Collecting Duct And Other Rare Forms Of Rcc
Collecting duct RCC is a rare but highly aggressive tumor of the distal nephron that shows LOH of chromosome 1q, 6p, 8p, 13q and 21q . Mapping of chromosome 1q , 8p and 13q have narrowed down the region but not yet identified the target suppressor genes. Renal medullary carcinoma described in African-Americans and associated with sickle cell trait, mucinous tubulocystic RCC and other rare forms of RCC have been reviewed in Srigley and Delahunt 2009 .
Tumors With Predominant Clear Cells
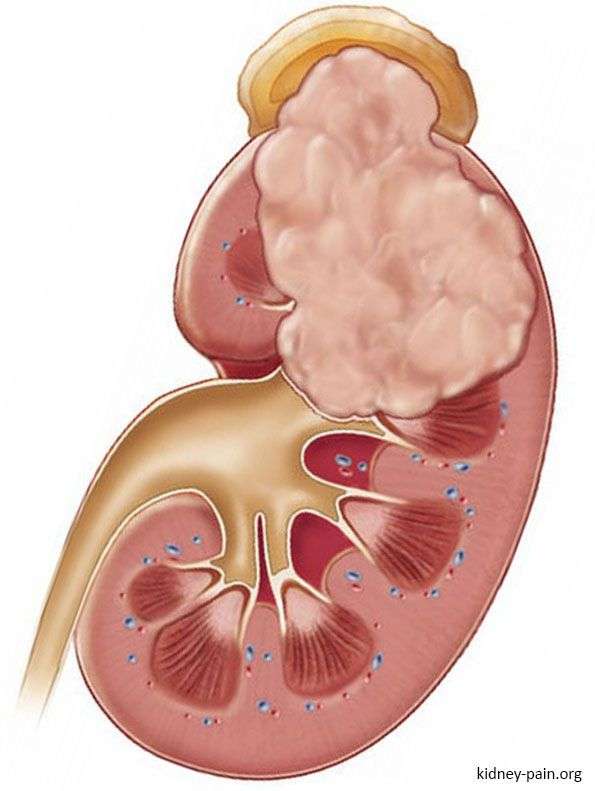
Clear cell renal cell carcinoma encompasses 70% of renal cell carcinomas. It occurs in sporadic form in 95% of all cases and a minor part of them are associated with von Hippel-Lindau disease and other familial syndromes. The typical morphology of tumor cells is clear or granular cytoplasm which gives a typical yellow appearance at gross examination. Architecture may be acinar, nested, alveolar, tubular, solid/cords, and small cysts. A delicate network of capillary vessels is intimately associated with the tumor . Clinical behavior is dependent on the presence of high-grade areas, higher stages, presence of necrosis, and sarcomatoid/rhabdoid morphology. One third of localized disease will developed metastasis during oncologic follow up. Half of patients who developed a post-nephrectomy recurrence will die of the disease .
Fig. 1Fig. 2
A metastatic carcinoma in the brain of a 68-year old female patient with a not biopsied kidney mass. It has minute areas of cytoplasmatic clearing . Most of the tumor showed, however, sarcomatoid morphology . Pan-cytokeratin and PAX8 were diffusely positive. When a kidney primary is considered, the expression of carbonic anhydrase IX in membranous and diffuse pattern is specific for clear cell subtype
Table reviews key recommendations for non-papillary tumors with predominant clear cells.
Table 1 Solid, non-papillary tumors with predominant clear cells
Table reviews key recommendations for papillary tumors with predominant clear cells.
Prognostic Systems For Metastatic Renal Cell Carcinoma
Two similar prognostic systems are commonly used to calculate risk in patients with metastatic renal cell carcinoma . The Memorial Sloan-Kettering Cancer Center /Motzer score includes the following criteria :
- Time from diagnosis to systemic treatment less than 1 year
- Hemoglobin concentration below the lower limit of normal
- Serum calcium concentration > 10 mg/dL
- Lactate dehydrogenase level more than 1.5 times the upper limit of normal
- Performance status less than 80%
The International Metastatic RCC Database Consortium risk model, validated and further developed by Heng et al, includes the following prognostic criteria :
- Time from diagnosis to systemic treatment less than 1 year
- Karnofsky performance status less than 80%
- Hemoglobin concentration below LLN
- Serum calcium above ULN
- Platelet count above the ULN
- Neutrophil count above the ULN
Both systems categorize patients into the following 3 risk groups:
- Favorable risk – Median survival 20 months 2-year overall survival 75%
- Intermediate risk – Median survival 10 months 2y OS 53%
- Poor/high risk group – Median survival 4 months 2y OS 7%
Review of an external validation cohort of 4657 patients treated for kidney cancer in clinical trials from 2003 to 2013 also demonstrated longer overall survival in obese patients, with median overall survivals of 23.4 months versus 14.5 months for those with low BMI.
Recommended Reading: Stage 3 Basal Cell Carcinoma Survival Rate
Looking For More Of An Introduction
If you would like more of an introduction, explore these related items. Please note that these links will take you to other sections on Cancer.Net:
-
ASCO Answers Fact Sheet:Read a 1-page fact sheet that offers an introduction to kidney cancer. This free fact sheet is available as a PDF, so it is easy to print.
The Following Stages Are Used For Renal Cell Cancer:
Stage I
In stage I, the tumor is 7 centimeters or smaller and is found in the kidney only.
Stage II
In stage II, the tumor is larger than 7 centimeters and is found in the kidney only.
Stage III
In stage III, one of the following is found:
- the cancer in the kidney is any size and cancer has spread to nearby lymph nodes or
- cancer has spread to blood vessels in or near the kidney , to the fat around the structures in the kidney that collect urine, or to the layer of fatty tissue around the kidney. Cancer may have spread to nearby lymph nodes.
Stage IV
In stage IV, one of the following is found:
- cancer has spread beyond the layer of fatty tissue around the kidney and may have spread into the adrenal gland above the kidney with cancer or to nearby lymph nodes or
- cancer has spread to other parts of the body, such as the bones, liver, lungs, brain, adrenal glands, or distant lymph nodes.
Recommended Reading: Osteomyoma
What Is The Prognosis Of Papillary Renal Cell Carcinoma
The prognosis of Papillary Renal Cell Carcinoma depends on the size and number of tumors, their localization, and spread.
- The most reliable prognostic factor of Papillary Renal Cell Carcinoma is dependent on whether the tumor can be completely removed through surgery with free margins or not
- The prognosis of PRCC also depends upon a set of several factors, which include:
- Stage of tumor: With lower-stage tumors, when the tumor is confined to site of origin, the prognosis is usually excellent with appropriate therapy. In higher-stage tumors, such as tumors with metastasis, the prognosis is poor
- The surgical respectability of the tumor
- Overall health of the individual. Individuals with overall excellent health have better prognosis compared with those with poor health
- Age of the individual. Older individuals generally have poorer prognosis than younger individuals
- Whether the tumor is occurring for the first time, or is a recurrent tumor. Recurring tumors have worse prognosis compared to tumors that do not recur
- Response to treatment. Tumors that respond to treatment have better prognosis compared to tumors that do not respond to treatment
As with any tumor, it is important to have follow-up appointments with a physician to monitor for any returning tumors.
Role Oflymph Node Invasion In Locally Advanced Rcc
In locally advanced RCC, the role of LND is still controversial. The onlyavailable RCT demonstrated no survival benefit for patients undergoing LND but this trialmainly included organ-confined disease cases . In the settingof locally advanced disease, several papers addressed the topic with contradictory results,as did several systematic reviews. Bhindi et al. couldnot confirm any survival benefit in patients at high risk of progression treated with LND. More recently, Luo etal. reported a systematic review and meta-analyses showing a survival benefit inpatients with locally advanced disease treated with LND . Morespecifically, thirteen studies on patients with LND and non-LND were identified and includedin the analysis. In the subgroup of locally advanced RCC , LND showed asignificantly better OS rate in patients who had undergone LND compared to those without LND.
7.2.2.1.Management of clinically negativelymph nodes in locally advanced RCC
In case of cN-, the probability of finding pathologically confirmed LNmetastases ranges between 0 and 25%, depending mainly on primary tumour size and thepresence of distant metastases . In case of clinically negativeLNs at imaging, removal of LNs is justified only if visible or palpable during surgery, at least for staging, prognosis and follow-up implicationsalthough a benefit in terms of cancer control has not yet been demonstrated . Whether to extend the LND also toretroperitoneal areas without cN+ remains controversial .
You May Like: What Is The Most Aggressive Skin Cancer
Advanced Or Recurrent Kidney Cancer Treatment
For people with advanced kidney cancer that has spread to other parts of the body, treatment with a drug may be recommended along with surgery, or instead of surgery. Some of these drugs are given to you as a pill that you take by mouth others are given as an injection. Much progress has been made in recent years, and people with advanced kidney cancer are living much longer than ten years ago.
- Medicine is often used for advanced kidney cancer that has spread to other parts of the body or where surgery cannot be done.
- Immunotherapy uses the bodys defense system to stop or slow the growth of cancer cells
- Monoclonal antibodies attack a specific part of cancer cells
- Checkpoint inhibitors help the immune system recognize and attack cancer cells
- Vaccines give an overall boost to the immune system
When To Get Medical Advice
See a GP if you have symptoms of kidney cancer.
Although it’s unlikely you have cancer, it’s important to get your symptoms checked out.
The GP will ask about your symptoms and may test a sample of your urine to see if it contains blood or an infection.
If necessary, they may refer you to a hospital specialist for further tests to find out what the problem is.
You May Like: Soderstrom Skin Cancer Screening
Understanding The Spread: Metastatic Renal Cell Carcinoma
Metastatic renal cell carcinoma
Renal cell carcinoma, also called kidney cancer, occurs when cancer cells form in the tubules of the kidney. Tubules are tiny tubes in your kidney that help filter waste products from your blood in order to make urine.
Smoking, hypertension, obesity, and hepatitis C all increase the risk of renal cell carcinoma. Renal cell carcinoma becomes metastatic renal cell carcinoma when it spreads beyond your kidney to your lymph system, bones, or other organs.
Renal cell carcinoma can spread from a mass of cancer cells or tumor to other parts of your body. This process is called metastasis. It occurs in one of three ways:
- Cancer cells spread into the tissue around the tumor in your kidney.
- The cancer moves from your kidney into your lymph system, which has vessels throughout the body.
- Kidney cancer cells enter the bloodstream and are carried and deposited to another organ or location in your body.
When renal cell carcinoma is in its early stages, its unlikely that youll experience obvious symptoms. Noticeable symptoms are often a sign that the disease has metastasized.
Symptoms typically include:
A physical exam and a review of your medical history may prompt further testing to determine the health of your kidneys.
Treatments For Renal Cell Carcinoma
There are five kinds of standard treatments for RCC. One or more may be used to treat your cancer.
Read Also: What Is The Most Aggressive Skin Cancer
Which Imaging Investigations For Whichpatients And When
- The sensitivity of chest radiography and US for detection of small RCC metastases ispoor. The sensitivity of chest radiography is significantly lower than CT-scans, asproven in comparative studies including histological evaluation . Therefore, follow-up for recurrence detectionwith chest radiography and US are less sensitive .
- Positron-emission tomography and PET-CT as well as bone scintigraphy should not be usedroutinely in RCC follow-up, due to their limited specificity and sensitivity .
- Surveillance should also include evaluation of renal function and cardiovascular riskfactors .
- Outside the scope of regular follow-up imaging of the chest and abdomen, targetedimaging should be considered in patients with organ-specific symptoms, e.g. CT or MRIimaging of the brain in patients experiencing neurological symptoms .
A follow-up algorithm for monitoring patients aftertreatment for RCC is needed, recognising not only the patients risk of recurrenceprofile, but also the efficacy of the treatment given . These prognostic systemscan be used to adapt the follow-up schedule according to predicted risk of recurrence.Ancillary to the above, life-expectancy calculations based on comorbidity and age atdiagnosis may be useful in counselling patients on duration of follow-up .
Table 8.1: Proposed follow-up schedule following treatment forlocalised RCC, taking into account patient risk of recurrence profile and treatment efficacy
|
Risk profile |
|
|
CT once yr |
CT once every two yrs |
How Is Ccrcc Diagnosed
Patients with ccRCC may have pain or feel tired. Sometimes, patients do not have any noticeable symptoms. Symptoms can include:
- Blood in the urine
- Fever
- A lump in the side
For people without symptoms, these tumors can be discovered if the person has an imaging test for another reason.
Imaging: If are suspected to have clear cell renal cell carcinoma, your doctor will use imaging scans such as X-rays, CT or MRI to look at the size of the tumor. They will also check for signs that the tumor has spread to other parts of the body.
Biopsy: To check if the tumor is ccRCC your doctor will perform a biopsy, taking a small sample from the tumor with a needle. An expert, called a pathologist, will study cells from the sample under the microscope to see what kind of tumor it is.
You May Like: Etiology Of Basal Cell Carcinoma
Clinical Features Of Ccrcc
Clear cell renal cell carcinoma is more likely to be symptomatic at presentation compared with other histologic variants of RCC .
The most common signs and symptoms reported for patients presenting clinically with RCC in modern surgical series include the following:
-
Anemia
Symptoms reported in less than 10% of patients include the following:
-
Thrombocytosis
-
A flank or abdominal mass
-
Hypertension
-
Erythrocytosis
-
Chills
All of the above signs and symptoms can occur in patients with localized as well as metastatic disease. Many of them represent paraneoplastic syndromes.
However, approximately 46% of patients with RCC in modern surgical series are asymptomatic, with the tumor diagnosed incidentally during abdominal radiologic imaging for unrelated symptoms. This reflects the introduction of high-resolution ultrasonography and computed tomography in the 1980s, which has increased the detection rate for RCC, in particular the detection of tumors smaller than 3 cm in maximal diameter.
The differential diagnosis of clear cell renal cell carcinoma is as follows:
-
Chromophobe RCC, eosinophilic variant
-
Papillary RCC with clear cell change
-
Clear cell papillary RCC
Treatment Of Stage Iii Renal Cell Cancer
For information about the treatments listed below, see the Treatment Option Overview section.
- Surgery . Blood vessels of the kidney and some lymph nodes may also be removed.
- Arterial embolization followed by surgery .
- Arterial embolization as palliative therapy.
- Surgery as palliative therapy.
- Radiation therapy before or after surgery .
- A clinical trial of biologic therapy following surgery.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Don’t Miss: Amelanotic Melanoma Blanch
Radiographic Investigations To Evaluate Rccmetastases
Chest CT is accurate for chest staging . Use of nomograms tocalculate risk of lung metastases have been proposed based on tumour size, clinical stageand presence of systemic symptoms .These are based on large, retrospective datasets, and suggest that chest CT may be omittedin patients with cT1a and cN0, and without systemic symptoms, anaemia or thrombocythemia,due to the low incidence of lung metastases in this group of patients. There is aconsensus that most bone metastases are symptomatic at diagnosis thus, routine bone imagingis not generally indicated . However, bone scan, brain CT, or MRI may be used inthe presence of specific clinical or laboratory signs and symptoms . A recent prospective comparative blinded study involving 92 consecutive mRCC patientstreated with first-line VEGFR-TKI found that whole-body DWI/MRIdetected a statistically significant higher number of bony metastases compared withconventional thoraco-abdomino-pelvic contrast-enhanced CT, with higher number ofmetastases being an independent prognostic factor for progression-free survival and OS.
Prognosis And Predictive Factors
Patients with clear cell renal cell carcinoma tend to have a worse prognosis than patients with other histologic subtypes of RCC, with 5-year disease-specific survival rates of 50-69%, compared with 67-87% for papillary RCC and 78-87% for chRCC. However, analysis of 1000 patients showed very similar 5-year disease-specific survival rates for CCRCC and papillary RCC once metastatic disease was present.
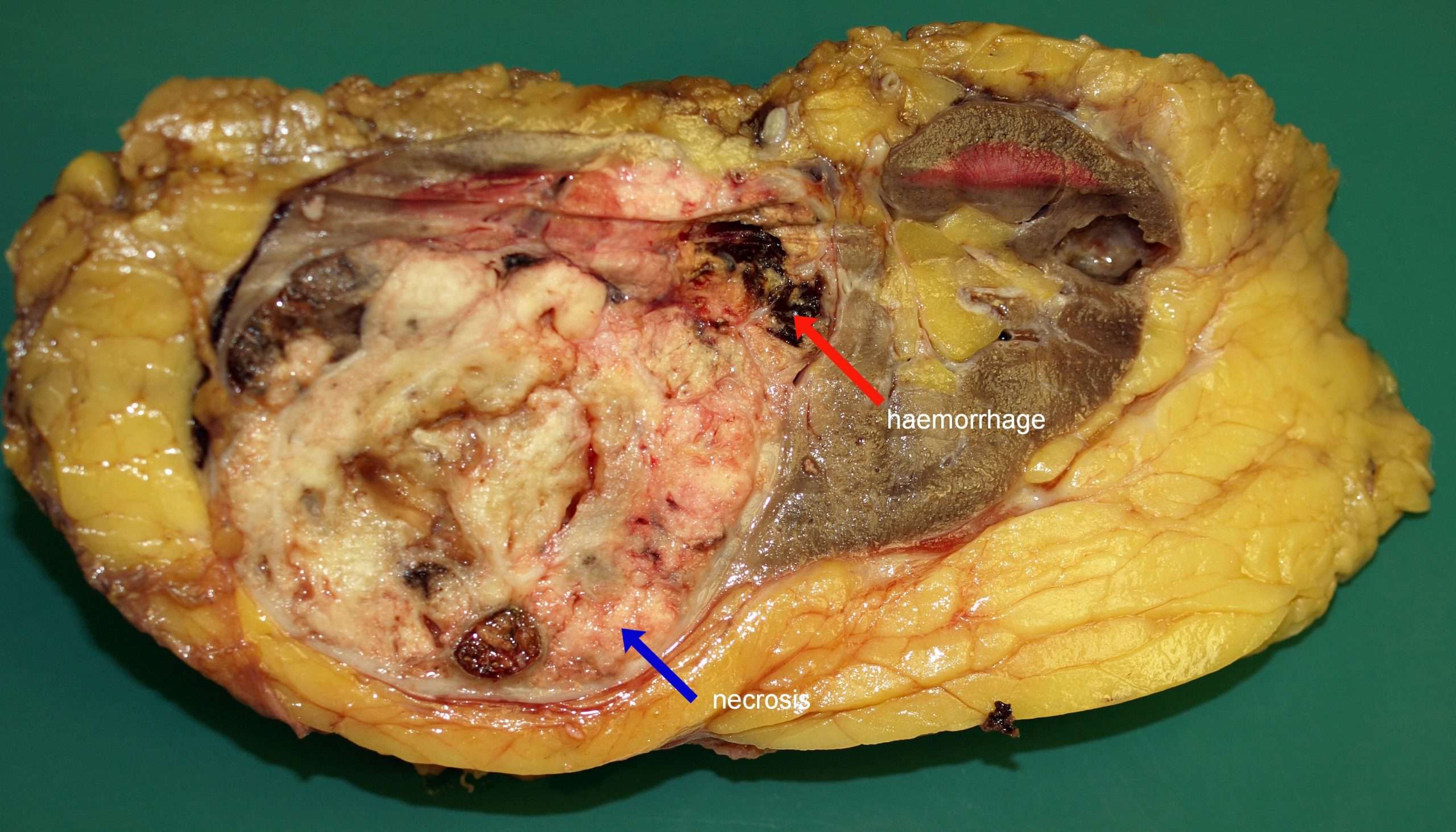
Multivariate analyses indicate that histologic RCC subtype has no significant independent value for predicting cancer-specific survival because prognosis is primarily dependent upon TNM stage and Fuhrman nuclear grade. Multivariate analysis specifically of CCRCC cases shows that in addition to the 3 separate components of tumor staging , other significant independent predictors of poor prognosis are nuclear grade, tumor size, and the presence of histologic necrosis or sarcomatoid differentiation.
Rhabdoid differentiation is also observed in CCRCC and seems to impart a poor outcome similar to sarcomatoid change however, this factor has not yet been tested in predictive models. Interestingly, histological necrosis is seen more commonly in papillary RCC but is not a significant predictor of poor prognosis for papillary RCC, even in univariate analyses.
References
Delahunt B, Eble JN. History of the development of the classification of renal cell neoplasia. Clin Lab Med. 2005 Jun. 25:231-46, v. .
Pascual D, Borque A. Epidemiology of kidney cancer. Adv Urol. 2008. 782381. .
Also Check: Does Amelanotic Melanoma Blanch When Pressed