An Unevenly Pigmented Patch Of Skin
In people of color, melanoma doesnt always show up as a mole. Sometimes it just looks like a dark lesion or patch of dark skin. And it often surfaces in places you wouldnt expect melanoma to grow: the soles of your feet or the palms of your hands. Melanoma in dark skin is far less common than it is in fair complexions, but when it does happen, its often deadlier because its typically found at a later stage. One more reason to be attuned to any changes in your body!
How To Treat Melanoma
Once your doctor has confirmed that your changing mole is indeed melanoma, your treatment will largely depend on how far the cancer has progressed and your overall health.
Melanoma in its earliest stages is often treated by surgery to remove the melanoma and a portion of skin surrounding it, according to the ACS. If the cancer has already progressed to a more advanced stage, your doctor may recommend surgery in conjunction with immunotherapy, radiation therapy, chemotherapy, or newer targeted therapy drugs.
Again, while melanoma is not exactly a common skin cancer, it causes the most deaths, so catching it and treating it early is key. Even better? Keep your skin healthy by staying out of the suns harmful UV rays when possible. Regardless if you have fair or dark skin, wearing sun-protective clothing, a hat, hanging out in the shade when possible, and reapplying a broad spectrum sunscreen with an SPF 30 or higher every two hours will go a long way in keeping melanoma out of your future.
Stay updated on the latest science-backed health, fitness, and nutrition news by signing up for the Prevention.com newsletter here.
Take our survey on healthcare during COVID and beyond, tooyour voice matters.
How To Tell A Melanoma From A Scary Mole
by Tim Daly | Feb 22, 2017 | Blog, Skin Cancer
Telling whether an odd looking mole is a melanoma is a real challenge. In fact, the only sure way to know is with a biopsy. But, before you get them all cut out, there are signs and symptoms that can help you and your doctor to make the right decision.
According to the National Cancer Institute there are three main kinds of moles you need to know about: a common mole, a dysplastic mole, and a melanoma.
What is a common mole?A common mole is a small growth on the skin usually found above the waist on areas exposed to the sun, and rarely found on the scalp, breast, or buttocks. If you have more than 50 common moles you have a greater chance of developing melanoma. That said, most common moles do not turn into melanoma.
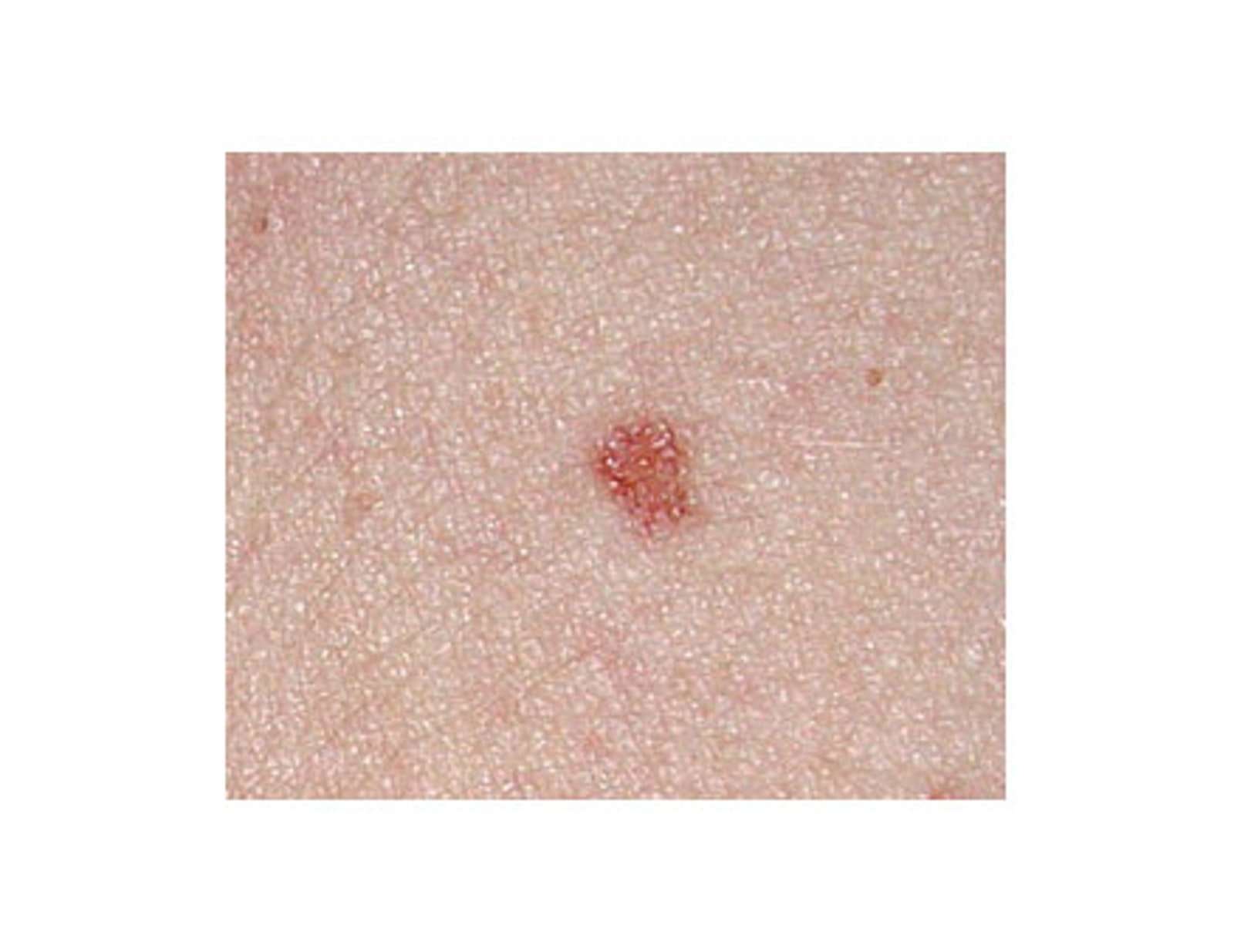
What do they look like?They are usually smaller than about 5 millimeters wide, just less than the width of a pencil eraser. They are round or oval, have a smooth surface with a distinct edge, and can be dome-shaped. They usually have an even pink, tan, or brown colour. People who have dark skin or hair tend to have darker moles than people with fair skin or blonde hair. Below are a few photos of common moles:
People with dark skin are much less likely than people with fair skin to develop melanoma. When it does develop in people with dark skin, it is often found under the fingernails, under the toenails, on the palms of the hands, or on the soles of the feet.
Common Mole
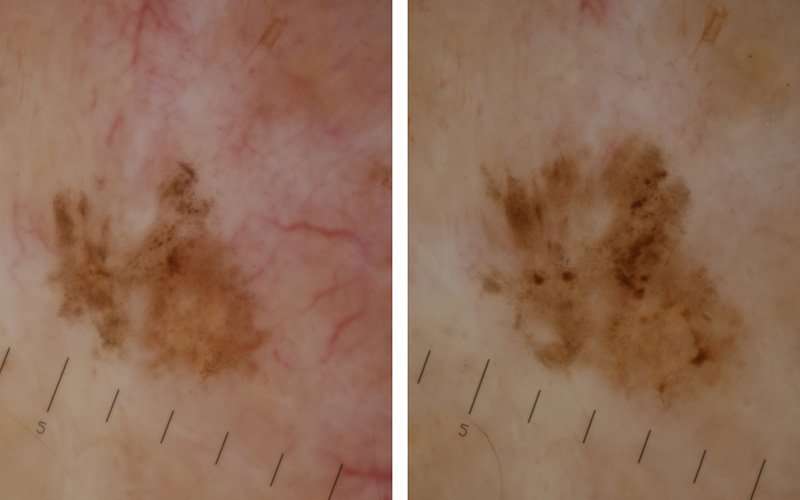
Dysplastic Mole
Recommended Reading: What Is The Survival Rate For Invasive Ductal Carcinoma
A Dark Line In Your Nail
When melanoma pops up on your nails, it looks more like a bruise under your nail plate, says Heather Woolery-Lloyd, M.D., director of the skin of color division in the department of dermatology of the University of Miami. Called subungual melanoma, which translates to melanoma beneath a fingernail or toenail, this type typically shows up as a dark, vertical line down the length of your nail. Over time, the line may spread, covering more of your nail. Its also known as acral lentiginous melanoma , melanoma on your hands, feet, or nails.
Early Warning Signs Of Melanoma
The key to detecting melanoma early is to know what to look for and where to look for it. This isnt always easy, as melanoma can be a master of disguise. It may look like an age spot, a bruise, a sore, a cyst, a scar or a dark line beneath your nail. You may not feel a melanoma, but there are times that it may itch, hurt or bleed.
The ABCDE method may help you determine whether an abnormal skin growth may be melanoma:
- A is for asymmetry: Does the mark look different on each half?
- B is for border: Are the edges jagged or irregular?
- C is for color: Is your lesion uneven in color with specks of black, brown and tan?
- D is for diameter: Is your lesion getting larger?
- E is for evolving or elevation: Has your lesion changed in size, shape or texture over the past few weeks or months?
If the answer to any of these questions is yes, or even maybe, see a dermatologist for a proper evaluation. The only way to be sure whether a mole is melanoma is to visit a doctor.
Other melanoma warning signs may include:
- Sores that dont heal
- Pigment, redness or swelling that spreads outside the border of a spot to the surrounding skin
- Itchiness, tenderness or pain
Read Also: Can You Die From Basal Cell Skin Cancer
What Happens At Follow
The primary purpose of follow-up is to detect recurrences early, but it also offers an opportunity to diagnose a new primary melanoma at the first possible opportunity. A second invasive melanoma occurs in 5-10% patients an unrelated melanoma in situ affects in more than 20% of melanoma patients.
The Australian and New Zealand Guidelines for the Management of Melanoma make the following recommendations for follow-up for patients with invasive melanoma.
- Self-skin examination
- Routine skin checks by a patient’s preferred health professional
- Follow-up intervals are preferably six-monthly for five years for patients with stage 1 disease, three-monthly or four-monthly for five years for patients with stage 2 or 3 disease, and yearly after that for all patients.
- Individual patients needs should be considered before an appropriate follow-up is offered
- Provide education and support to help the patient adjust to their illness
The follow-up appointments may be undertaken by the patient’s general practitioner or specialist, or they may be shared.
Follow-up appointments may include:
- A check of the scar where the primary melanoma was removed
- A feel for the regional lymph nodes
- A general skin examination
- A full physical examination
- In those with many moles or atypical moles, baseline whole-body imaging and sequential macro and dermoscopic images of melanocytic lesions of concern
In those with more advanced primary disease, follow-up may include:
Get To Know Your Skin
The sooner a skin cancer is identified and treated, the better your chance of avoiding surgery or, in the case of a serious melanoma or other skin cancer, potential disfigurement or even death.
It is also a good idea to talk to your doctor about your level of risk and for advice on early detection.
It’s important to get to know your skin and what is normal for you, so that you notice any changes. Skin cancers rarely hurt and are much more frequently seen than felt.
Develop a regular habit of checking your skin for new spots and changes to existing freckles or moles.
Also Check: What Is The Survival Rate For Invasive Ductal Carcinoma
How To Diagnose Skin Cancer
First, a doctor will examine a personâs skin and take their medical history. They will usually ask the person when the mark first appeared, if its appearance has changed, if it is ever painful or itchy, and if it bleeds.
The doctor will also ask about the personâs family history and any other risk factors, such as lifetime sun exposure.
They may also check the rest of the body for other atypical moles and spots. Finally, they may feel the lymph nodes to determine whether or not they are enlarged.
The doctor may then refer a person to a skin doctor, or dermatologist. They may examine the mark with a dermatoscope, which is a handheld magnifying device, and take a small sample of skin, or a biopsy, and send it to a laboratory to check for signs of cancer.
What Are The Causes Of & Risk Factors For Scalp Melanoma
Sun exposure is the leading cause of all forms of melanoma. Because the scalp often receives a significant amount of sun exposure, that means there is a high risk for melanoma and other forms of skin cancer in this area. In addition to sun exposure, regularly visiting tanning beds, radiation treatment, and chemical exposure can all contribute to the development of skin cancers.
In addition to the underlying causes of skin cancer, numerous factors can increase the risk of developing scalp melanoma, including:
- Taking immunosuppressive medications
Don’t Miss: What Is The Survival Rate For Invasive Ductal Carcinoma
Pigmentation In Your Gums
A dark spot on your gums can signal mucosal melanoma, an extremely rare form of the skin cancer that appears on mucus membranesin your mouth, your nose, genitals, and even within your respiratory and GI tracts. Mucosal melanoma accounts for 1.4% of all melanoma cases, but its particularly lethal compared to other forms of the disease. Aside from pigmented lesions in these mucous-lined areas, other symptoms may include pain, bleeding, lumps, or changes in your GI tract such as diarrhea or constipation.
Not Every Melanoma Is Black
1 September 2016
West Australian nurse Amanda Whittle never imagined a small pink mark on her upper arm was anything to be concerned about. The spot didn’t resemble anything she knew about skin cancers. It wasn’t black or raised, hadn’t grown from a mole or freckle and she couldn’t remember it changing shape, size or colour.
When her dermatologist noticed the mark at her annual skin check and insisted on a biopsy, Amanda, aged 51, was surprised and shocked.
“I had previously noticed the spot six months prior, but there was nothing about it that raised my suspicions at all because it was pink. It was hardly even raised. I thought my dermatologist would simply burn it off next time I saw her,” Amanda explains.
“When the biopsy report came back two days later and my dermatologist said it was an amelanotic melanoma, you could have knocked me over with a feather. I hadnt heard that name before. Here I was a nurse, looking after my skin, and I’d never even heard of this type of skin cancer.”
Thankfully for Amanda however, regular skin checks meant the skin cancer was picked up and treated early with surgery.
“Although it was a very small lesion, the surgeon removed quite a lot of tissue as it was a level 3 melanoma. I have ended up with a very long 15-16 centimetre excision, but my surgeon is confident it is all clear,” Amanda says.
Nine months on since diagnosis and treatment, Amanda says her journey has been harder to overcome that she first realised.
Also Check: Melanoma Bone Cancer Life Expectancy
Tips For Screening Moles For Cancer
Examine your skin on a regular basis. A common location for melanoma in men is on the back, and in women, the lower leg. But check your entire body for moles or suspicious spots once a month. Start at your head and work your way down. Check the “hidden” areas: between fingers and toes, the groin, soles of the feet, the backs of the knees. Check your scalp and neck for moles. Use a handheld mirror or ask a family member to help you look at these areas. Be especially suspicious of a new mole. Take a photo of moles and date it to help you monitor them for change. Pay special attention to moles if you’re a teen, pregnant, or going through menopause, times when your hormones may be surging.
Melanomas That Could Be Mistaken For A Common Skin Problem
Melanoma that looks like a bruise
Melanoma can develop anywhere on the skin, including the bottom of the foot, where it can look like a bruise as shown here.
Melanoma that looks like a cyst
This reddish nodule looks a lot like a cyst, but testing proved that it was a melanoma.
Dark spot
In people of African descent, melanoma tends to develop on the palm, bottom of the foot, or under or around a nail.
Did you spot the asymmetry, uneven border, varied color, and diameter larger than that of a pencil eraser?
Dark line beneath a nail
Melanoma can develop under a fingernail or toenail, looking like a brown line as shown here.
While this line is thin, some are much thicker. The lines can also be much darker.
Don’t Miss: Etiology Of Skin Cancer
What Are The Differences Between A Common Mole A Dysplastic Nevus And A Melanoma
Common moles, dysplastic nevi, and melanoma vary by size, color, shape, and surface texture. The list below summarizes some differences between moles and cancer. Another important difference is that a common mole or dysplastic nevus will not return after it is removed by a full excisional biopsy from the skin, but melanoma sometimes grows back. Also, melanoma can spread to other parts of the body.
Common Mole
What Are The Signs And Symptoms Of Actinic Keratosis
An actinic keratosis develops when skin has been badly damaged by ultraviolet light from the sun or indoor tanning.
Signs of actinic keratosis
The brown spots on this mans face may look like age spots, but theyre actually actinic keratoses.
Left untreated, some actinic keratoses turn into a type of skin cancer called squamous cell carcinoma. Thats why its important to know if you have any of these precancerous growths on your skin.
The following pictures show some diverse ways that it can appear.
You May Like: Can You Die From Basal Cell Skin Cancer
Does An Actinic Keratosis Hurt
While most people see only a change to their skin, an AK can:
-
Itch
-
Feel tender or painful when touched
-
Stick to your clothing, causing discomfort
-
Bleed
If you find a change on your skin that could be an actinic keratosis, protect your health by seeing a board-certified dermatologist. Should that change be an AK, you have a greater risk of developing skin cancer. Being under the care of a board-certified dermatologist helps to find skin cancer early when its highly treatable.
While having skin thats been badly damaged by the sun or indoor tanning greatly increases your risk of developing AKs, other things can increase your risk. Youll find out what else may increase your risk of developing AKs at, Actinic keratosis: Causes.
Related AAD resources
ImagesImages 1,2, and 9: Used with permission of the American Academy of Dermatology National Library of Dermatologic Teaching Slides.
Images 3,4,5,6,7,8,10: Used with permission of the Journal of the American Academy of Dermatology:
-
Image 3: J Am Acad Dermatol. 2017 76:349-50.
-
Image 4: J Am Acad Dermatol. 2007 56:125-43.
-
Image 5: J Am Acad Dermatol. 2013 69:e5-e6.
-
Image 6: J Am Acad Dermatol. 2010 62:85-95.
-
Images 7, 8: J Am Acad Dermatol. 2012 66:173-84.
-
Image 10: J Am Acad Dermatol. 2000 42 part 2:S8-S10.
Rigel DS, Cockerell CJ, et al. Actinic keratosis, basal cell carcinoma, and squamous cell carcinoma. In: Bolognia JL, et al. Dermatology. . Mosby Elsevier, Spain, 2008:1645-58.
What Does Scalp Melanoma Look & Feel Like
When it comes to looking for scalp melanoma, Dr. Walker says, Because of hair growth and general difficulty clearly seeing the top of the head, it can be a challenge to see melanoma forming on the scalp. In addition to your own examinations, you may also want to chat with your hair professional. If one person regularly cuts your hair, they may be in a unique position to screen for common warning signs of scalp melanoma, so chat with your barber or stylist at your next appointment.
The first step to finding scalp melanoma is simple you need to know what youre looking and feeling for. Melanoma on any area of the skin usually looks like common skin conditions, which is one of the main reasons why its overlooked on other parts of the body. Melanomas may be mistaken for warts, moles, freckles, age spots, ulcers, or sores, and in some cases, they grow out of pre-existing skin growths. Melanoma lesions may bleed regularly, feel painful, or tingle.
To differentiate between benign skin lesions and potential scalp melanoma, keep the ABCDEs of skin cancer in mind:
- A Asymmetry Are the sides of the mole the same, or are they noticeably different?
- B Border Do the edges of the spot look jagged or otherwise atypical?
- C Color Is the color different from other spots on your body, or does the color vary throughout the lesion?
- D Diameter Is the mole larger than 6 mm ?
- E Evolution Is the mole changing in any way ?
You May Like: Brain Melanoma Treatment
Should People Have A Doctor Remove A Dysplastic Nevus Or A Common Mole To Prevent It From Changing Into Melanoma
No. Normally, people do not need to have a dysplastic nevus or common mole removed. One reason is that very few dysplastic nevi or common moles turn into melanoma . Another reason is that even removing all of the moles on the skin would not prevent the development of melanoma because melanoma can develop as a new colored area on the skin . That is why doctors usually remove only a mole that changes or a new colored area on the skin.
Referral Pathways And Management
If a patient with a suspected malignant melanoma is seen in primary care there are clear referral pathways for urgent/red flag referral to secondary care. The National Institute for Health and Care Excellence Referral Guidelines for Suspected Cancer state that an urgent referral to a dermatologist or other suitable specialist with experience of melanoma diagnosis should be made and excision in primary care avoided.
The Northern Ireland Cancer Network has issued clear guidance for referral of suspected skin cancer into secondary care . As mentioned previously, a changing lesion or a score of 3 or more in the Glasgow 7-point checklist is suspicious of melanoma. The importance of clear accurate clinical information cannot be emphasized enough as this allows patients to be triaged appropriately and therefore seen in a timely manner. Patients should be referred into secondary care as a red flag and are seen within 2-weeks. It is emphasised in the NICE Guidance that such lesions should not be excised in primary care and strongly recommended that incisional or incomplete excisions are avoided, particularly because of sampling error and the risk of inaccurate diagnosis. All excised skin specimens even those regarded as benign should be sent for histopathological analysis. The practitioner should also maintain a fail-safe log of all procedures performed with details of the outcome and action following histological diagnosis.
Read Also: What Is The Survival Rate For Invasive Ductal Carcinoma