your skin, set up a doctors appointment to get a professional opinion.
Reducing The Risk Of Breast Cancer Including Paget’s Disease Of The Nipple
Modifying certain lifestyle factors, such as reducing the amount of alcohol you drink and making sure you exercise regularly, may reduce your risk of developing certain types of cancer, including breast cancer.
Breast cancer screening is also used to help detect breast cancer early. In the UK, the NHS Breast Screening Programme provides free breast screening every 3 years for all women aged 50 to 70.
In some areas, women aged 47 to 49 and 71 to 73 are also invited for screening as part of a study looking at whether the age range for breast screening should be extended.
Page last reviewed: 22 October 2019 Next review due: 22 October 2022
How Is Inflammatory Breast Cancer Diagnosed
Inflammatory breast cancer can be difficult to diagnose. Often, there is no lump that can be felt during a physical exam or seen in a screening mammogram. In addition, most women diagnosed with inflammatory breast cancer have dense breast tissue, which makes cancer detection in a screening mammogram more difficult. Also, because inflammatory breast cancer is so aggressive, it can arise between scheduled screening mammograms and progress quickly. The symptoms of inflammatory breast cancer may be mistaken for those of mastitis, which is an infection of the breast, or another form of locally advanced breast cancer.
To help prevent delays in diagnosis and in choosing the best course of treatment, an international panel of experts published guidelines on how doctors can diagnose and stage inflammatory breast cancer correctly. Their recommendations are summarized below.
Minimum criteria for a diagnosis of inflammatory breast cancer include the following:
- A rapid onset of erythema , edema , and a peau d’orange appearance and/or abnormal breast warmth, with or without a lump that can be felt.
- The above-mentioned symptoms have been present for less than 6 months.
- The erythema covers at least a third of the breast.
- Initial biopsy samples from the affected breast show invasive carcinoma.
Imaging and staging tests include the following:
Recommended Reading: How To Identify Skin Cancer On Leg
Common Skin Cancer Can Signal Increased Risk Of Other Cancers
Frequent skin cancers due to mutations in genes responsible for repairing DNA are linked to a threefold risk of unrelated cancers, according to a Stanford study. The finding could help identify people for more vigilant screening.
Basal cell carcinomas are common. More than 3 million cases a year are diagnosed nationwide.jax10289/Shutterstock.com
People who develop abnormally frequent cases of a skin cancer known as basal cell carcinoma appear to be at significantly increased risk for developing of other cancers, including blood, breast, colon and prostate cancers, according to a preliminary study by researchers at the Stanford University School of Medicine.
The increased susceptibility is likely caused by mutations in a panel of proteins responsible for repairing DNA damage, the researchers found.
We discovered that people who develop six or more basal cell carcinomas during a 10-year period are about three times more likely than the general population to develop other, unrelated cancers, said Kavita Sarin, MD, PhD, assistant professor of dermatology. Were hopeful that this finding could be a way to identify people at an increased risk for a life-threatening malignancy before those cancers develop.
Sarin is the senior author of the study, which was published online Aug. 9 in JCI Insight. Medical student Hyunje Cho is the lead author.
Fungating Wounds From Secondary Tumours
A secondary tumour is a tumour that has spread from a primary site to other parts of the body.
A tumour that spreads to the blood and lymphatic system can travel to the skin. It can develop into an ulcerating tumour, but this is rare.
Always attend follow up appointments after your treatment has finished. This way your doctor can pick up any early signs of problems.
Contact your doctor between follow up appointments if you are worried. You should especially do so if you have any new symptoms, such as unexplained skin lumps or sores.
Also Check: Can Skin Cancer Be Cured
Is Sun Exposure The Only Cause Of Skin Cancer
Skin cancer is one of the most common and treatable forms of cancer when caught in the early stages. Any person can develop skin cancer, but the cause depends on the type of cancer diagnosed as well as the persons skin type. People with lighter colored hair, eyes, and skin have a greater risk of developing skin cancer because their body contains less melanin that protects them from sun damage. Continuous exposure to the sun without the protection of sunscreen, hats, lightweight long-sleeved clothing, and other barriers increase the risk of developing skin cancer as well.
Although long-term, unprotected sun exposure is a leading cause of skin cancer, its not the only cause. It depends largely on whether a doctor diagnoses a non-melanoma or melanoma type of skin cancer.
Axillary Basal Cell Carcinoma: A Need For Full Cutaneous Examination
JOSEPH C. ENGLISH III, M.D., Brooke Army Medical Center/Wilford Hall Air Force Medical Center, San Antonio, Texas
DANIEL R. CANCHOLA, M.D., University of Texas Health Science Center, San Antonio, Texas
ERIC M. FINLEY, M.D., Brooke Army Medical Center/Wilford Hall Air Force Medical Center, San Antonio, Texas
Am Fam Physician. 1998 Apr 15 57:1860-1864.
Basal cell carcinoma is the most common skin malignancy. While this lesion most often occurs in sun-exposed areas of the skin, it can also develop in sites that are not usually exposed to sunlight or artificial ultraviolet radiation, such as the breast, palm or groin. A periodic complete examination of the skin should be performed to ensure that atypical presentations of basal cell carcinoma are not overlooked or misdiagnosed. Treatment options include curettage and desiccation, cryosurgery, surgical excision, radiotherapy and Mohs micrographic surgery.
More than 900,000 cases of nonmelanoma skin cancer are estimated to occur annually.1 Basal cell carcinoma is the most common of these lesions. In the general population, the estimated lifetime risk of developing this malignancy is 28 to 33 percent.1 Although basal cell carcinoma can occur in younger persons, it usually develops after the age of 50 years.2 Up to 85 percent of basal cell carcinomas are found in the head and neck region,3 but the lesions occasionally occur in unusual and routinely photo-protected locations.49
Risk Factors for Basal Cell Carcinoma
Also Check: Do I Have Basal Cell Carcinoma
Who Gets Skin Cancer And Why
Sun exposure is the biggest cause of skin cancer. But it doesn’t explain skin cancers that develop on skin not ordinarily exposed to sunlight. Exposure to environmental hazards, radiation treatment, and even heredity may play a role. Although anyone can get skin cancer, the risk is greatest for people who have:
- Fair skin or light-colored eyes
- An abundance of large and irregularly-shaped moles
- A family history of skin cancer
- A history of excessive sun exposure or blistering sunburns
- Lived at high altitudes or with year-round sunshine
- Received radiation treatments
Outlook For Squamous Cell Breast Carcinoma
Generally speaking, squamous cell breast carcinoma has an aggressive clinical course, with an outcome about the same as that of poorly differentiated breast adenocarcinoma. However, squamous cell breast cancers do typically show a reduced tendency for lymphatic spread when compared to breast adenocarcinomas. Statistically, about 10%-30% show lymphatic involvement at the time of surgery, and about 30% of patients will develop a distant metastasis.
Don’t Miss: What Is The Most Dangerous Type Of Skin Cancer
Risk Factors And Causes Of Skin Cancer
Despite the fact that high melanin content confers better photo protection, significant photo damage in the form of epidermal atypia and atrophy, dermal collagen and elastin damage and pigmentary disorders can cause skin cancer which could be fatal due to delay in detection in skin of color . Skin cancer is skin growth with varying degrees of malignancy . It is not yet very clear why skin cancer incidence has grown so dramatically over the past decades but the reason is likely to be multi factorial which includes increased UV exposure, environmental, hereditary risk factors and improved surveillance and earlier recognition . In addition, genetic polymorphisms also modulate the susceptibility to skin cancer .
Organ transplant receivers especially kidney and HIV patients have an increased frequency of skin cancers . Some treatments, including radiation therapy, phototherapy, psoralen and long-wave ultraviolet radiation can also predispose to skin malignancies . Viral infections such as the human papilloma virus can cause cancer. Patients with familial genetic patterns are vulnerable to particular types of skin cancers . Certain drugs, from common antibiotics to heart medications, can increase the skins sensitivity to sunlight, causing the skin to burn in less time and may increase the incidence of skin cancer .
Read Also: What Is Skin Cancer Caused By
How Do Tamoxifen Raloxifene Anastrozole And Exemestane Reduce The Risk Of Breast Cancer
If you are at increased risk for developing breast cancer, four medications tamoxifen , raloxifene , anastrozole , and exemestane may help reduce your risk of developing this disease. These medications act only to reduce the risk of a specific type of breast cancer called estrogen receptor-positive breast cancer. This type of breast cancer accounts for about two-thirds of all breast cancers.
Tamoxifen and raloxifene are in a class of drugs called selective estrogen receptor modulators . These drugs work by blocking the effects of estrogen in breast tissue by attaching to estrogen receptors in breast cells. Because SERMs bind to receptors, estrogen is blocked from binding. Estrogen is the fuel that makes most breast cancer cells grow. Blocking estrogen prevents estrogen from triggering the development of estrogen-receptor-positive breast cancer.
Anastrozole and exemestane are in a class of drugs called aromatase inhibitors . These drugs work by blocking the production of estrogen. Aromatase inhibitors do this by blocking the activity of an enzyme called aromatase, which is needed to make estrogen.
Read Also: What Happens In Skin Cancer
When Is A Mole A Problem
A mole is a benign growth of melanocytes, cells that gives skin its color. Although very few moles become cancer, abnormal or atypical moles can develop into melanoma over time. “Normal” moles can appear flat or raised or may begin flat and become raised over time. The surface is typically smooth. Moles that may have changed into skin cancer are often irregularly shaped, contain many colors, and are larger than the size of a pencil eraser. Most moles develop in youth or young adulthood. It’s unusual to acquire a mole in the adult years.
Skin Cancer Vs Breast Cancer
Skin cancer on breasts is possible, but that does not automatically mean the patient has breast cancer. There are many factors that separate skin cancer vs. breast cancer. Skin cancer develops in the topmost layers of the epidermis, caused by abnormal skin cell production. This is often triggered by excessive environmental stimuli that the skin tries to counteract overexposure to sunlight is the most common culprit of skin cancer. While the three types of skin cancer often start near the surface of the skin, they can penetrate deeper if left undetected, potentially spreading to surrounding tissue.
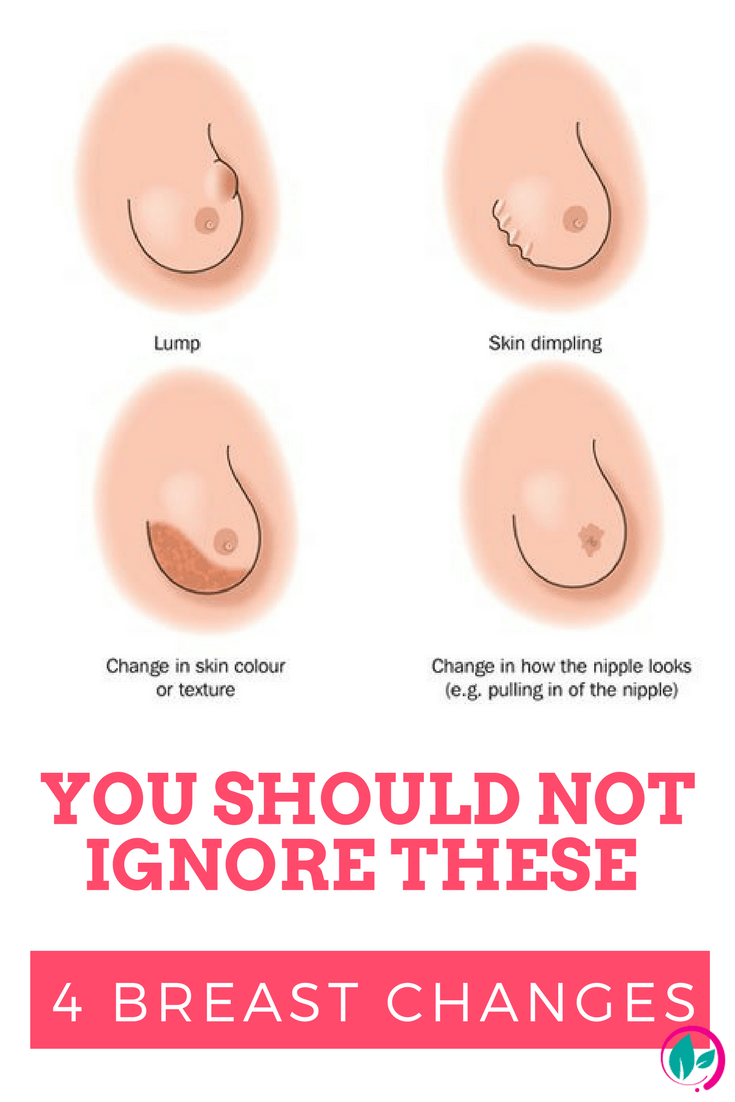
Breast cancer, on the other hand, always starts with tumors growing deep in the breast tissue. Hormonal and genetic factors contribute to breast cancer development, though the exact cause is unknown. While the most common early symptom of breast cancer is finding a hard lump in the breast, breast cancer can potentially have some effects on the surrounding skin, including:
- Dimpling of the breast skin
- Peeling or crusting around the areola or nipple
- Redness of the breast skin
While none of these symptoms constitute a breast cancer lesion on skin, its important to note that any significant changes to your skin should be treated with caution. Drastic physical changes can signal internal issues, and should be addressed by a physician as soon as possible.
Read Also: What Happens When You Have Skin Cancer
What Is Inflammatory Breast Cancer
Inflammatory breast cancer is a rare and very aggressive disease in which cancer cells block lymph vessels in the skin of the breast. This type of breast cancer is called inflammatory because the breast often looks swollen and red, or inflamed.
Inflammatory breast cancer is rare, accounting for 1 to 5 percent of all breast cancers diagnosed in the United States. Most inflammatory breast cancers are invasive ductal carcinomas, which means they developed from cells that line the milk ducts of the breast and then spread beyond the ducts.
Inflammatory breast cancer progresses rapidly, often in a matter of weeks or months. At diagnosis, inflammatory breast cancer is either stage III or IV disease, depending on whether cancer cells have spread only to nearby lymph nodes or to other tissues as well.
Additional features of inflammatory breast cancer include the following:
- Compared with other types of breast cancer, inflammatory breast cancer tends to be diagnosed at younger ages.
- Inflammatory breast cancer is more common and diagnosed at younger ages in African American women than in white women.
- Inflammatory breast tumors are frequently hormone receptor negative, which means they cannot be treated with hormone therapies, such as tamoxifen, that interfere with the growth of cancer cells fueled by estrogen.
- Inflammatory breast cancer is more common in obese women than in women of normal weight.
What Happens After The Local Breast Cancer Treatment
Following local breast cancer treatment, the treatment team will determine the likelihood that the cancer will recur outside the breast. This team usually includes a medical oncologist, a specialist trained in using medicines to treat breast cancer. The medical oncologist, who works with the surgeon, may advise the use of the drugs like tamoxifen or anastrozole or possibly chemotherapy. These treatments are used in addition to, but not in place of, local breast cancer treatment with surgery and/or radiation therapy.
After treatment for breast cancer, it is especially important for a woman to continue to do a monthly breast examination. Regular examinations will help you detect local recurrences. Early signs of recurrence can be noted in the incision area itself, the opposite breast, the axilla , or supraclavicular region .
Maintaining your follow-up schedule with your physician is also necessary so problems can be detected when treatment can be most effective. Your health care provider will also be able to answer any questions you may have about breast self-examination after the following procedures.
Also Check: Can You Have Basal Cell Carcinoma For Years
How Dna Changes Can Lead To Cancer
Genes are short segments of DNA found in chromosomes. DNA contains the instructions for building proteins. And proteins control the structure and function of all the cells that make up your body.
Think of your genes as an instruction manual for cell growth and function. Changes or mistakes in the DNA are like typographical errors. They may provide the wrong set of instructions, leading to faulty cell growth or function. In any one person, if there is an error in a gene, that same mistake will appear in all the cells that contain the same gene. This is like having an instruction manual in which all the copies have the same typographical error.
There are two types of DNA changes: those that are inherited and those that happen over time. Inherited DNA changes are passed down from parent to child. Inherited DNA changes are called germ-line alterations or mutations.
DNA changes that happen over the course of a lifetime, as a result of the natural aging process or exposure to chemicals or sunlight in the environment, are called somatic mutations.
Clinical And Cytological Presentation Of Squamous Cell Breast Carcinoma
Examined cytologically, squamous cell breast carcinoma will tend to show malignant squamous cells with keratinising cytoplasm. Nuclei are typically herpchromatic and dense, with coarse chromatin and thick nuclear membranes. Keratin debris and background necrosis are common features. Squamous cell breast tumors are usually estrogen and progesterone receptor negative. In terms of clinical presentation, squamous cell breast carcinomas usually present as a firm-to-hard painless breast lump. Clinically, it would be indistinguishable from other kinds of malignant breast lumps.
Squamous cell carcinoma can present in a very similar way to an adenocarcinoma so differential diagnosis is important. To complicate issues further for diagnosis, some tumors are mixed that is there can be squamous cells found in adenocarcinomas or from metastatic diseases elsewhere.
You May Like: Can Cancer Cause Skin Rash
How Much Do Tamoxifen And Raloxifene Lower The Risk Of Breast Cancer
Multiple studies have shown that both tamoxifen and raloxifene can reduce the risk of developing estrogen receptor-positive breast cancer in healthy postmenopausal women who are at high risk of developing the disease. Tamoxifen lowered the risk by 50 percent. Raloxifene lowered the risk by 38 percent. Overall, the combined results of these studies showed that taking tamoxifen or raloxifene daily for five years reduced the risk of developing breast cancer by at least one-third. In one trial directly comparing tamoxifen with raloxifene, raloxifene was found to be slightly less effective than tamoxifen for preventing breast cancer.
Both tamoxifen and raloxifene have been approved for use to reduce the risk of developing breast cancer in women at high risk of the disease. Tamoxifen is approved for use in both premenopausal women and postmenopausal women . Raloxifene is approved for use only in postmenopausal women.
Less common but more serious side effects of tamoxifen and raloxifene include blood clots to the lungs or legs. Other serious side effects of tamoxifen are an increased risk for cataracts and endometrial cancers. Other common, less serious shared side effects of tamoxifen and raloxifene include hot flashes, night sweats, and vaginal dryness.