Measures For Risk Management
Actions to minimize the risk are prophylactic bilateral mastectomy or breast surveillance. In case of important family history for breast cancer with CDH1 germline mutations, prophylactic bilateral mastectomy with breast reconstruction is recommended after a careful genetic counseling. In general, as well in hereditary lobular breast cancer associated with CDH1 mutations, in absence of family history for gastric cancer, prophylactic gastrectomy is not indicated therefore, yearly endoscopic surveillance should be purposed. In case of breast surveillance only, annual breast magnetic resonance imaging followed by mammography and ultrasound at six months interval, are recommended. Chemoprevention with low-dose Tamoxifen is also considered.
How Can I Reduce My Risk For Invasive Ductal Carcinoma
Like most cancers, knowing your family history can help you take preventative steps, such as early screenings and mammograms. Even though invasive ductal carcinoma cant be prevented altogether, there are steps you can take to lower your risk:
- Maintain a healthy body weight.
- Dont smoke.
- Eat a healthy, well-balanced diet.
- Undergo genetic testing for gene mutations if recommended based on family history.
When Should I See My Healthcare Provider Regarding Invasive Ductal Carcinoma
If you notice any unusual changes in your breast tissue, schedule an appointment with your healthcare provider. If youre currently undergoing treatment for invasive ductal carcinoma, call your healthcare provider if you develop any concerning symptoms, such as high fever, chills, confusion, chest pain, shortness of breath , bone pain or abdominal pain.
Don’t Miss: How Long Does It Take For Melanoma To Spread
Assessment Of Grade And Er Status
For the ICICLE study, information on cytonuclear grade of DCIS was available for 2,578 cases, mostly from the local histopathology reports. In 200 cases where the grade data were missing from the report but the tumor block was available, an H& E section was cut and the DCIS was graded by the study histopathologist according to UK and College of American Pathologists guidelines . Data on grade of DCIS were available from histopathology reports for 828 BCAC cases.
A subset of 81 ICICLE cases, graded in the pathology report and with a tumor block available, were examined to assess the reliability of the cytonuclear grade provided by the pathology reports. In the majority of cases grade was concordant with the pathology report. Nine cases were re-graded as low/intermediate grade and two cases as high grade. As the study pathologist re-graded the samples on a single H& E section, rather than all the blocks from an individual case, and in some cases on re-excision specimens with residual disease rather than the original excision specimen, the grade reported in the pathology report, if available, was used for the purposes of this study.
Request An Appointment At Moffitt Cancer Center
Please call for support from a Moffitt representative. New Patients and Healthcare Professionals can submit an online form by selecting the appropriate buttonbelow. Existing patients can call . for a current list of insurances accepted at Moffitt.
NEW PATIENTS To request a new patient appointment, please fill out the online form or call 1-888-663-3488.
REFERRING PHYSICIANS Providers and medical staff can refer patients by submitting our online referral form.
Moffit now offers Virtual Visits for patients. If you are eligible for a virtual appointment, our scheduling team will discuss this option further with you.
Moffitt Cancer Center is committed to the health and safety of our patients and their families. For more information on how were protecting our new and existing patients, visit our COVID-19 Info Hub
You May Like: What Is Clear Cell Carcinoma
A Study Looking At The Genetics Of Ductal Carcinoma In Situ
Cancer type:
Phase:
This study was to find genes that might increase the risk of ductal carcinoma in situ .
DCIS is when some cells inside the tubes in the breast have started to turn into cancer cells. DCIS might develop into an invasive ductal breast cancer if it isnt treated.
Cancer Research UK supported this study.
What Happens If My Test Is Positive For Hereditary Breast Cancer Risk
If testing confirms you are at risk, your care provider can work with you on a plan to safeguard your health, which could include:
- High-risk evaluation and monitoring
- Screening schedules, including digital mammography and clinical breast exams
- Hormonal therapy medications designed to prevent the development of breast cancer
Preventive surgery, such as mastectomy with breast reconstruction, is necessary only for patients at very high risk for aggressive breast cancer.
A comprehensive breast center offers a safe and supportive environment where you can ask questions and get the best answers for you, Ninan says. Every patients decision about how to handle their risk of developing breast cancer is managed with sensitivity and an understanding about the complexity of these decisions.
Also Check: Can You Have Cancer Without A Tumor
Diagnostic Findings Part 1
The patient appears anxious. Clinical breast examination reveals a palpable mass in theright breast of approximately 2 cm in size that is located 3 cm lateral to the nipple. Thenipple is retracted, and there is no nipple discharge. There are no palpable abnormalitiesin the left breast. The remainder of the physical examination is unremarkable.
Loh At Brca1 And Brca2 Loci And Other Chromosome Alterations
It has been demonstrated that BRCA1 promoter hypermethylation may be a second inactivation event in BRCA1 families, but this mode of inactivation is infrequent due to the dominance of genetic deletions as second hits.
Staff et al reported that the somatic loss of the other cancer susceptibility gene locus might be selected in cancer development in tumors from BRCA1/2-mutation carriers. They used microsatellite analysis and Fluorescence in situ hybridization to study somatic loss of BRCA1 in breast tumors from BRCA2-germline mutation carriers and vice versa. They found that eight out of eleven informative tumors from BRCA1-mutation carriers had BRCA2 LOH, and that five out of six informative tumors from BRCA2-mutation carriers had BRCA1 LOH. Combined LOH in BRCA1 and BRCA2 genes was seen in twelve of the 17 informative hereditary breast tumors, whereas this situation was only seen in 32 and 47% of sporadic tumors .
Table 3 Molecular characterization of familial and sporadic breast tumors
You May Like: Cell Cancer Symptoms
How Is Invasive Ductal Carcinoma Treated
There are several approaches that can be used when treating this type of breast cancer. Specific treatment depends on the size and location of your tumor, your healing capacity and your personal preferences. Invasive ductal carcinoma treatments include:
Are there side effects of invasive ductal carcinoma treatment?
Yes. As with any cancer treatment, side effects are possible. Your specific experience depends on how advanced your tumor is, where its located and what type of treatment you undergo.
People who have breast cancer surgery may experience infection, blood clots or complications from anesthesia. Those who undergo chemotherapy, radiation therapy, targeted therapy or immunotherapy may have:
- Weight changes.
- Fertility problems.
For patients receiving anti-hormone therapy, the most common side effects are hot flashes, joint pain, weight changes, mood changes, vaginal dryness or discharge and decrease of sexual desire.
You may experience other symptoms, too. Your healthcare provider can tell you what to expect during invasive ductal carcinoma treatment.
Invasive Ductal Carcinoma Survival Rate
A five-year survival rate refers to the percentage of cancer patients who are alive five years after they were diagnosed. Keep in mind that these are estimates and based on past data, and advances in treatments may have improved these numbers.
If cancer has spread only within the breast, the five-year survival rate estimate is 99 percent, according to the American Society of Clinical Oncology , and a majority of women with breast cancer receive a diagnosis at this stage.
If cancer has spread to the neighboring lymph nodes, the five-year survival rate is 86 percent, according to the ASCO, and if its spread to a distant part of the body , the rate is 28 percent.
Tremendous strides in treating breast cancer, as well as diagnosing it earlier when its in more treatable stages, are helping to improve these statistics.
Expert
You May Like: Well-differentiated Squamous Cell Carcinoma Prognosis
Cancer Risks For Womenwith Brca1/brca2 Mutations
Women who inherit a mutation in the BRCA1 or BRCA2 gene have a much higher risk of developing breast and ovarian cancer. But, important steps can be taken to help lower the risk for cancer in these women. Its important to know that not everyone who inherits a BRCA1 or BRCA2 mutation will get breast or ovarian cancer, and that not all inherited forms of breast or ovarian cancer are due to mutations in BRCA1 and BRCA2.
What Is Estrogen Receptorpositive Breast Cancer And Progesterone Receptorpositive Breast Cancer
Cells from your breast cancer can be tested for receptors on two hormones that can fuel cancer growth: estrogen and progesterone. Receptors are special proteins on cells that attach to certain substances, such as estrogen and progesterone, much like a key entering a lock. Breast cancer can contain receptors for one of these hormones, both, or neither.
- Breast cancer with receptors for estrogen is called estrogen receptor positive, or ER positive.
- Breast cancer with no receptors for estrogen is called estrogen receptor negative, or ER negative.
- Breast cancer with receptors for progesterone is called progesterone receptor positive, or PR positive.
- Breast cancer with no receptors for progesterone is called progesterone receptor negative, or PR negative.
If your cancer is ER positive, PR positive, or positive for both estrogen and progesterone receptors, your treatment may include a hormone therapy a drug or drugs that keep these hormones from plugging into their receptors. The idea is to cut off the cancers access to the fuel that would otherwise power its growth, much like putting a child safety cap on an electrical outlet.
Also Check: Web Md Skin Cancers
Family History Of Breast Cancer And Inherited Genes
Some people have a higher risk of developing breast cancer than the general population because other members of their family have had particular cancers. This is called a family history of cancer.
Having a mother, sister or daughter diagnosed with breast cancer approximately doubles the risk of breast cancer. This risk is higher when more close relatives have breast cancer, or if a relative developed breast cancer under the age of 50. But most women who have a close relative with breast cancer will never develop it.
UK guidelines help GPs to identify people who might have an increased risk of cancer due to their family history.
What Are Lobular Carcinoma In Situ And Atypical Lobular Hyperplasia
Lobular carcinoma in situ is not considered breast cancer or a precancer because it doesnt turn into invasive cancer if untreated. LCIS and atypical lobular hyperplasia , a similar noncancerous condition, are subtypes of lobular neoplasia, a disorder marked by abnormal cells in the breasts lobules . Since LCIS and ALH raise your risk for breast cancer in the future, if youve been diagnosed with either of them, talk to your doctor about how often you should be screened for breast cancer and whether you should have any additional screening tests.
Recommended Reading: Does Amelanotic Melanoma Blanch When Pressed
What Is Invasive Lobular Carcinoma
Invasive lobular carcinoma is a cancer that starts in the breasts lobules and invades surrounding tissue. ILC is the second most common form of invasive breast cancer, accounting for 10 to 15% of breast cancer cases. ILC doesnt always form a lump, but women who have it may notice a thick or full area that doesnt feel like the rest of the breast.
How Long Does It Take To Recover From Invasive Ductal Carcinoma Treatment
People who undergo surgery for invasive ductal carcinoma usually recover in about two to four weeks. Healing may take longer if lymph nodes are removed or if you choose to undergo breast reconstruction.
Recovery after chemotherapy, radiation therapy, targeted therapy or immunotherapy may take several weeks or several months, depending on the location and stage of the tumor. Your healthcare provider can tell you about how long your treatment should take.
Recommended Reading: Skin Cancer Metastasis To Lymph Nodes
What Is A Breast Papilloma And Is It Cancer
Also called intraductal papilloma, a breast papilloma is a small, wartlike growth in the breasts milk ducts. This benign condition may cause a clear or bloody discharge from the nipple, or you may feel a small lump behind or next to the nipple. Having one papilloma does not raise your breast cancer risk, though having several of these growths has been linked to higher risk.
Criteria For Genetic Screening
Clinical criteria for genetic testing were suggested as following: bilateral lobular breast cancer with or without family history of breast cancer, with age at onset < 50 years and unilateral lobular breast cancer with family history of breast cancer, with age at onset < 45 years. In this context, it has been estimated that the frequency of E-cadherin germline mutation is a rare event, affecting about 3% of the screened population. However, there are ongoing studies to assess the penetrance and the cancer risk in the hereditary lobular breast cancer syndrome.
You May Like: Well Differentiated Meaning
Having A Family History Of Breast Cancer
Its important to note that most women who get breast cancer do not have a family history of the disease. But women who have close blood relatives with breast cancer have a higher risk:
- Having a first-degree relative with breast cancer almost doubles a womans risk. Having 2 first-degree relatives increases her risk by about 3-fold.
- Women with a father or brother who has had breast cancer also have a higher risk of breast cancer.
What Can You Tell Me About Invasive Ductal Carcinoma Stages

Staging describes how advanced your cancer is, based on the location, size and how far it has spread. There are five stages of ductal carcinoma:
- Stage 0: The cancer is localized to your milk ducts. This stage is also known as non-invasive ductal carcinoma in situ.
- Stage 1: The cancer has spread outside of your milk ducts to the breast tissue, but it hasnt spread to your lymph nodes. In some cases, the cancer may have spread to your lymph nodes, but not to your surrounding breast tissue.
- Stage 2: The tumor is small and has spread to one to three of your lymph nodes. Or, the tumor is larger, but hasnt spread to any of your lymph nodes.
- Stage 3: The cancer has often spread to more than three of your lymph nodes or is causing inflammation of most of your breast skin, but hasnt spread to other areas of your body.
- Stage 4: The cancer has spread to your other organs, which may include your bones, liver, lungs, brain, chest wall or distant lymph nodes.
Read Also: Stage 3 Invasive Ductal Carcinoma Survival Rate
Alterations In Apoptosis Regulation
Dysregulation of apoptosis plays an important role in the pathogenesis and progression of breast cancer, as well as in responses of tumors to therapeutic intervention. Overexpression of BCL2 is commonly observed in estrogen receptor-positive sporadic breast carcinomas and has been associated with a good prognosis. Compared with BCL2, far less is known about the expression of other apoptotic markers in breast tumors in general, and in hereditary cases in particular.
Overexpression of BCL2 in BRCA2 tumors has been reported in several studies, confirming the good correlation between these markers and estrogen receptor status. By contrast, low levels of BCL2 but high levels of caspase 3 were observed in BRCA1 tumors. Caspase 3 is a cytosolic enzyme that is activated only in cells committed to undergoing apoptosis, and is strongly associated with morphological assessment. Thus, previous studies have shown that the apoptotic index obtained by measuring caspase activation was higher in high-grade, estrogen receptor-negative tumors, as has been observed in BRCA1-associated carcinomas. These data are in accordance with an expression study using cDNA microarrays that showed BRCA1-mutation-positive tumors to have increased expression of genes associated with inducing apoptosis , and decreased expression of genes involved in suppressing apoptosis .
Invasive Ductal Carcinoma Treatment At Moffitt Cancer Center
As a National Cancer Institute-designated Comprehensive Cancer Center, Moffitt Cancer Center is a recognized leader in breast cancer research. Because our services are research-based, our patients have access to cutting-edge techniques and promising new medications that are available only through clinical trials. We continue to make great strides in understanding the causes of breast cancer and developing effective approaches to its prevention, diagnosis and treatment.
If youd like to discuss possible causes of invasive ductal carcinoma with the breast cancer experts at Moffitt, call or complete a new patient registration form online. No referrals are required.
Recommended Reading: How Long Does It Take For Melanoma To Metastasize
Histopathology And Molecular Features Of Familial Non
Very little is known about the genetic basis of non-BRCA1/2 breast cancer. Genetic linkage analysis of families has been performed and several chromosomal regions potentially harboring breast cancer susceptibility genes have been identified, including 8p12p22, 13q21, and 2q31q33. However, these loci have either been shown not to be major predisposing loci, or their status remains to be confirmed, thereby emphasizing genetic heterogeneity and population-specific effects among non-BRCA1/2 families. Non-BRCA1/2 hereditary carcinomas represent 67% of familial breast cancers when families with only female breast cancer and four or five affected members are considered. In the Spanish population, considering families with at least three cases of female breast cancer and one of the affected women being < 50 years, 75% of cases were not attributable to BRCA1/2 mutation.
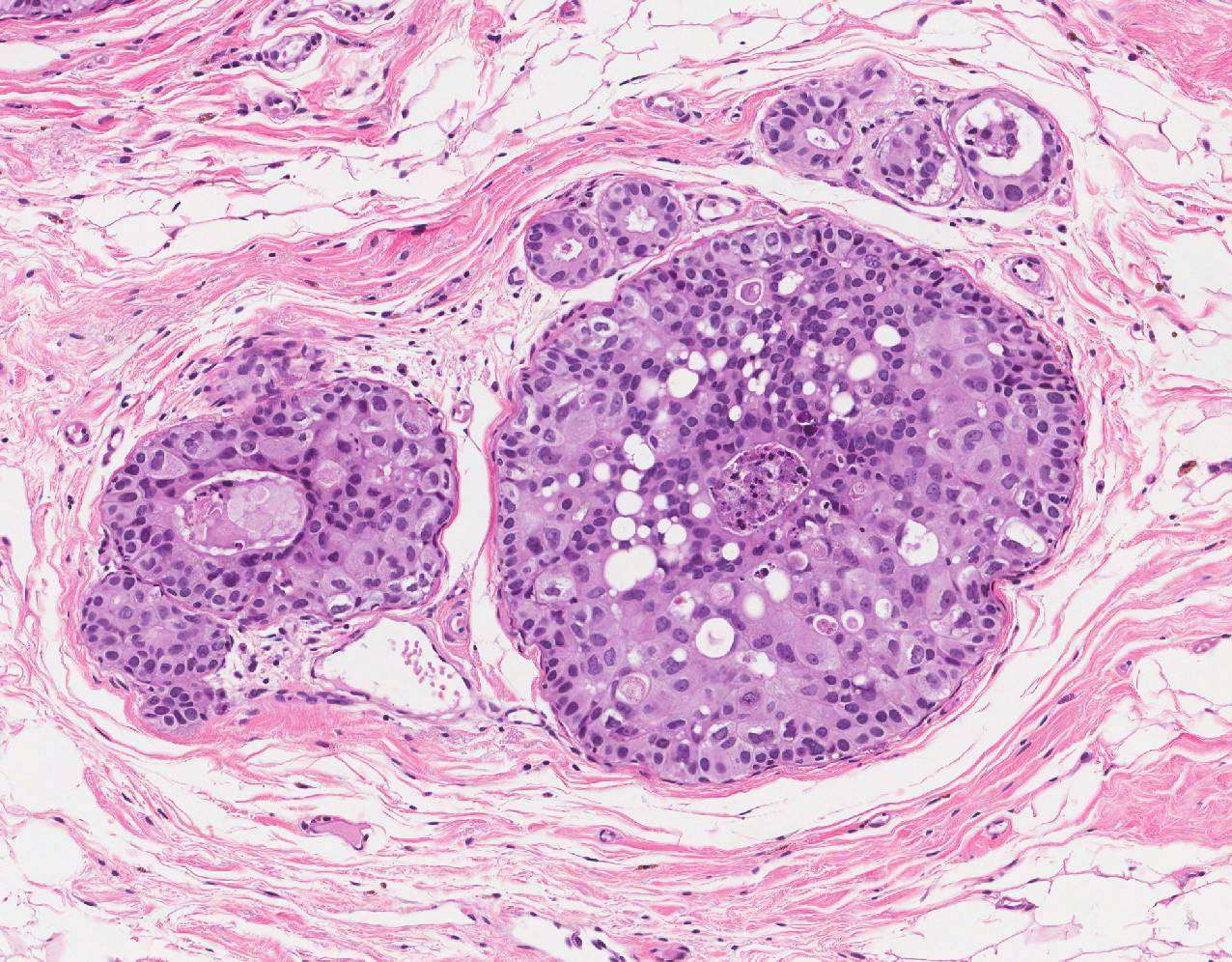
There are three studies that have defined the histological characteristics of these neoplasias., , In the three studies, invasive ductal carcinoma was the most frequent histological type: 77% of the cases according to Lakhani et al, 78% in the series of Palacios et al and 67% in the study of Eerola et al. In two of them,, an excess of lobular carcinomas was found in familial non-BRCA1/2 compared with BRCA1 , BRCA2 , and sporadic cases . The difference was only significant with respect to BRCA1 tumors.