What Is Estrogen Receptorpositive Breast Cancer And Progesterone Receptorpositive Breast Cancer
Cells from your breast cancer can be tested for receptors on two hormones that can fuel cancer growth: estrogen and progesterone. Receptors are special proteins on cells that attach to certain substances, such as estrogen and progesterone, much like a key entering a lock. Breast cancer can contain receptors for one of these hormones, both, or neither.
- Breast cancer with receptors for estrogen is called estrogen receptor positive, or ER positive.
- Breast cancer with no receptors for estrogen is called estrogen receptor negative, or ER negative.
- Breast cancer with receptors for progesterone is called progesterone receptor positive, or PR positive.
- Breast cancer with no receptors for progesterone is called progesterone receptor negative, or PR negative.
If your cancer is ER positive, PR positive, or positive for both estrogen and progesterone receptors, your treatment may include a hormone therapy a drug or drugs that keep these hormones from plugging into their receptors. The idea is to cut off the cancers access to the fuel that would otherwise power its growth, much like putting a child safety cap on an electrical outlet.
What Is Metaplastic Carcinoma
Also known as metaplastic breast cancer, metaplastic carcinoma is a rare type of invasive breast cancer with a unique characteristic: It contains a mix of two or more types of breast cancer cells, usually carcinoma combined with sarcoma. Metaplastic means that one form is turning into another. Various leading-edge techniques are used to analyze the exact genetics and biology of these confused cancers to find out if the tumor is more similar to carcinoma or sarcoma, since these two types of cancer have very different treatments.
What Are The Signs Of Invasive Breast Cancer
Breast cancer may have no signs or symptoms, especially during the early stages. As the cancer grows, you may notice one or more of the following:
- A lump or thickening in or near the breast or in the underarm that continues after your monthly menstrual cycle
- A mass or lump, which may feel as small as a pea
- A change in the size, shape, or contour of the breast
- A blood-stained or clear fluid from the nipple
- A change in the feel or appearance of the skin on the breast or nipple — dimpled, puckered, scaly, or inflamed
- Redness of the skin on the breast or nipple
- A change in shape or position of the nipple
- An area that is distinctly different from any other area on either breast
- A marble-like hardened area under the skin
You may notice changes when you do a monthly breast self-exam. By doing a regular self-check of your breast, you can become familiar with the normal changes in your breasts.
Recommended Reading: Melanoma Stage 2 Treatment
Tumor Size Or Clinical Features On Diagnosis
Tumor size, as a single prognostic factor in DCIS, has remained controversial amongst medical experts.
Whilst many cases of DCIS are diagnosed by mammography and are not palpable on diagnosis some present as a clinical, palpable mass .
Narod, following a 2014 medical study, asserts that:-
Tumour size and palpability are risk factors for breast cancer recurrence and mortality.
One small, 2006 medical study concluded that higher rates of invasive caner were detected according to tumor size. Progression to invasive cancer occurred in 10% of DCIS patients with a tumor size between 2.5 to 3.5 cms, 57% for tumor size 3.6 to 4.5 cms and 71% for tumors between 4.5 and 6 cms.
This study concluded that tumors over 2.5 cms have a higher risk of progressing to invasive cancers. However, the study stresses the correlating importance of axillary node involvement.
Recommended Reading: How Common Is Renal Cell Carcinoma
Papillary Breast Cancer Diagnosis
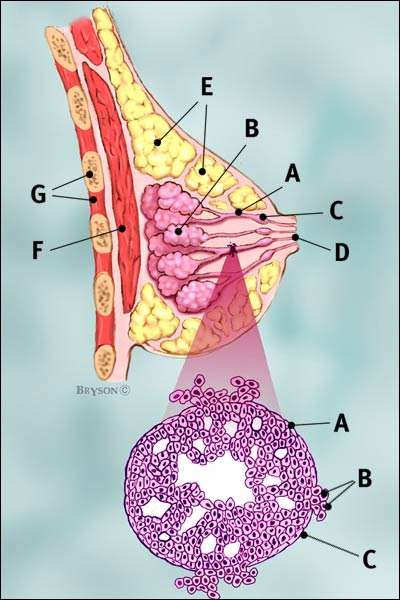
Papillary breast cancer is a very rare type of invasive ductal breast cancer that accounts for fewer than 1% of all breast cancers. The name comes from finger-like projections, or papules, which are seen when the cells are looked at under the microscope.
Many papillary tumors are benign. These are called papillomas. Even when a biopsy is negative for cancer, the pathologist often needs to look at the whole tumor under the microscope to be sure about the diagnosis. This is why surgery to remove a papilloma is usually recommended, even if it is thought to be benign.
Malignant papillary tumors are a form of breast cancer. Like other types of invasive ductal cancer, papillary breast cancer begins in the milk duct of the breast. Most of the time, papillary breast cancers include both in situ cells and invasive cells .
Papillary breast cancers are usually small, and positive for the estrogen and/or progesterone receptors and negative for the HER2 receptor . Compared to more common types of breast cancers, papillary breast cancers are less likely to involve the lymph nodes, are more responsive to treatment, and may have a better prognosis than more common types of invasive ductal cancer.
Also Check: Melanoma 3c
Papillary Breast Cancer Treatment
Local therapy is aimed at preventing the cancer from coming back in the breast. Local therapy includes surgery , and may include radiation.
Systemic therapy is used to prevent the disease from coming back or spreading to another part of the body. This may include endocrine therapy, chemotherapy, and therapy that targets the HER2 protein. Often different types of treatment are used together to achieve the best result.
Your treatment plan will be based on the features of the tumor and the stage of the disease . Your oncology team will recommend a treatment plan based on what is known about papillary breast cancer in general and tailored to your specific disease.
We know that it can be stressful to receive a diagnosis of breast cancer, and learning that you have a rare form of the disease can add to your anxiety. We hope it will be reassuring to know that our team at the Center for Rare Breast Tumors is dedicated to latest research and treatment of papillary breast cancer, and is here to support patients and their families through diagnosis, treatment, and survivorship.
Request an Appointment
Models Of Dcis Progression To Breast Cancer
The conventional model of DCIS progression to breast cancer goes something like this:-
- Atypical ductal hyperplasia
But there are alternative models emerging now, suggesting that DCIS does not necessarily have to be of a high grade before transforming into an invasive breast cancer.
Some breast cancer researches propose that if certain features are present in an intermediate grade DCIS, such as a certain nuclear feature or the presence and degree of necrosis, then the carcinoma might proceed directly to invasive breast cancer status.
This has not been definitively proven, but there is a general consensus that the presence of necrosis in any early stage breast carcinoma is usually considered as an indicator of a potentially more aggressive breast cancer.
By and large, however, it would appear that analysis of the nuclear grade and not the presence, degree, and pattern of necrosis, is the more consistent indicator of malignancy in breast carcinoma. Moreover, some researchers believe that high grade DCIS is itself a unique genetic pattern, that may not develop from low and intermediate grade DCIS.
Also Check: Carcinoma Causes
What Can I Expect If I Have Invasive Ductal Carcinoma
If youve been diagnosed with invasive ductal carcinoma, your healthcare provider will discuss your treatment options with you in detail. For best results, youll want to begin treatment as soon as possible.
How curable is invasive ductal carcinoma?
Invasive ductal carcinoma is quite curable, especially when detected and treated early.
What is the survival rate for invasive ductal carcinoma?
The five-year survival rate for localized invasive ductal carcinoma is high nearly 100% when treated early on. If the cancer has spread to other tissues in the region, the five-year survival rate is 86%. If the cancer has metastasized to distant areas of your body, the five-year survival rate is 28%.
Keep in mind that survival rates cannot tell you how long you will live. These numbers are based on people who have undergone breast cancer treatment in the past. For more information about your specific case, talk to your healthcare provider.
What Are The Treatment Options For Stage 3 Breast Cancer
Another way a doctor may describe stage 3 breast cancer is if its operable or inoperable. This will determine further treatments.
If a cancer is operable, this means a doctor believes most or all of the cancer can be removed with surgery.
Inoperable cancer is still treatable with systemic therapy, but surgery isnt the right option because doctors feel they cant remove enough cancerous cells.
Treatment options for stage 3 breast cancer may include:
- Surgery: known as a mastectomy, to remove cancerous tissue and also to remove lymph nodes
- Hormone therapy: to slow or stop the growth of cancerous cells, if hormones are driving their growth
- Chemotherapy: involves taking medications to kill fast-growing cancer cells
- Targeted therapy: uses your genes to attack cancer cells without harming healthy cells
Your doctor may also recommend a combination of two or more treatments.
Also Check: What Is Stage 2 Squamous Cell Carcinoma
How Is Prognosis Estimated
Prognosis is estimated by looking at what has happened over many years to large groups of people diagnosed with a similar cancer. However, everyones situation is different so no one can say for certain what will happen to you. Also, treatments and survival rates are constantly improving, which affects the accuracy of estimates for people being treated today.
Prognosis is described in different ways. It may be put into words or numbers. Its often expressed as a five- or ten-year survival rate. This is an estimate of how many people are likely to be alive five or ten years following their diagnosis.
A 90% five-year survival rate means that 90 out of 100 people diagnosed with breast cancer are likely to be alive five years after their diagnosis. It doesnt mean these people will only live for five years it just states how many people are likely to be alive at that point.
Cancer Research UK has general statistics on five- and ten-year breast cancer survival rates on their website. Remember, these statistics are based on large groups of patients and cannot predict what will happen in your individual case.
Some Cases Of Dcis Will Progress Towards Invasive Breast Cancer If Left Untreated
There is a general consensus that DCIS may represent a transitional stage between the normal breast tissue and invasive breast carcinoma.
However, it is still largely unknown which types of DCIS are non-progressing towards invasive breast cancer if left untreated.
One recent study estimated that only between 100 to 270 cases of DCIS per 100000 will not progress to invasive breast cancer if left untreated.
A medical study from the United Kingdom examined 84 breast cancer screening units. This large research study looked at DCIS diagnoses between the years of 2003 and 2007 for women aged 50 to 64 years.
Data from over 5,243,658 was analyzed. The average frequency of DCIS detected was 1.60 per 1000 women. The study found that for every 3 cases of DCIS detected on screening there was one less case of invasive cancer in the next 3 years.
Donât Miss: What Does Skin Cancer On Your Lip Look Like
You May Like: Cancer Lesion Pictures
For Microinvasive Dcis Breast Conserving Surgery With Radiation Is Usually Considered The Most Reasonable Approach
Because of the high rates of survival and freedom from distant metastases and because of the ability to salvage patients with local recurrence, breast-conserving surgery and definitive irradiation should continue to be considered as an alternative to mastectomy for appropriately selected and staged patients with microinvasive ductal carcinoma of the breast. However, virtually all microinvasive ductal carcinoma tumors which eventually metastasize are shown to be tumors with a T1 invasive status.
Are Women Opting Against Ductal Carcinoma In Situ Treatment
Its no surprise that these results were met with some raised eyebrows and of course concerns in the medical community, especially considering DCIS is almost exclusively diagnosed by mammography and some women may view these findings as a green light to cancel those appointments or ignore a diagnosis of DCIS.
Yet, there is no right way to treat DCIS. Like any cancer, there are a variety of factors at play ranging from the biology of the tumor and patients age to menopausal status and lifestyle.
The most common type of non-invasive breast cancer, DCIS, is considered non-invasive because it has not yet spread beyond the milk ducts to the surrounding tissue. While this type of breast cancer isnt life threatening, having DCIS can increase a womans chance of later developing invasive breast cancer.
So the question remains: does it matter if I have DCIS? Should I opt for a double mastectomy, no mastectomy, lumpectomy? Or should I do nothing? Of course, there is no simple answer when it comes to the treatment of breast cancer and that logic holds true for women facing a DCIS diagnosis. We are all unique individuals armed with a vast array of biological characteristics and risks and physicians must treat your cancer with this same multi-faceted approach.
You May Like: Lobular Breast Cancer Survival Rates
Invasive Ductal Carcinoma Not Otherwise Specified
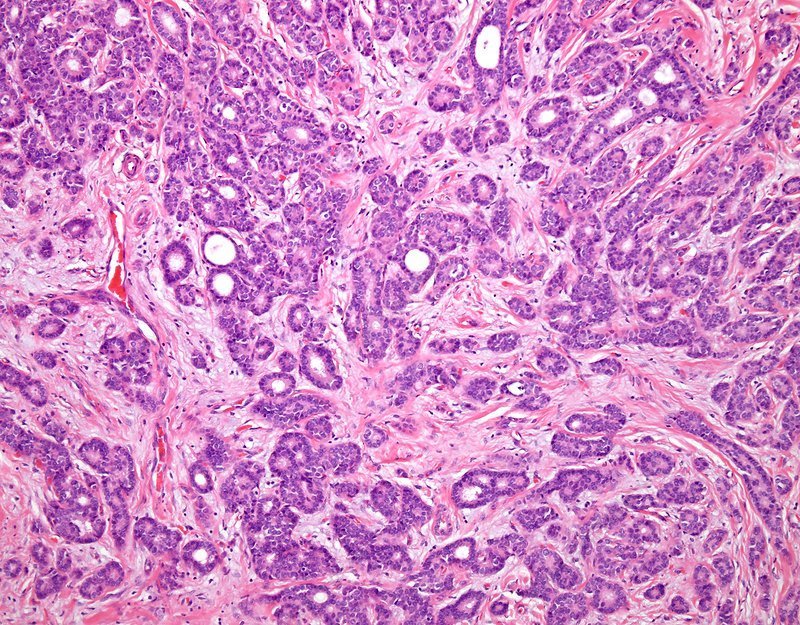
The most common type of invasive breast carcinoma, accounting for approximately 70% of breast carcinomas. The gross appearance is usually typical with an irregular stellate outline. Microscopically, randomly arranged epithelial elements are seen. When large sheets of malignant cells are present, necrosis may be seen. With adequate tissue sampling, in situ carcinoma can be demonstrated in association with the infiltrating carcinoma. The in situ component is nearly always ductal but occasionally may be lobular or both.
What Are The Symptoms Of Inflammatory Breast Cancer
Symptoms of inflammatory breast cancer include swelling and redness that affect a third or more of the breast. The skin of the breast may also appear pink, reddish purple, or bruised. In addition, the skin may have ridges or appear pitted, like the skin of an orange . These symptoms are caused by the buildup of fluid in the skin of the breast. This fluid buildup occurs because cancer cells have blocked lymph vessels in the skin, preventing the normal flow of lymph through the tissue. Sometimes the breast may contain a solid tumor that can be felt during a physical exam, but more often a tumor cannot be felt.
Other symptoms of inflammatory breast cancer include a rapid increase in breast size sensations of heaviness, burning, or tenderness in the breast or a nipple that is inverted . Swollen lymph nodes may also be present under the arm, near the collarbone, or both.
It is important to note that these symptoms may also be signs of other diseases or conditions, such as an infection, injury, or another type of breast cancer that is locally advanced. For this reason, women with inflammatory breast cancer often have a delayed diagnosis of their disease.
Recommended Reading: Scc Cancer Stages
Basal Cell Breast Cancer
Basal cell breast cancer is a type of breast cancer with a clear pattern of changes in proteins in the cells.
Cancer doctors recognise basal cell breast cancer when they examine the cancer cells under a microscope. It is often linked with triple negative breast cancer.
Basal cell breast cancers are usually triple negative. And most triple negative breast cancers are basal cell cancers. They are similar types of breast cancer, but not exactly the same.
See also
The symptoms of triple negative breast cancer are the same as for other breast cancer types.
See also
Idc Type: Tubular Carcinoma Of The Breast
Tubular carcinoma of the breast is a subtype of invasive ductal carcinoma . Tubular carcinomas are usually small and made up of tube-shaped structures called “tubules.” These tumors tend to be low-grade, meaning that their cells look somewhat similar to normal, healthy cells and tend to grow slowly.
At one time, tubular carcinomas accounted for about 1-4% of all breast cancers. Now that screening mammography is widely used, however, tubular carcinomas are being diagnosed more frequently often before you or your doctor would be able to feel a lump. Exact numbers aren’t available, but studies suggest that tubular carcinomas may account for anywhere from just under 8% to 27% of all breast cancers.
Studies also suggest that the average age of diagnosis for tubular carcinoma is the early 50s, although women can be diagnosed with it at any age. This type of cancer is rare in men.
Even though tubular carcinoma is an invasive breast cancer, it tends to be a less aggressive type that responds well to treatment. It isn’t likely to spread outside the breast and is considered to have a very good prognosis.
On the following pages, you can learn more about:
You May Like: Melanoma Stage 3 Symptoms
What Increases The Risk Of Invasive Breast Cancer
Thereâs no way to know if youâll develop an invasive form of breast cancer, but there are things that increase your chances, many of which you canât change.
Older women are at higher risk. About 10% of women diagnosed with invasive breast cancer are under age 45. And 2 out of every 3 women with invasive breast cancer are age 55 or older when theyâre first diagnosed.
Your genetics and family history of breast cancer play roles. Itâs more common among white women than black, Asian, or Hispanic women.
Also, youâre at higher risk if youâre obese, your breasts are dense, you didnât have children, or you became pregnant after the age of 35.
Staging And Treatment Of Microinvasive Breast Cancer : Is Axillary Lymph Node Investigation Necessary
Staging of microinvasive ductal carcinoma in situ is somewhat of a controversial topic. The general consensus surrounding pure ductal carcinoma in situ is that axillary lymph node metastasis is so very improbable that lymph node staging or sentinel lymph node biopsy are not necessary.
The overall estimated rate of lymph node metastases in patients with microinvasive breast carcinoma is low, but not negligible. The statistics also tend to be quite inconsistent, adding to the dilemma. Some studies on lymph node metastasis of microinvasive DCIS place the rate from 0 to just over 5%. Other studies suggest a rate of lymph node metastasis as high as 10%-11%, while others place it as high as 28%.
Also Check: Stage Iii Melanoma Prognosis