How Is Melanoma In Situ Diagnosed
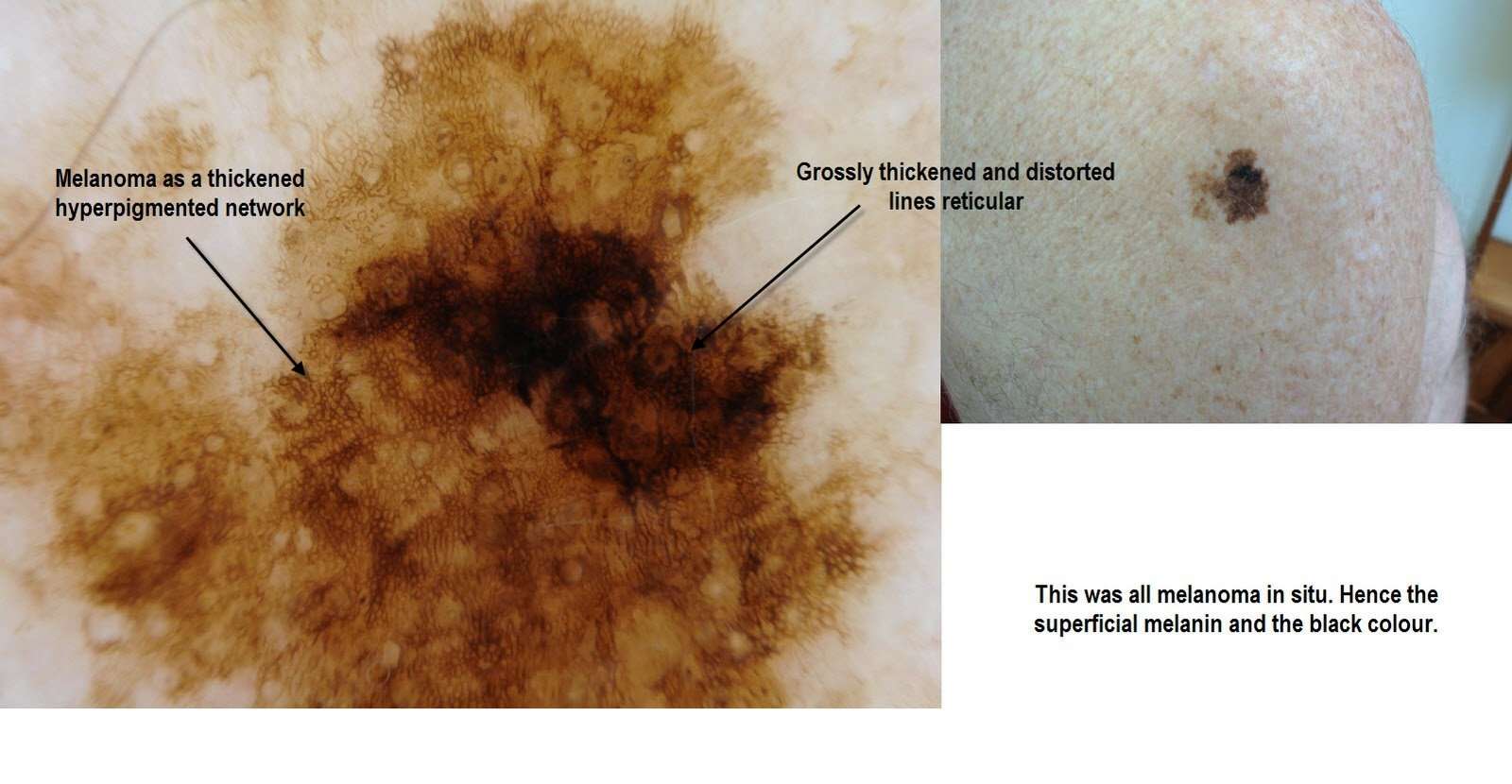
Melanoma in situ may be suspected clinically or by dermoscopy.
Diagnosis is confirmed by histological examination of the tumour and finding malignant melanocytes confined to the epidermis and epidermaladnexal structures. Breslow thickness is not reported for melanoma in situ.
- Melanoma in situ is often reported as a Clark level 1 melanoma.
- Melanoma in situ is considered Stage 0 in the American Joint Committee on Cancer staging guidelines.
Multiple sections through the specimen should be examined to ensure there are no areas of invasive disease. Immunohistochemical stains, such as micropthalmia-associated transcription factor and Sry-related HMG-BOX gene 10 , may aid diagnosis .
- In sun-damaged skin, it can be difficult to differentiate benign forms of atypical melanocytic hyperplasia and lichenoidinflammation from melanoma in situ.
- The morphology may differ between subtypes of melanoma.
- An initial diagnosis of melanoma in situ may be upstaged to invasive melanoma upon evaluating the deeper sections of a complete excision specimen.
Recurrence In Other Parts Of The Body
Melanoma can also come back in distant parts of the body. Almost any organ can be affected. Most often, the melanoma will come back in the lungs, bones, liver, or brain. Treatment for these recurrences is generally the same as for stage IV melanoma . Melanomas that recur on an arm or leg may be treated with isolated limb perfusion/infusion chemotherapy.
Melanoma that comes back in the brain can be hard to treat. Single tumors can sometimes be removed by surgery. Radiation therapy to the brain may help as well. Systemic treatments might also be tried.
As with other stages of melanoma, people with recurrent melanoma may want to think about taking part in a clinical trial.
The treatment information given here is not official policy of the American Cancer Society and is not intended as medical advice to replace the expertise and judgment of your cancer care team. It is intended to help you and your family make informed decisions, together with your doctor. Your doctor may have reasons for suggesting a treatment plan different from these general treatment options. Don’t hesitate to ask him or her questions about your treatment options.
What They Look Like
Melanomas in situ tend to be flat and asymmetric with irregular borders. They can be black, brown, tan, gray or even pink if the person has very fair skin. Areas that receive the greatest sun exposure, such as the scalp, face and neck, are more likely to develop melanoma in situ than the arms or legs. However, non-sun exposed areas, such as the buttocks, are also at risk. We dont always understand the causes of these melanomas, though heredity can play a role. To detect melanoma in situ as early as possible, it helps to monitor your own skin. Head-to-toe self-examinations are a good place to start, including the areas where the sun doesnt shine. When evaluating your skin, focus on the ABCDEs of melanoma detection. A stands for asymmetry B for irregular borders C for more than one color D for diameter greater than 6mm , or the size of a pencil eraser and E for evolving, meaning any lesion that is new or changing. View helpful photos showing the ABCDEs of melanoma.
Also Check: Are There Stages Of Basal Cell Carcinoma
Melanoma At Its Most Curable
Our authors recent research shows that melanoma in situ, the earliest form of the disease, is on the rise, especially among young men. Heres why this is bad news and good news, and what everyone needs to know to stay ahead of it.
H. WILLIAM HIGGINS II, MD, MBE, and DAVID LEFFELL, MD
Growing up in Texas, Jim was no stranger to sun exposure. A year-round athlete, he also spent many summers landscaping, and he was proud of his golden bronze tan. To achieve this look, he purposely burned during his first intense sun exposure in spring, thinking that would be a good start on maintaining a tan through the summer. He even frequented tanning salons during the winter to keep it going.
When Jims mother noticed a spot on his cheek shed never seen before, she pointed it out to him. It was dark brown, about the size of a pencil eraser, and it had an irregular shape. At first glance, it looked like a new freckle or mole. When it continued to grow, Jim became worried and visited a dermatologist. Just 29 years old, he was shocked when tests showed he had melanoma, a cancer that arises in the skins pigment-producing cells.
He was lucky, though. It was melanoma in situ: The tumor had not invaded beyond the epidermis, the outermost layer of the skin. The earliest form of melanoma , it is the easiest to treat and almost always curable. If Jim had waited any longer before seeing the doctor, it could have been much worse.
Checking Your Skin For A Melanoma With Central Regression

Its important to note that a benign mole that has a hair follicle in it can pass as a centrally regressed melanoma to the laypersons naked eye.
A benign mole can also have central regression.
Examine your skin every month for suspicious moles or changes in moles such as in their borders and symmetry.
When in doubt, see a dermatologist!
If any mole or spot is ever removed, request a biopsy, even if the removal is for cosmetic purposes.
Specializing in the diagnosis and treatment of all skin conditions including melanoma, Dr. Madan has a special interest in skin cancer treatment, including Mohs micrographic surgery for basal cell carcinoma.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. Shes also a former ACE-certified personal trainer.
Recommended Reading: What Does Squamous Skin Cancer Look Like
What Is Melanomain Situ
Melanoma in situ is an early form of primary melanoma in which the malignant cells are confined to the tissue of origin, the epidermis. It is also known as in-situ melanoma and level 1 melanoma.
As melanoma in situ has no associated mortality, early detection of melanoma in an in-situ phase increases survival from melanoma and leads to less morbidity and decreased costs compared to that associated with more advanced melanoma .
Management of melanoma is evolving. For up to date recommendations, refer to Australian Cancer Council Clinical practice guidelines for the diagnosis and management of melanoma.
Melanoma in situ
See more images of melanoma in situ.
Supplement Moh’s Surgery And Staged Serial Excision
A large prospective study assessed complete clearance of 1120 melanomas in situ excised by Mohs micrographic surgery with frozen-section examination of the margin. Six millimetre margins were adequate for complete clearance in 86% of all tumours 9 mm margins were adequate for complete clearance in 98.9% of all tumours. A 1.2 cm margin yielded 99.4% clearance, 1.5 cm margin yielded 99.6% clearance, and 3 cm margin yielded 100% clearance. The authors state that the frequently recommended 5 mm margin for melanoma is inadequate. Standard surgical excision of melanoma in situ should include 9 mm of normal-appearing skin, similar to that recommended for early invasive melanoma. This study includes a mixture of cases of melanoma in situ, both LM and non-lentigo maligna type, and it is possible that LM requires a wider margin than other melanomas in situ.
A retrospective review of 192 cases of melanoma in situ found that LM required wider margins for complete excision than did non-lentigo maligna melanoma in situ.
In a study of 51 cases of facial LM and thin LMM, with LMM present in nine lesions , peripheral margin control was performed with repeated margin excision until histological clearance of the lesion. Margins required for clearance of LM and LMM averaged 1.0 and 1.3 cm, respectively. No recurrences were identified with long-term follow-up. Immediate reconstruction was performed in all cases.
You May Like: Is Skin Cancer Usually Raised
What Is The Cause Of Superficial Spreading Melanoma
Superficial spreading melanoma is due to the development of malignant pigment cells along the basal layer of the epidermis. The majority arise in previously normal-appearing skin. About 25% develop within an existing melanocytic naevus, which can be a normal common naevus, an atypical or dysplastic naevus, or a congenital naevus.
What triggers the melanocytes to become malignant is not fully known. Specific genemutations such as BRAFV600E have been detected in many superficial spreading melanomas and these mutations may change as the disease advances.
Damage by ultraviolet radiation results in a degree of immune tolerance, allowing abnormal cells to grow unchecked. This can occur from exposure to natural sunlight, particularly if sunburn has occurred, and artificial sources of ultraviolet radiation from sun beds / solaria.
What To Ask Your Doctor About Stage 0 Melanoma
When your doctor tells you that you have Stage 0 melanoma, it can be frightening. But it is important to use the time with your doctor to learn as much about your cancer as you can. S/he will provide you important information about your diagnosis and what happens next.
The following questions are those you may want to ask your doctor. Remember, it is ALWAYS okay to ask your doctor to repeat or clarify something s/he said so that you can better understand it. You may find it helpful to print out these questions and bring them with you to your next appointment.
Don’t Miss: How To Identify Skin Cancer On Leg
What Is A Melanoma In Situ
Melanoma in situ is an early stage type of melanoma. In situ means that the cancer cells may not have had the opportunity to spread to anywhere else in the body. The cancer cells are in the top layer of the skin and they are all contained in the area in which they began to develop, they have not become invasive to the lower layers of skin . If not treated, melanoma in situ can develop into an invasive cancer. It may be referred to as a precancerous lesion.
What Is Stage 0 Melanoma
In Stage 0 melanoma, the malignant tumor is still confined to the upper layer of the skinthe epidermiswhich means the cancer cells are only in the outer layer of the skin and have not grown into the second layer of skin, called the dermis. Stage 0 melanoma is not considered invasive melanoma the other stages are invasive. In Stage 0 melanoma, there is no evidence the cancer has spread to the lymph nodes or to distant sites . Stage 0 is local melanoma, meaning it has not spread beyond the primary tumor. Another term for Stage 0 melanoma is in situ, which means in place in Latin.
You May Like: What Happens When Melanoma Spreads
What Will You Find On A Pathology Report
The report is broken down into a few sections including:
- Some information about the patient.
- Diagnosis if it is known.
- Procedure.
- Description of what the specimen looks like to the naked eye
- Description of what was seen under the microscope
- Where the tissue was taken from.
- Diagnosis of the biopsy.
The pathologist will describe the type of melanoma and some characteristics or features of it that are important for prognosis and treatment. To help you read your report, let’s go through what you may find in your report.
Type of Melanoma
Also called the histologic type or cellular type of melanoma. There are four major subtypes, with a few rare subtypes:
- Superficial Spreading Melanoma: most common of the melanomas.
- Nodular Melanoma: are always vertical growth phase present melanomas. Most commonly found on the chest, back, head or neck.
- Acral Lentiginous: most common type in dark skinned and Asian populations. More frequently occur on soles of feet, palms of hands or under nails.
- Lentigo Maligna Melanoma: tends to occur on sun-exposed areas in older people. Often found on the face or neck.
- Rare subtypes: mucosal melanoma, desmoplastic melanoma, nevoid melanoma
Breslow Depth Classification:
- Melanoma in situ or thin invasive tumors: less than 1.0mm in depth.
- Intermediate risk melanoma: 1mm – 4mm in thickness.
- High risk melanoma: greater than 4.0mm in depth.
Types of Biopsies :
What Are The Clinical Features Of Melanoma In Situ
Typically, melanoma in situ is an irregular pigmentedpatch of skin. It often has the ABCDE criteria:
ABCDE
The body site and other clinical features of melanoma in situ depend on the subtype of melanoma . In general terms, melanoma in situ is macular . However, in about 8% of cases, melanoma in situ is thickened and can be scaly due to reactive thickening of the epidermis .
Also Check: How To Get Skin Cancer
New Melanomas Likely To Recur At Same Rate
byCharles Bankhead, Senior Editor, MedPage Today August 9, 2014
CHICAGO — A diagnosis of in situ or invasive melanoma conferred a similar long-term risk of invasive melanoma recurrence, a 40-year retrospective review showed.
For the first 2 years after initial diagnosis, invasive melanoma had a greater risk of invasive recurrence, as compared with an initial diagnosis of in situ disease. Thereafter, the risk of invasive recurrence remains the same, regardless of the initial diagnosis, Hyemin Pomerantz, MD, of Brown University in Providence, R.I., reported here at the American Academy of Dermatology summer meeting.
Action Points
- Note that this study was published as an abstract and presented at a conference. These data and conclusions should be considered to be preliminary until published in a peer-reviewed journal.
“The findings suggest that follow-up after diagnosis of in situ or invasive melanoma should be the same,” Pomerantz told MedPage Today. “Because the incidence of melanoma in situ is increasing, surveillance for recurrence in this patient population could help improve outcomes for melanoma.”
To compare recurrence risk associated with the initial diagnosis, investigators reviewed data from the Surveillance, Epidemiology, and End Results program for 1973 to 2011. They identified all patients with a first diagnosis of melanoma and no history of other types of cancer and determined the classification of the initial diagnosis .
Disclosures
Primary Source
Mitotic Rate Of Your Melanoma
The staging system has been recently updated. It no longer includes the mitotic rate to work out your stage. But your doctor may still use it to work out how likely your cancer. is to spread.
Mitotic rate means the number of cells that are dividing in a certain amount of melanoma tissue. Higher mitotic rate may mean that the melanoma is at greater risk the spreading because more cells are dividing more.
Read Also: How Can You Tell If You Have Skin Cancer
Carcinoma In Situ Vs Invasive Carcinoma
In contrast to carcinoma, or invasive cancer, carcinoma in situ has not yet invaded the basement membrane, and there is no stromal invasion. Other than thisthe fact that the cells have not yet broken through the supporting structure from which they beganthe cells appear the same as invasive cancer cells would appear under the microscope.
What Are The Clinical Features Of Superficial Spreading Melanoma
Superficial spreading melanoma tends to occur at sites of intermittent, intense sun exposure, especially on the trunk in males and the legs in females .
Superficial spreading melanoma presents as a slowly growing or changing flat patch of discoloured skin. At first, it may resemble a melanocytic naevus , ephelis , or lentigo. It becomes more distinctive in time, often growing over months to years or even decades before it is recognised. Like other flat forms of melanoma, it can be recognised by the ABCDE signs: Asymmetry, Border irregularity, Colour variation, Different, and Evolving. The EGF signs indicate nodular melanoma.
Superficial spreading melanoma clinical features may include:
- Irregular asymmetrical shape
- Irregular border which may be ill-defined and smudgy in places
- Variable pigmentation: colours may include light brown, dark brown, black, blue, grey, pink, and red
- There may be skip areas that are skin coloured, or white scars due to regression
- Different – the odd-mole-out or ‘ugly duckling’ is different from that person’s usual naevi.
- It may be larger in size than most moles: > 6 mm and often 12 centimetres in diameter at diagnosis: however aim for diagnosis when less than 6mm
- Change over days, weeks, months, or years.
A rare variant of superficial spreading melanoma is the verrucous melanoma on the limbs and back of middle-aged and elderly men.
Invasive may be indicated by the following features:
You May Like: What Is The Blue Light Treatment For Skin Cancer
Meaning Of Carcinoma In Situ
In many ways, the term “carcinoma” is simply equated with cancer. Roughly 85 percent of cancers are carcinomas. Carcinomas are composed of epithelial cells the type of cells that line the skin, breast ducts, and other surfaces of organs in the body.
The subtypes of carcinomas include adenocarcinoma, squamous cell carcinoma, transitional cell carcinoma , and basal cell carcinoma.
Carcinoma in situ can be further defined by the tissue type in which cancer is beginning. For example, squamous cell carcinoma in situ of the cervix would represent a cancer that had started in squamous cells which line the cervix and has not yet become invasive.
Tumors such as sarcomas arise in tissues which do not have a basement membrane so that for these types of cancer there is not a stage of carcinoma in situ. In other words, tumors such as bone cancer do not have a pre-invasive stage and the cells would either be considered normal or cancer. Likewise, blood-related cancers, such as leukemias and lymphomas, do not have a preinvasive but cancerous stage for which people can be screened. For cancers that don’t have a CIS stage, screening tests are not as effective in early detection, because once the abnormal cells are detected, it would already be considered invasive with the potential to spread .
Treating Stage Iii Melanoma
These cancers have already reached the lymph nodes when the melanoma is first diagnosed. Surgical treatment for stage III melanoma usually requires wide excision of the primary tumor as in earlier stages, along with lymph node dissection.
After surgery, adjuvant treatment with an immune checkpoint inhibitor or with targeted therapy drugs may help lower the risk of the melanoma coming back. Other drugs or perhaps vaccines may also be recommended as part of a clinical trial to try to reduce the chance the melanoma will come back. Another option is to give radiation therapy to the areas where the lymph nodes were removed, especially if many of the nodes contain cancer.
If melanoma tumors are found in nearby lymph vessels in or just under the skin , they should all be removed, if possible. Other options include injections of the T-VEC vaccine , Bacille Calmette-Guerin vaccine, or interleukin-2 directly into the melanoma radiation therapy or applying imiquimod cream. For melanomas on an arm or leg, another option might be isolated limb perfusion or isolated limb infusion . Other possible treatments might include targeted therapy , immunotherapy, or chemotherapy.
Some people with stage III melanoma might not be cured with current treatments, so they may want to think about taking part in a clinical trial of newer treatments.
Read Also: How Often Does Basal Cell Carcinoma Spread