Management Of The Neck
Surgery is the mainstay of treatment for cervical lymph node metastases, which are grouped into five levels .2). With clinical evidence of nodal disease it is clear that the neck requires treatment, traditionally in the form of a neck dissection. Surgery has moved away from radical neck dissections towards modified and selective neck dissections . This preserves function, especially in relation to the accessory nerve, which if sacrificed usually gives rise to a stiff and painful shoulder. If clinical evidence of the presence of enlarged cervical nodes is lacking, but the expected incidence of node metastases is greater than 20%, it is common practice to treat the neck . The incidence of involved cervical lymph nodes for different sites and stages of tumour is known from retrospective studies.w2 Watching and waiting, to see if a node appears, is also practised, and no prospective randomised trials compare the two approaches. Prophylactic treatment of the neck may reduce the rate of systemic metastatic disease.
Factors That Could Affect Your Prognosis
Certain aspects of your health or cancer could affect your outlook. For example, people who have a weakened immune system from a disease like HIV or a medication they take tend to have a less positive outlook.
The location of the tumor also matters. Cancers on the face, scalp, fingers, and toes are more likely to spread and return than those on other parts of the body. SCC that starts in an open wound is also more likely to spread.
Larger tumors or ones that have grown deep in the skin have a higher risk of growing or returning. If a cancer does recur after treatment, the prognosis is less positive than it was the first time around.
Ask your doctor if you have any risk factors that can be managed or controlled. You may need more aggressive treatment, or to be monitored more closely for recurrence.
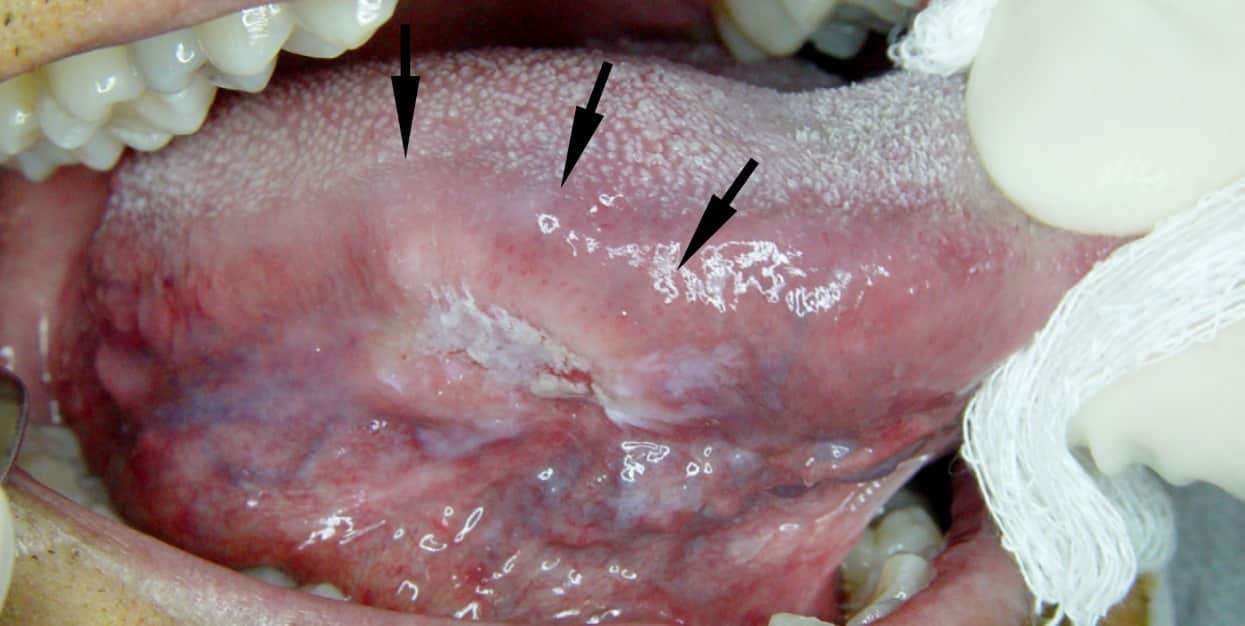
Diagnosing Squamous Cell Carcinoma
The main way to diagnose squamous cell carcinoma is with a biopsy. This involves having a small piece of tissue removed from the suspicious area and examined in a laboratory.
In the laboratory, a pathologist will examine the tissue under a microscope to determine if it is a skin cancer. He or she will also stage the cancer by the number of abnormal cells, their thickness, and the depth of penetration into the skin. The higher the stage of the tumor, the greater the chance it could spread to other parts of the body.
Squamous cell carcinoma on sun-exposed areas of skin usually does not spread. However, squamous cell carcinoma of the lip, vulva, and penis are more likely to spread. Contact your doctor about any sore in these areas that does not go away after several weeks.
Don’t Miss: Ductal Invasive Carcinoma Survival Rate
What Is A 5
A relative survival rate compares women with the same type and stage of vulvar cancer to people in the overall population. For example, if the 5-year relative survival rate for a specific stage of vulvar cancer is 90%, it means that women who have that cancer are, on average, about 90% as likely as women who dont have that cancer to live for at least 5 years after being diagnosed.
Stage 0 Squamous Cell Carcinoma
This is a very early stage that may or may not develop into SCC depending on whether it is caught in time and treated. This is considered a pre-malignant or pre-cancerous stage and is also known as carcinoma in situ or Bowens disease. It is at this point only present in the upper layer of the skin known as the epidermis and is yet to penetrate to lower layers and spread to deeper areas. Cells have begun to turn cancerous but have not yet spread and affected surrounding areas.6
You May Like: What Is Braf Testing In Melanoma
What Are Stage 4 Cervical Cancer Treatments
Because stage 4 cervical cancer is advanced, the are more aggressive. However, if you decide that you do not want to undergo the above treatments, there are options for to improve your quality of life. These options include:
- Chemoradiation
- For stage 4A cervical cancer, both chemotherapy and radiation are given. The chemotherapy drug or drugs are delivered every 4 weeks to make radiation therapy more effective. Brachytherapy can also supplement the EBRT.
What Is Stage 3 Cervical Cancer
Stage 3 cervical cancer is when cancer has spread to the lower part of the vagina or the pelvic walls. With stage 3 cervical cancer, tumors may block the ureters . Stage 3 cervical cancer has:
- Spread to the lower part of the vagina or pelvic walls
- May have spread to lymph nodes
- Not spread to distant sites
Stage 3 is split into A, B and C. Cancer has spread to:
- 3A: The lower part of the vagina but not the pelvic walls
- 3B: The walls of the pelvis and is blocking 1 or both ureters
- 3C: Nearby pelvic or para-aortic lymph nodes – the tumor can be any size
Recommended Reading: Melanoma Bone Cancer Symptoms
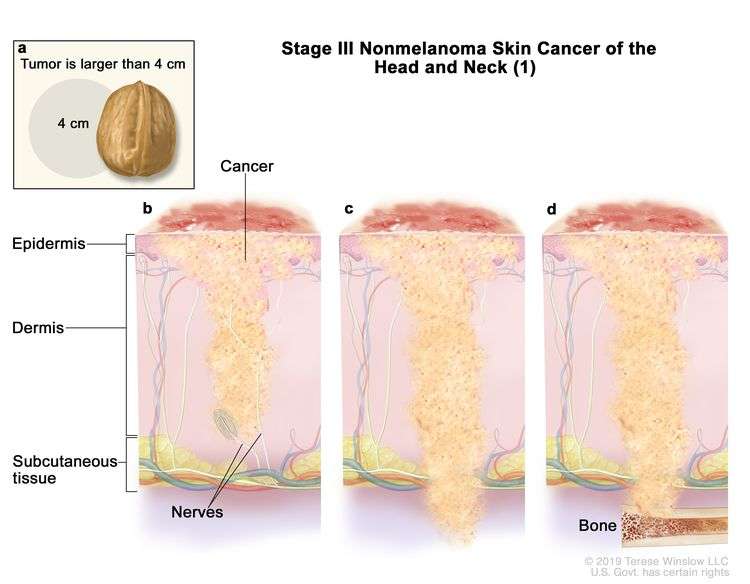
Stage Iii Squamous Cell Carcinoma
The tumor cells may be of any size at the original site. A stage III SCC has begun to invade the nearby lymph nodes on the side of the body of the original cancerous growth. This new growth is still under 3 cm in size. It may also have grown into the facial bones like the bones surrounding the eye or your jaw bone.9 It has not affected any other organs.10
Treating Squamous Cell Carcinoma
Most of squamous cell carcinomas can be cured if they are treated early. Once squamous cell carcinoma has spread beyond the skin, though, less than half of people live five years, even with aggressive treatment.
There are many ways to treat squamous cell carcinoma that has not spread. These include:
- cutting away the cancer and a small amount of healthy tissue around it. If a large area of skin is removed, a skin graft may be necessary.
- scraping away the cancer with a surgical tool. An electric probe is used to kill any cancerous cells left behind.
- freezing cancer cells with liquid nitrogen. This treatment is usually used only for very small tumors or for a patch of skin that looks abnormal but isn’t yet cancerous.
- destroying the tumor with radiation.
- shaving away the cancer, one thin layer at a time. Each layer is examined under the microscope as it is removed. This technique helps the doctor preserve as much healthy skin as possible.
- applying drugs directly to the skin or injecting them into the tumor
- using a narrow laser beam to destroy the cancer.
The treatment that is best for you depends on the size and location of the cancer, whether it has returned after previous treatment, your age, and your general health.
Once your treatment is finished, it’s important to have regular follow-up skin exams. Your doctor may want to see you every three months for the first year, for example, and then less often after that.
Recommended Reading: Stage 2 Invasive Ductal Carcinoma Survival Rate
Tests That Examine The Tissues Of The Neck Respiratory Tract And Upper Part Of The Digestive Tract Are Used To Detect And Diagnose Metastatic Squamous Neck Cancer And The Primary Tumor
Tests will include checking for a primary tumor in the organs and tissues of the respiratory tract , the upper part of the digestive tract , and the genitourinary system.
The following procedures may be used:
- Physical exam and health history: An exam of the body, especially the head and neck, to check general signs of health. This includes checking for signs of disease, such as lumps or anything else that seems unusual. A history of the patients health habits and past illnesses and treatments will also be taken.
- Biopsy: The removal of cells or tissues so they can be viewed under a microscope by a pathologist or tested in the laboratory to check for signs of cancer.
Three types of biopsy may be done:
- Fine-needle aspiration biopsy: The removal of tissue or fluid using a thin needle.
- Core needle biopsy: The removal of tissue using a wide needle.
- Excisional biopsy: The removal of an entire lump of tissue.
The following procedures are used to remove samples of cells or tissue:
One or more of the following laboratory tests may be done to study the tissue samples:
What Are Stage 1 Cervical Cancer Treatments
The treatments for stage 1 cervical cancer vary for women depending on whether they want to be able to have children in the future or not.
For those who wish to maintain fertility, the initial treatments are:
- Cone biopsy: Removing a cone-shaped piece of tissue from the cervix. Whether it warrants additional treatment depends on the results of the biopsy.
- If the cones edge has negative margins, that means the edges do not contain cancer cells, and the surgery removed it all. You will need to be monitored to ensure the cancer doesnt return, but no more treatment is required.
- If the edges of the cone have positive margins , cancer may be left behind, which will require 1 of 2 treatments:
- Repeat cone biopsy
- Radical trachelectomy
- This procedure involves removing the cervix, upper vagina and tissue surrounding the cervix.
- Becoming pregnant after this surgery may be more difficult, and some women experience fertility issues. However, there are options to preserve fertility.
- The pregnancy following a trachelectomy will result in a cesarean section for the birth of the baby.
For those who are done having children, the options are different:
Don’t Miss: Malignant Breast Cancer Survival Rate
Altered Radiation Fractionation Schedules
Conventional radiotherapy consists of one daily treatment Monday to Friday for three to seven weeks, varying between centres in the United Kingdom. Total doses vary from 50 Gy to 70 Gy. In the United States and Europe 60 Gy to 70 Gy are standard. These schedules are assumed to have the same overall radiobiological effect, which depends on the relation between overall time, total dose, and the number of fractions. They developed through clinical experience and training, however, randomised controlled trials have never been used to compare these different conventional fractionation schedules.
In the 1980s focus centred on time-fractionation schedules low doses per fraction could give reduced late morbidity. This led to trials of hyperfractionation in which the dose per fraction was smallthat is, divided up into two or three treatments per day instead of one. With increasing overall treatment time the total dose had to be increased to achieve the same effect. Accelerated regimens with shortened overall duration were therefore investigated, with the aim of reducing the time in which tumour cell repopulation could occur. These regimens have been studied by groups at Mount Vernon, United Kingdom, the Danish head and neck cancer group, radiation therapy, and oncology group in the United States, the European Organization for Research and Treatment of Cancer, and others with improvements in disease specific survival and locoregional control .
Pursue Compensation For Your Illness
Pintas & Mullins Law Firm may be able to help you seek financial compensation for your illness if you have been diagnosed with lung cancer and believe it may be due to asbestos or radon exposure. We have represented clients across the United States in personal injury cases since 1985.
We can investigate the cause of your cancer and may be able to pursue a settlement on your behalf with the liable partys insurance company. If you were exposed to asbestos and the business responsible has declared bankruptcy, we may be able to obtain an award from a trust fund that was set up to compensate victims. We can also fight to get you fair compensation in a trial, if necessary.
Our firm works on a contingency basis, so you will not have to pay upfront fees. We will only receive a fee if we secure compensation for you. Call our office at to discuss your case with a member of our staff.
Symptoms are often crucial to the early detection and treatment of any disease. Unfortunately, lung cancer does not always exhibit signs until it is already in the advanced stages. Even when symptoms are present, doctors can dismiss them as indicators of a less severe respiratory infection. This means most people will not realize that they …
Also Check: Basal Cell Carcinoma Late Stages
Basal Cell Carcinoma Stages
There are certain features that are considered to make the cancer at higher risk for spreading or recurrence, and these may also be used to stage basal cell carcinomas. These include:
- Greater than 2 mm in thickness
- Invasion into the lower dermis or subcutis layers of the skin
- Invasion into the tiny nerves in the skin
- Location on the ear or on a hair-bearing lip
After the TNM components and risk factors have been established, the cancer is given a stage. For basal cell carcinoma staging, the factors are grouped and labeled 0 to 4. The characteristics and stages of basal cell carcinoma are:
Stage 0: Also called carcinoma in situ, cancer discovered in this stage is only present in the epidermis and has not spread deeper to the dermis.
Stage 1 basal cell carcinoma: The cancer is less than 2 centimeters, about 4/5 of an inch across, has not spread to nearby lymph nodes or organs, and has one or fewer high-risk features.
Stage 2 basal cell carcinoma: The cancer is larger than 2 centimeters across, and has not spread to nearby organs or lymph nodes, or a tumor of any size with 2 or more high-risk features.
Stage 3 basal cell carcinoma: The cancer has spread into facial bones or 1 nearby lymph node, but not to other organs.
Stage 4 basal cell carcinoma: The cancer can be any size and has spread to 1 or more lymph nodes which are larger than 3 cm and may have spread to bones or other organs in the body.
What Are The Stages Of Squamous Cell Carcinoma
After evaluating these factors, the oncologist will assign one of the following squamous cell carcinoma stages to the tumor: 1 Stage 0 Cancer is only present on the epidermis . 2 Stage 1 Cancer has grown deep into the skin, but has not spread to nearby lymph nodes 3 Stage 2 Cancer has grown deep into
There is no standard staging system for metastatic squamous neck cancer with occult primary. The tumors are described as untreated or recurrent. Untreated metastatic squamous neck cancer with occult primary is cancer that is newly diagnosed and has not been treated, except to relieve signs and symptoms caused by the cancer.
Also Check: Can You Die From Basal Cell Skin Cancer
Combined Radiotherapy And Chemotherapy
With this treatment, you have daily external radiotherapy for 5 days every week, for around 5 weeks. You also have a boost of internal radiotherapy at the end of your course.
During your course of radiotherapy, you also have chemotherapy once a week or once every 2 or 3 weeks. This depends on the chemotherapy drugs you have.
-
Cancer: Principles and Practice of Oncology VT DeVita , TS Lawrence, SA RosenbergWolters Kluwer, 2019
-
Cancer and its Management J Tobias and D HochhauserWiley-Blackwell, 2015
-
Cervical cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow upC Marth and others Annals of Oncology, 2017. Volume 28, Supplement 4
-
2018 FIGO Staging System for Cervical cancer: Summary and comparison with 2009 FIGOStaging System
Treating Squamous Cell Carcinoma Of The Skin
Treatment options for squamous cell skin cancer depend on the risk of the cancer coming back, which is based on factors like the size and location of the tumor and how the cancer cells look under a microscope, as well as if a person has a weakened immune system.
Most squamous cell skin cancers are found and treated at an early stage, when they can be removed or destroyed with local treatment methods. Small squamous cell cancers can usually be cured with these treatments. Larger squamous cell cancers are harder to treat, and fast-growing cancers have a higher risk of coming back.
In rare cases, squamous cell cancers can spread to lymph nodes or distant parts of the body. If this happens, treatments such as radiation therapy, immunotherapy, and/or chemotherapy may be needed.
You May Like: Tumor Calcification
Squamous Cell Carcinoma Stages
There are certain features that are considered to make the cancer at higher risk for spreading or recurrence, and these may also be used to stage squamous cell carcinomas. These include:
- Greater than 2 mm in thickness
- Invasion into the lower dermis or subcutis layers of the skin
- Invasion into the tiny nerves in the skin
- Location on the ear or on a hair-bearing lip
After the TNM components and risk factors have been established, the cancer is assigned to one of the five squamous cell carcinoma stages, which are labeled 0 to 4. The characteristics and stages of squamous cell cancer are:
Stage 0: Also called carcinoma in situ, cancer discovered in this stage is only present in the epidermis and has not spread deeper to the dermis.
Stage 1 squamous cell carcinoma: The cancer is less than 2 centimeters, about 4/5 of an inch across, has not spread to nearby lymph nodes or organs, and has one or fewer high-risk features.
Stage 2 squamous cell carcinoma: The cancer is larger than 2 centimeters across, and has not spread to nearby organs or lymph nodes, or a tumor of any size with 2 or more high risk features.
Stage 3 squamous cell carcinoma: The cancer has spread into facial bones or 1 nearby lymph node, but not to other organs.
Stage 4 squamous cell carcinoma: The cancer can be any size and has spread to 1 or more lymph nodes which are larger than 3 cm and may have spread to bones or other organs in the body.