Treatments For Stage I Melanoma
Your doctor will most likely treat stage 1 melanoma with surgery called wide excision, which cuts out the melanoma along with a margin of healthy surrounding skin. The amount of healthy skin removed is determined by the location and the thickness of the melanoma being treated.
While wide excision surgery is often the only treatment necessary, in some cases a doctor may also choose to check for cancer in nearby lymph nodes by performing a sentinel lymph node biopsy. If cancer cells are found in the lymph nodes, further treatment will become necessary, such as a lymph node dissection , chemotherapy, immunotherapy, or targeted therapies.
Treatment For Stage 0 Melanoma
The standard treatment for Stage 0 melanoma is surgery.
The purpose of the surgery is to remove any cancer remaining after the biopsy. This procedure is called a wide local excision. The surgeon removes any remaining tumor from the biopsy site, the surgical margin , and the underlying subcutaneous tissue, to make certain the whole tumor has been removed. This procedure may be done in a doctors office under local anesthetic. The width of the margin taken depends upon the thickness of the primary tumor. The surgical margin for in situ melanoma is 0.5 to 1.0 cm, based on National Comprehensive Cancer Network guidelines.
What Will You Find On A Pathology Report
The report is broken down into a few sections including:
- Some information about the patient.
- Diagnosis if it is known.
- Procedure.
- Description of what the specimen looks like to the naked eye
- Description of what was seen under the microscope
- Where the tissue was taken from.
- Diagnosis of the biopsy.
The pathologist will describe the type of melanoma and some characteristics or features of it that are important for prognosis and treatment. To help you read your report, lets go through what you may find in your report.
Type of Melanoma
Also called the histologic type or cellular type of melanoma. There are four major subtypes, with a few rare subtypes:
- Superficial Spreading Melanoma: most common of the melanomas.
- Nodular Melanoma: are always vertical growth phase present melanomas. Most commonly found on the chest, back, head or neck.
- Acral Lentiginous: most common type in dark skinned and Asian populations. More frequently occur on soles of feet, palms of hands or under nails.
- Lentigo Maligna Melanoma: tends to occur on sun-exposed areas in older people. Often found on the face or neck.
- Rare subtypes: mucosal melanoma, desmoplastic melanoma, nevoid melanoma
Breslow Depth Classification:
- Melanoma in situ or thin invasive tumors: less than 1.0mm in depth.
- Intermediate risk melanoma: 1mm 4mm in thickness.
- High risk melanoma: greater than 4.0mm in depth.
Types of Biopsies :
Also Check: Soderstrom Skin Cancer Screening
Carcinoma In Situ Vs Invasive Carcinoma
In contrast to carcinoma, or invasive cancer, carcinoma in situ has not yet invaded the basement membrane, and there is no stromal invasion. Other than thisthe fact that the cells have not yet broken through the supporting structure from which they beganthe cells appear the same as invasive cancer cells would appear under the microscope.
Available Evidence On Histologic Clearance Margins In Mis
Thirty-two articles were identified that met the inclusion criteria for this review . The majority of the articles were reviews of single-surgeon or single-institution experiences using MMS or SE for surgical treatment of MIS and/or LM. No RCTs were identified. It should be noted that a subset of studies of LM included patients with lentigo maligna melanoma we focused our review on the subcohort of patients with LM only. As previously mentioned, if the analysis did not separate in situ from invasive lesions, the study was excluded.
Recommended Reading: Does Amelanotic Melanoma Blanch When Pressed
What Are The Clinical Features Of Superficial Spreading Melanoma
Superficial spreading melanoma tends to occur at sites of intermittent, intense sun exposure, especially on the trunk in males and the legs in females .
Superficial spreading melanoma presents as a slowly growing or changing flat patch of discoloured skin. At first, it may resemble a melanocytic naevus , ephelis , or lentigo. It becomes more distinctive in time, often growing over months to years or even decades before it is recognised. Like other flat forms of melanoma, it can be recognised by the ABCDE signs: Asymmetry, Border irregularity, Colour variation, Different, and Evolving. The EGF signs indicate nodular melanoma.
Superficial spreading melanoma clinical features may include:
- Irregular asymmetrical shape
- Irregular border which may be ill-defined and smudgy in places
- Variable pigmentation: colours may include light brown, dark brown, black, blue, grey, pink, and red
- There may be skip areas that are skin coloured, or white scars due to regression
- Different the odd-mole-out or ugly duckling is different from that persons usual naevi.
- It may be larger in size than most moles: > 6 mm and often 12 centimetres in diameter at diagnosis: however aim for diagnosis when less than 6mm
- Change over days, weeks, months, or years.
A rare variant of superficial spreading melanoma is the verrucous melanoma on the limbs and back of middle-aged and elderly men.
Invasive may be indicated by the following features:
You May Like: What Is The Blue Light Treatment For Skin Cancer
Treating Stage I Melanoma
Stage I melanoma is typically treated by wide excision . The width of the margin depends on the thickness and location of the melanoma. Most often, no other treatment is needed.
Some doctors may recommend a sentinel lymph node biopsy to look for cancer in nearby lymph nodes, especially if the melanoma is stage IB or has other characteristics that make it more likely to have spread. You and your doctor should discuss this option.
If the SLNB does not find cancer cells in the lymph nodes, then no further treatment is needed, although close follow-up is still important.
If cancer cells are found on the SLNB, a lymph node dissection might be recommended. Another option might be to watch the lymph nodes closely by getting an ultrasound of the nodes every few months.
If the SLNB found cancer, adjuvant treatment with an immune checkpoint inhibitor or targeted therapy drugs might be recommended to try to lower the chance the melanoma will come back. Other drugs or perhaps vaccines might also be options as part of a clinical trial.
Also Check: Osteomyoma
What Does A Pathology Report Tell You
Skin samples taken by a biopsy or surgical excision are typically sent to a pathology laboratory for microscopic examination and diagnosis. A pathology report is issued by a pathologist ordermatopathologist.
A pathologist is a physician who diagnoses disease through laboratory tests and direct evaluation of cells, tissues, and organs. A dermatopathologist specializes in skin pathology, a subspecialty of dermatology and pathology.
The pathology report states the diagnosis and further describes any defining characteristics of the melanoma, such as the type of melanoma, depth of invasion, presence or absence of ulceration, mitotic count, presence or absence of regression, presence or absence of satellite lesions, and presence or absence of blood vessel/lymphatic vessel/nerve invasion.
Additionally, the pathology report will indicate whether the excised lesion is a primary melanoma, in which case it would be described using the terms above, or a metastatic melanoma deposit. A metastatic melanoma deposit is one in which the melanoma started somewhere else on the skin and some of the melanoma cells broke off and spread within the skin tissue to the current biopsy/specimen site.
Putting It All Together
Some pieces of the report are used to determine the stage of the cancer and other pieces play a role in deciding what treatment is needed. By understanding the basics of the report, you will be better able to discuss your treatment options with your healthcare team. Your provider will be able to explain any questions you have about your report.
Don’t Miss: Does Skin Cancer Burn And Itch
Stage I And Stage Ii Melanomas
Making a melanoma diagnosis means gathering as much information about your skin cancer as possible. One key step is determining the cancers stage, which is a measure of the amount and severity of cancer in the body. Staging helps your doctor understand how best to treat the cancer, and is used when discussing survival rates.
Following stage 0 , the degrees of melanoma range from stage I through stage IV, with higher numbers indicating further spreading of the cancer throughout the body.
There are three factors commonly used to determine melanoma staging, and theyre represented by the TNM system. The first factor is the severity of the primary tumor , which includes how thick the tumor is and whether the skin covering it has broken. The second factor is whether the cancer has spread to nearby lymph nodes . The third factor is whether the cancer has spread, or metastasized , to lymph nodes farther away in the body or other organs.
Treating Stage Iv Melanoma
Stage IV melanomas have already spread to distant lymph nodes or other areas of the body. Skin tumors or enlarged lymph nodes causing symptoms can often be removed by surgery or treated with radiation therapy.
Metastases in internal organs are sometimes removed, depending on how many there are, where they are, and how likely they are to cause symptoms. Metastases that cause symptoms but cannot be removed may be treated with radiation, immunotherapy, targeted therapy, or chemotherapy.
The treatment of widespread melanomas has changed in recent years as newer forms of immunotherapy and targeted drugs have been shown to be more effective than chemotherapy.
Immunotherapy drugs called checkpoint inhibitors such as pembrolizumab or nivolumab are typically the first drugs tried, especially in people whose cancer cells do not have BRAF gene changes. These drugs can shrink tumors for long periods of time in some people. Ipilimumab , a different type of checkpoint inhibitor, is not typically used by itself as the first treatment, although it might be combined with nivolumab or pembrolizumab. This slightly increase the chances that the tumor will shrink, although itâs also more likely to result in serious side effects, which needs to be considered carefully. People who get any of these drugs need to be watched closely for serious side effects..
Itâs important to carefully consider the possible benefits and side effects of any recommended treatment before starting it.
Don’t Miss: What Is The Most Aggressive Skin Cancer
What To Ask Your Doctor About Stage 0 Melanoma
When your doctor tells you that you have Stage 0 melanoma, it can be frightening. But it is important to use the time with your doctor to learn as much about your cancer as you can. S/he will provide you important information about your diagnosis and what happens next.
The following questions are those you may want to ask your doctor. Remember, it is ALWAYS okay to ask your doctor to repeat or clarify something s/he said so that you can better understand it. You may find it helpful to print out these questions and bring them with you to your next appointment.
How Is Melanoma Diagnosed
If you have a mole or other spot that looks suspicious, your doctor may remove it and look at it under the microscope to see if it contains cancer cells. This is called a biopsy.
After your doctor receives the skin biopsy results showing evidence of melanoma cells, the next step is to determine if the melanoma has spread. This is called staging. Once diagnosed, melanoma will be categorized based on several factors, such as how deeply it has spread and its appearance under the microscope. Tumor thickness is the most important characteristic in predicting outcomes.
Melanomas are grouped into the following stages:
- Stage 0 : The melanoma is only in the top layer of skin .
- Stage I: Low-risk primary melanoma with no evidence of spread. This stage is generally curable with surgery.
- Stage II: Features are present that indicate higher risk of recurrence, but there is no evidence of spread.
- Stage III: The melanoma has spread to nearby lymph nodes or nearby skin.
- Stage IV: The melanoma has spread to more distant lymph nodes or skin or has spread to internal organs.
Recommended Reading: What Is The Most Aggressive Skin Cancer
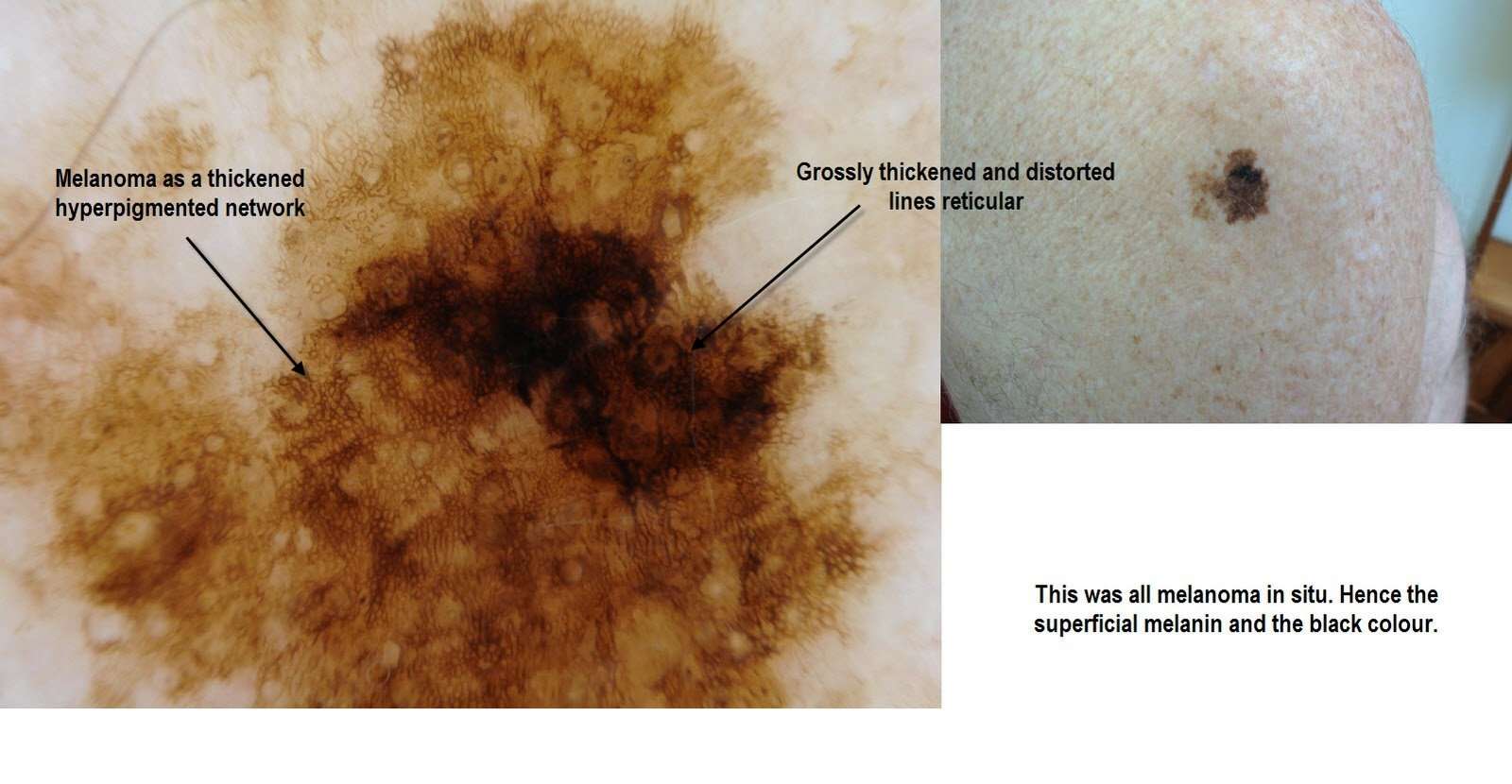
What Is Stage 0 Melanoma
In Stage 0 melanoma, the malignant tumor is still confined to the upper layer of the skinthe epidermiswhich means the cancer cells are only in the outer layer of the skin and have not grown into the second layer of skin, called the dermis. Stage 0 melanoma is not considered invasive melanoma the other stages are invasive. In Stage 0 melanoma, there is no evidence the cancer has spread to the lymph nodes or to distant sites . Stage 0 is local melanoma, meaning it has not spread beyond the primary tumor. Another term for Stage 0 melanoma is in situ, which means in place in Latin.
Superficial Spreading Malignant Melanoma
This is the most common type of invasive malignant melanoma comprising approximately 70% of all tumors. It starts in the basal layer and spreads horizontally for months to years before it invades into the dermis. It appears as a flat or barely raised pigmented lesion with irregular borders, like ink leaching out into paper and variable color. It is found most commonly on the trunks of men, the legs of women, and the upper backs of both sexes. It is diagnosed most frequently between the ages of 30 and 50 years. 50% occur in pre-existing moles and appear as a darkening or change in color of part of a mole. The other 50% arise as new moles on normal-appearing skin.
You May Like: How To Identify Basal Cell Carcinoma
How Is Melanoma In Situ Treated
Melanoma in situ is treated by excision biopsy. A special tissue-sparing technique may be used for a large melanoma in situ, such as Mohs micrographic surgery or staged mapped excisions .
When surgical margins are narrow, a second surgical procedure is undertaken, including a 510mm clinical margin of normal skin, to ensure complete removal of the melanoma. This is known as wide local excision.
Non-surgical options may be considered in selected cases of melanoma in situ where surgery is contraindicated, including imiquimod cream , intralesional interferon-alpha, radiation therapy, and laser therapy. Recurrence rates are high with these second-line treatments.
Clinical Staging And Pathologic Staging
To add to the complexity of staging, the cancer also may have a clinical stage and a pathologic stage.
Clinical staging takes place before surgery, based on blood tests, physical exams or imaging tests such as X-rays, a computed tomography scan, magnetic resonance imaging or positron emission tomography scans.
What doctors discover during surgery may provide more detailed information about the cancers size and spread. Often, some tissue from the surgery will be examined afterward to provide more clues. This process is known as pathologic staging, or surgical staging.
If surgery isnt possible, doctors will use the clinical stage when determining a treatment plan.
You May Like: Can Squamous Cell Carcinoma Metastasis
What Is The Outcome For Melanoma In Situ
Patients with melanoma in situ have the same life expectancy as the general population. Further problems are rare from melanoma in situ because the malignant cells within the epidermis have no metastatic potential. However, a small focus of invasive disease may have beeen missed due to the impracticability of evaluating every part of a large skin lesion.
Melanoma in situ occasionally recurs at the same site, requiring further surgery.
Recurrence In Other Parts Of The Body
Melanoma can also come back in distant parts of the body. Almost any organ can be affected. Most often, the melanoma will come back in the lungs, bones, liver, or brain. Treatment for these recurrences is generally the same as for stage IV melanoma . Melanomas that recur on an arm or leg may be treated with isolated limb perfusion/infusion chemotherapy.
Melanoma that comes back in the brain can be hard to treat. Single tumors can sometimes be removed by surgery. Radiation therapy to the brain may help as well. Systemic treatments might also be tried.
As with other stages of melanoma, people with recurrent melanoma may want to think about taking part in a clinical trial.
The treatment information given here is not official policy of the American Cancer Society and is not intended as medical advice to replace the expertise and judgment of your cancer care team. It is intended to help you and your family make informed decisions, together with your doctor. Your doctor may have reasons for suggesting a treatment plan different from these general treatment options. Dont hesitate to ask him or her questions about your treatment options.
Also Check: Stage 3 Basal Cell Carcinoma Survival Rate
Treatments For Stage Ii Melanoma
As with stage I, stage II melanoma is typically treated with wide excision surgery, which cuts out the melanoma along with a margin of healthy surrounding skin. In the case of stage II melanoma, many doctors will recommend looking for cancer in nearby lymph nodes by performing a sentinel lymph node biopsy, which may necessitate further treatment if cancer cells are found.
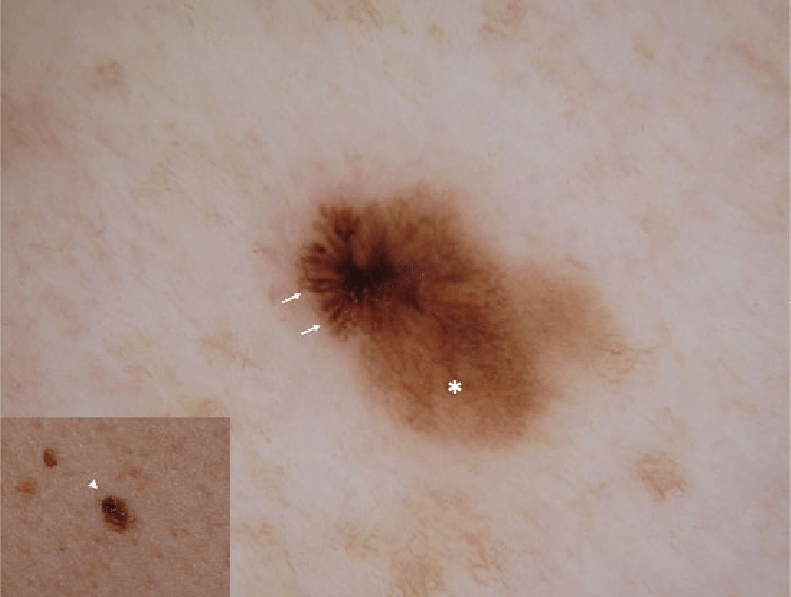
What Are The Clinical Features Of Melanoma In Situ

Typically, melanoma in situ is an irregular pigmentedpatch of skin. It often has the ABCDE criteria:
ABCDE
The body site and other clinical features of melanoma in situ depend on the subtype of melanoma . In general terms, melanoma in situ is macular . However, in about 8% of cases, melanoma in situ is thickened and can be scaly due to reactive thickening of the epidermis .
Read Also: Does Amelanotic Melanoma Blanch When Pressed
Mitotic Rate And Your Melanoma Pathology Report
Casey Gallagher, MD, is board-certified in dermatology. He is a clinical professor at the University of Colorado in Denver, and co-founder and practicing dermatologist at the Boulder Valley Center for Dermatology in Colorado.
One way to better understand your melanoma diagnosis and the resulting treatment strategy is to read your melanoma pathology report, which is sent to your healthcare provider and contains critical information such as the exact stage of your disease.