Metastatic Brain Cancer Treatment
It is important to know that metastatic brain tumors are often treatable, and can be well-controlled. Generally, the faster you start treatment, the better the chances of killing or controlling the disease.
The treatment options for brain metastases may include:
- Surgery
- Immunotherapy
- Clinical trials
In many cases, surgery or radiation therapy can improve or entirely get rid of symptoms. Read more about brain tumor treatment.
Survival And Clinical Outcome
Fifty-nine patients had died of melanoma progression at the time of the analysis, among which 32 died with progressing brain metastases. The median overall survival duration from the time of initial brain metastasis was 12.8;months ;, and the median overall survival duration from the time of initial melanoma diagnosis was 60.5;months for all 79 patients. The median overall survival durations from the time of craniotomy and stereotactic radiosurgery were 17.3;months and 15.4;months , respectively. The median survival durations of patients who received anti-CTLA-4 antibody, anti-PD-1 antibody and BRAF inhibitor after the diagnosis of brain metastasis were 19.2;months , 37.9;months and 12.7;months , respectively. Tables; and describe the outcomes of the entire cohort as well as specific subsets of patients. Figures and illustrate the Kaplan-Meier curves of overall survival for all patients and for those who were treated with or without anti-PD-1 therapy, respectively.
Fig. 1
Immunotherapy Combination Attacks Brain Tumors In Stage 4 Melanoma Patients
In a breakthrough clinical trial, T cells bypass the blood-brain barrierto attack metastatic tumors
Colleen Wittoesch learned in March 2016 that she had late-stage melanoma in the most difficult way.
“I couldn’t get my thoughts together, I kept forgetting things,” she recalls. “One night I was talking to my daughter and she said ‘you don’t sound right, we need to take you to the ER.'”
An MRI scan showed 12 tumors in her brain. A surgeon removed the two largest, which were applying pressure on her brain and affecting her thinking.
Wittoesch sought treatment at MD Anderson, where she had volunteered for 12 years, seven of those in the Melanoma clinic.
For stage IV melanoma that has spread to the brain, surgery and radiation can remove small tumors and provide relief from symptoms, but they don’t stop disease progression. Median survival for these patients is four-to-five months.
Melanoma brain metastases are known to be resistant to multiple types of chemotherapies. In addition, due to the poor prognosis associated with melanoma brain metastases, patients often are excluded by drug companies from clinical trials.
In 2016, this had started to change, and Wittoesch’s oncologist, Rodabe Amaria, M.D., an assistant professor of Melanoma Medical Oncology, enrolled her in a clinical trial of two immunotherapy drugs designed to free the immune system to attack cancer.
Not long after the three-month initial regimen of the drugs ipilimumab and nivolumab, Amaria had good news.
You May Like: What Is The Main Cause Of Skin Cancer
Metastatic Melanoma Life Expectancy
The 5-year survival rate for a metastatic melanoma is about 15% to 20% 7). The 10-year survival is about 10% to 15% 8). The outlook is better if the spread is only to distant parts of the skin or distant lymph nodes rather than to other organs, and if the blood level of lactate dehydrogenase is normal.
- The survival differences among M categories will be useful for clinical trial stratification; however, the overall prognosis of all patients with stage IV melanoma remains poor, even among patients with M1a. For this reason, the Melanoma Staging Committee recommended no stage groupings for stage IV.
Table 2. American Joint Committee on Cancer TNM system for Stage 4 Melanoma
| M |
|---|
- A sore that doesnt heal
- Spread of pigment from the border of a spot into surrounding skin
- Redness or a new swelling beyond the border of the mole
- Change in sensation, such as itchiness, tenderness, or pain
- Change in the surface of a mole scaliness, oozing, bleeding, or the appearance of a lump or bump
Be sure to show your doctor any areas that concern you and ask your doctor to look at areas that may be hard for you to see. Its sometimes hard to tell the difference between melanoma and an ordinary mole, even for doctors, so its important to show your doctor any mole that you are unsure of.
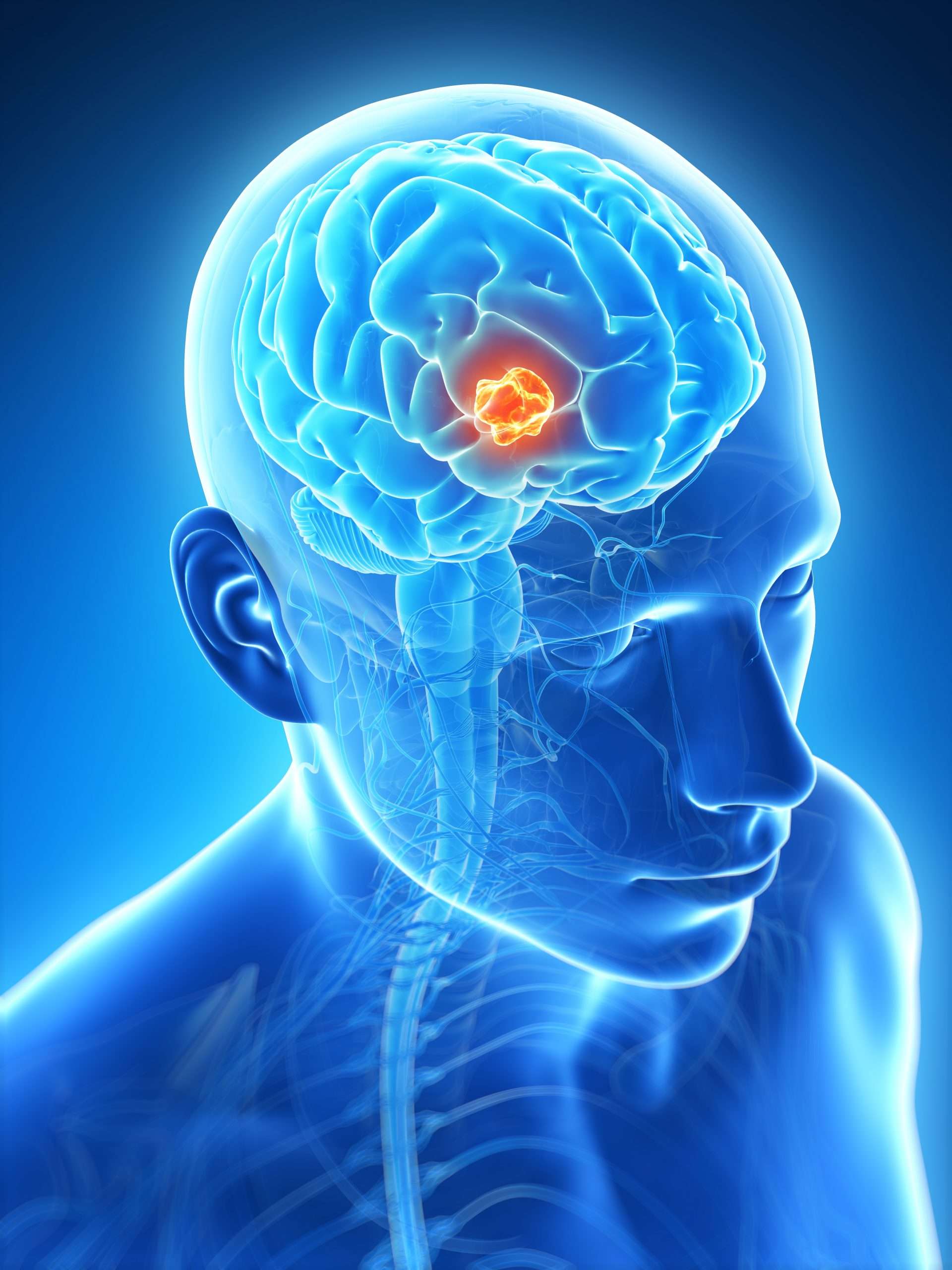
Metastatic melanoma in the brain
Figure 2. Metastatic melanoma in the brain
How Are Metastatic Brain Tumors Diagnosed
Metastatic brain and spine tumors are not usually diagnosed until symptoms appear. Here are some ways doctors may diagnose a metastatic brain tumor:
- Physical exam: After gathering information about your symptoms and personal and family health history, the doctor proceeds with a physical exam and vision and reflex tests.
- Magnetic resonance imaging;
- Diffusion tensor imaging is a type of MRI that visualizes how water molecules pass through parts of the brain. It reveals microscopic differences of tissue structure, including very early infiltration of cancer cells.
Also Check: How Common Is Renal Cell Carcinoma
Predictive Factors For Overall Survival
We analyzed the potential association between several factors and survival using univariate Cox regression of overall survival . Intriguingly, of factors in the primary tumor, increased levels of tumor-infiltrating lymphocytes showed a trend toward improved survival in patients with brain metastasis. Several clinical factors were found to be significantly associated with overall survival in patients with brain metastasis by univariate analysis . Factors associated with shorter overall survival included male sex, cerebellar involvement, higher number of metastatic brain tumors, concurrent presence of adrenal metastasis, or treatment with whole-brain radiation therapy. Factors associated with longer overall survival were treatment with craniotomy, stereotactic radiosurgery, or anti-PD-1 antibody therapy after initial diagnosis of brain metastasis.
Table 4 Univariate Cox regression analysis of association of various clinical factors with overall survival in melanoma patients with brain metastasis
Multivariate analysis of all eight factors revealed cerebellar involvement, craniotomy, and adrenal involvement as independently predictive of survival . There was trend toward significance for treatment with anti-PD-1 antibody .
Table 5 Multivariate Cox regression analysis of association of various clinical factors with overall survival in melanoma patients with brain metastasis
Treatment Of Metastatic Melanoma
Metastatic melanomas can be difficult to treat. The five-year survival rate for people diagnosed with melanoma that has spread to nearby lymph nodes is 66 percent, according to the American Cancer Society. When cancer has spread to distant parts of the body, there may also be other metastases too small to detect by scans. For people diagnosed with stage 4 melanoma, or melanoma that has spread to distant parts of the body, the five-year survival rate is 27 percent.
For stage 3 and 4 melanomas, the following treatments may be used:
Multiple therapies can be used at any given time, and your care plan is a dynamic process. You and your care team should discuss all the options and decide on a treatment plan. Each treatment has different side effects, and its important to feel fully informed of all the associated risks. Other medications and options may help manage the symptoms of your cancer treatment, so you can live the highest quality of life possible throughout the course of your treatment and disease.
Expert
Read Also: Can Melanoma Be Treated Successfully
Treating Stage Iii Melanoma
These cancers have already reached the lymph nodes when the melanoma is first diagnosed. Surgical treatment for stage III melanoma usually requires wide excision of the primary tumor as in earlier stages, along with lymph node dissection.
After surgery, adjuvant treatment with an immune checkpoint inhibitor or with targeted therapy drugs may help lower the risk of the melanoma coming back. Other drugs or perhaps vaccines may also be recommended as part of a clinical trial to try to reduce the chance the melanoma will come back. Another option is to give radiation therapy to the areas where the lymph nodes were removed, especially if many of the nodes contain cancer.
If melanoma tumors are found in nearby lymph vessels in or just under the skin , they should all be removed, if possible. Other options include injections of the T-VEC vaccine , Bacille Calmette-Guerin vaccine, or interleukin-2 directly into the melanoma; radiation therapy; or applying imiquimod cream. For melanomas on an arm or leg, another option might be isolated limb perfusion or isolated limb infusion . Other possible treatments might include targeted therapy , immunotherapy, or chemotherapy.
Some people with stage III melanoma might not be cured with current treatments, so they may want to think about taking part in a clinical trial of newer treatments.
What Symptoms Develop When Melanoma Spreads To The Brain
Many patients feel the same. They dont have any symptoms that would indicate the cancer has spread.
If your doctor thinks that you are at risk for melanoma spreading to your brain, you may need an MRI. An MRI can find cancer in the brain before you have symptoms. Not everyone who has melanoma needs to have an MRI.
When melanoma spreads to the brain and symptoms occur, they may include:
-
Headaches
-
Paralysis on one side of your body
-
Problems with your eyesight
Symptoms tends to occur when the cancer has spread to more than one area of the brain. A large tumor can also cause symptoms.
Recommended Reading: How Bad Is Basal Cell Skin Cancer
Treating Stage Ii Melanoma
Wide excision is the standard treatment for stage II melanoma. The width of the margin depends on the thickness and location of the melanoma.
Because the melanoma may have spread to nearby lymph nodes, many doctors recommend a sentinel lymph node biopsy as well. This is an option that you and your doctor should discuss.
If an SLNB is done and does not find cancer cells in the lymph nodes, then no further treatment is needed, although close follow-up is still important.
If the SLNB finds that the sentinel node contains cancer cells, then a lymph node dissection will probably be done at a later date. Another option might be to watch the lymph nodes closely by getting an ultrasound of the nodes every few months.
If the SLNB found cancer, adjuvant treatment with an immune checkpoint inhibitor or targeted therapy drugs might be recommended to try to lower the chance the melanoma will come back. Other drugs or perhaps vaccines might also be options as part of a clinical trial.
Patients Previously Excluded From Clinical Trials
One reason patients with brain metastases had been excluded from clinical trials is that the blood-brain barrier tight vascular construction of blood vessels serving the brain prevents drugs from reaching tumors. Since immunotherapy empowers T cells to attack tumors, rather than treating tumors directly, the immune system cells can cross the barrier. There were, however, concerns about immune-related side effects.
“We were quite concerned going into the study about immunotherapy causing inflammation and swelling in the brain, so this was closely monitored,” Tawbi says. “In the end, only 5 percent of patients had swelling in the brain.”
The most common brain-related side effect was headache, and most of these side effects were low grade and easily managed. Overall, 52 patients had more challenging side effects, with 19 patients having to leave the trial.
For Wittoesch, the main side effect of the treatment “was like having the flu. I was kind of shaky and sick at times.”
Read Also: Are There Stages Of Basal Cell Carcinoma
Immunotherapy Combination Shows Clinical Benefit
Brain metastases shrank in half of the 94 participants with sufficient follow-up, including 24 participants whose brain metastases were completely eliminated and 28 whose brain metastases shrunk partially. Two other participants had brain metastases that remained stablemeaning, they did not shrink or growfor at least 6 months.
These tumor response rates are similar to response rates for people with metastatic melanoma who dont have brain metastases, Dr. Sharon noted. It appears that patients are benefitting regardless of the site of metastasis.
The responses were rapid, the investigators noted, with some tumor reductions detectable just 6 weeks after the start of treatment. And the responses were durable: 90% of patients whose brain metastases responded to the treatment had an ongoing response 14 months later.
The number of brain metastases a patient had at the time of enrollment did not affect whether the person benefited from the treatment. However, brain metastases were more likely to shrink or remain stable in patients whose tumors had high expression of PD-L1, a biomarker of immunotherapy response, than in patients whose tumors had low PD-L1 expression.
Overall, the response rate for tumors outside of the brain was similar to the response rate for brain metastases.
The Trial Is A Lifesaver

“I’ve never had chemotherapy, but I have seen it up close, and it can be pretty harsh,” she says, referring to her experience as an MD Anderson volunteer and with her father’s treatment years ago.
“Dealing with cancer can be such a difficult fight,” she says. “Without this clinical trial, I wouldn’t be here, and it’s a great pleasure for me to know that this study will be used to help other people.”
Tawbi notes oncologists continue to work with radiation oncologists and neurosurgeons to further improve outcomes and provide the best guidance for patients on initial treatment and the best timing for subsequent treatments, if needed.
“Helping 57 or 58 percent of these patients is significant improvement, but our goal is to reach 100 percent,” Tawbi says.
Read Also: How Bad Is Melanoma Skin Cancer
Recurrence In Nearby Lymph Nodes
If nearby lymph nodes werenât all removed during the initial treatment, the melanoma might come back in these lymph nodes. Lymph node recurrence is treated by lymph node dissection if it can be done, sometimes followed by adjuvant treatments such as radiation therapy and/or immunotherapy or targeted therapy . If surgery is not an option, radiation therapy or systemic treatment can be used.
How Do You Decide Which Metastatic Brain Cancer Treatment Is Right For You
Your neurosurgeon will discuss the most appropriate treatment approach with you by considering these and other factors:
- The type of primary cancer, your response to treatment and current status
- The location and number of metastatic tumors within the brain or spine
- Your general health and preferences regarding potential treatment options
- Your current symptoms
Along with benefits, doctors also consider the potential risks and side effects of any treatment. Many patients are worried about the effects of radiation. Others hesitate about the idea of surgery. Tell your doctor about your concerns they are important to consider.
You May Like: How To Identify Skin Cancer
Improving Access To Clinical Trials For Patients With Brain Metastases
Addressing some of the bigger questions this new study raises will require allowing more people with brain metastases to enroll in clinical trials, Dr. Sharon said.
For example, although the immunotherapy combination seems to be a promising potential treatment for people with metastatic melanoma tumors in the brain, it cant be assumed that it will also benefit higher-risk patients who were excluded from the study, Drs. Turajlic and Larkin wrote.
Being realistic about the patient population, we know that some patients present with neurological symptoms and require treatment with steroids, Dr. Tawbi explained.
Although people with metastatic melanoma who had neurological symptoms or had been treated with steroids were initially excluded from the trial, the investigators later enrolled 20 such patients. The team plans to analyze data from these participants soon.
In addition, nivolumab and ipilimumab are used to treat several kinds of cancerincluding colon, liver, lung, and kidney cancerbut their efficacy on brain metastases of these cancers has not been carefully evaluated. Drs. Turajlic and Larkin stated that future clinical trials for checkpoint inhibitors should include such patients.
Enhancing Healthcare Team Outcomes
Skin cancers are frequently seen by primary care providers, nurse practitioners, internists,;and pharmacists; this is why an interprofessional team approach is needed. While many skin lesions are benign, it is important always to consider melanoma- as it is potentially deadly if the diagnosis gets missed. If there is suspicion of melanoma, the patient should obtain a referral to the dermatologist/oncologist and pathologist for further workup, irrespective of which of the other healthcare providers first became suspicious. Surgery includes wide local excision with sentinel lymph node biopsy, elective node dissection, or both. These surgical procedures are the definitive treatment for early-stage melanoma.
When performing the wide local excision, first consider the surgical margins. If the primary closure is not feasible, skin grafting or tissue transfers may be needed.;Medical management is reserved for adjuvant therapy of patients with advanced melanoma; here again, the pharmacist can monitor medications and consult with the dermatologist. Dermatology nursing staff will assist at all stages of case management, and provide patient counsel and monitor the condition, reporting to the treating clinician as necessary. For localized lesions, the prognosis is with surgery, but advanced melanoma has a;grim prognosis, but the interprofessional team approach to care will optimize the patient’s prospects for a better outcome.;
You May Like: What Does Skin Cancer Look Like On Your Head
Metastatic Brain Cancer Prognosis
Prognosis for metastatic brain cancer varies greatly. Keep in mind that each patient is unique, and with newer treatments, many patients live longer. Speaking with your care team about your unique diagnosis can provide an accurate prognosis.
Palliative Care at Johns Hopkins
Palliative care is specialized medical care that helps patients facing serious illnesses and their families by adding an extra layer of support.
Palliative care teams can help with the symptoms and the stress of living with a serious illness, including controlling pain, providing support for the mental and emotional effects of an illness, and managing other symptoms.
Melanoma Brain Metastasis Presentation And Treatment In The Age Of Targeted And Immunotherapies
- Cancer
You’ve saved your first item
You can find your saved items on your dashboard, in the “saved” tab.
You’ve recommended your first item
Your recommendations help us improve our content suggestions for you and other PracticeUpdate members.
You’ve subscribed to your first topic alert
What does that mean?
Recommended Reading: What Are The Types Of Skin Cancer