How Is Melanoma Of The Head And Neck Diagnosed
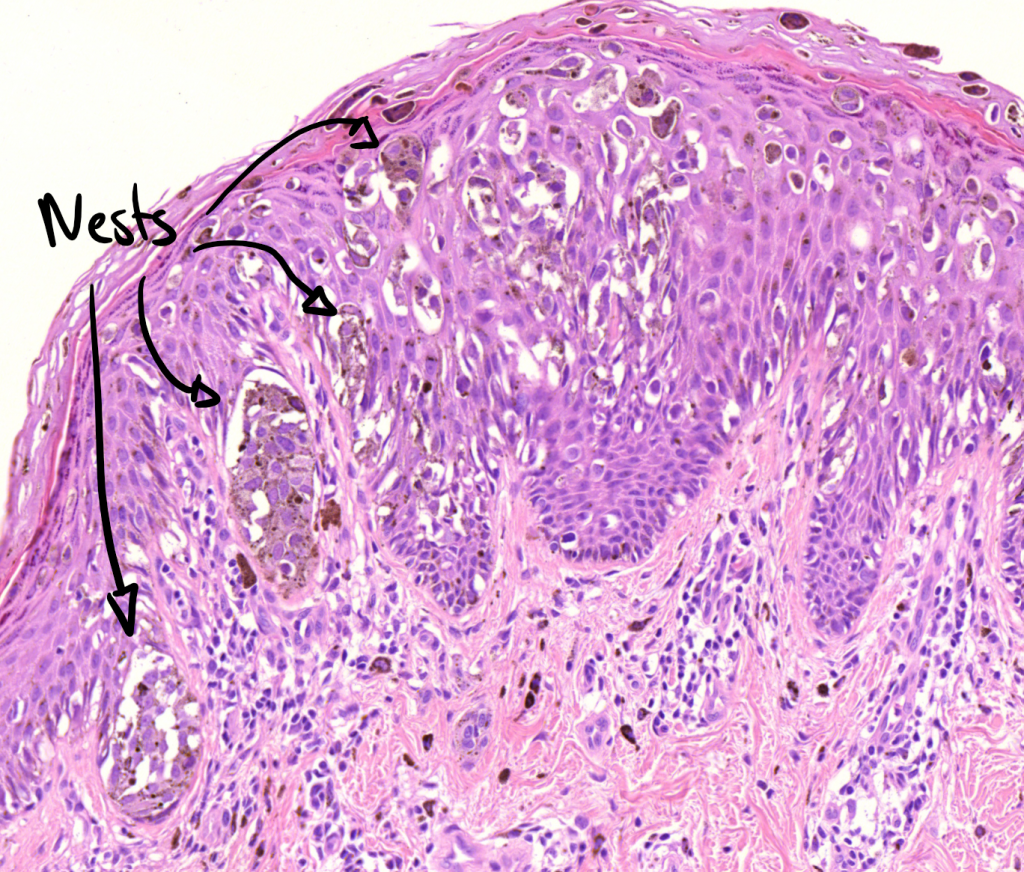
Diagnosis is made by clinical exam and a biopsy. Melanoma is diagnosed by the presence of abnormal melanocytes.
Melanoma of the skin is staged based on how deeply it invades the skin layers and whether or not it has spread. A superficial or shave biopsy will not provide the accurate staging information used to guide treatment. The depth of invasion determines the risk of spread to lymph nodes or other organs. Ulceration and microsatellitosis are additional diagnostic features that, when present, are associated with a higher risk of spread. In patients without clinically enlarged lymph nodes, sentinel lymph node biopsy is used to determine if microscopic spread to lymph nodes in the neck has occurred, and is used for all but very thin melanomas unless other high-risk features are present.
This information is used for staging, to guide prognosis and further treatment. Thick melanomas are associated with a higher risk of spread to other organs, which is evaluated by pretreatment imaging. When enlarged lymph nodes are detected on clinical exam, a fine needle aspiration biopsy is performed to determine whether melanoma is present in nodes.
Some subtypes of melanoma may be less likely to spread: lentigo maligna and desmoplastic melanoma. The role of sentinel node biopsy is controversial in these cases, and will be discussed with you by your treatment team.
Squamous Cell Carcinoma Stages
There are certain features that are considered to make the cancer at higher risk for spreading or recurrence, and these may also be used to stage squamous cell carcinomas. These include:
- Greater than 2 mm in thickness
- Invasion into the lower dermis or subcutis layers of the skin
- Invasion into the tiny nerves in the skin
- Location on the ear or on a hair-bearing lip
After the TNM components and risk factors have been established, the cancer is assigned to one of the five squamous cell carcinoma stages, which are labeled 0 to 4. The characteristics and stages of squamous cell cancer are:
Stage 0: Also called carcinoma in situ, cancer discovered in this stage is only present in the epidermis and has not spread deeper to the dermis.
Stage 1 squamous cell carcinoma: The cancer is less than 2 centimeters, about 4/5 of an inch across, has not spread to nearby lymph nodes or organs, and has one or fewer high-risk features.
Stage 2 squamous cell carcinoma: The cancer is larger than 2 centimeters across, and has not spread to nearby organs or lymph nodes, or a tumor of any size with 2 or more high risk features.
Stage 3 squamous cell carcinoma: The cancer has spread into facial bones or 1 nearby lymph node, but not to other organs.
Stage 4 squamous cell carcinoma: The cancer can be any size and has spread to 1 or more lymph nodes which are larger than 3 cm and may have spread to bones or other organs in the body.
Risk Factors For Metastatic Melanomas
You cannot get metastatic melanoma without first having melanoma, though the primary melanoma may be so small its undetectable. Major risk factors for melanomas include:
- Light skin, light-colored hair or light-colored eyes
- Skin prone to burning easily
- Multiple blistering sunburns as a child
- Family history of melanoma
- Frequent exposure to sun or ultraviolet radiation
- Certain genetic mutations
- Exposure to environmental factors, such as radiation or vinyl chloride
Other factors have been connected with increased metastasis. In a 2018 study in the Anais Brasileiros de Dermatologia and a 2019 study in the Journal of the National Cancer Institute, the following factors were associated with higher levels of metastasis:
- Male gender
- Primary tumor thickness of more than 4 mm
- Nodular melanoma, which is a specific subtype that a care team would identify
- Ulceration of the primary tumor
Also Check: Prognosis Of Skin Cancer
Recognizing The Signs And Symptoms
The most noticeable sign of melanoma is the appearance of a new mole or a change in an existing mole or birthmark. People should be aware of any pigmented areas on the skin that appear abnormal in color, shape, size, or texture.
People with stage 4 melanoma may also have ulcerated skin , which is skin with tiny breaks on the surface. These ulcerations can bleed.
Another sign is swollen or hard lymph nodes, which a doctor can confirm by carrying out a physical examination. Other tests include blood tests and imaging scans to confirm the presence of cancer and check how much it has spread.
How Is Melanoma Diagnosed
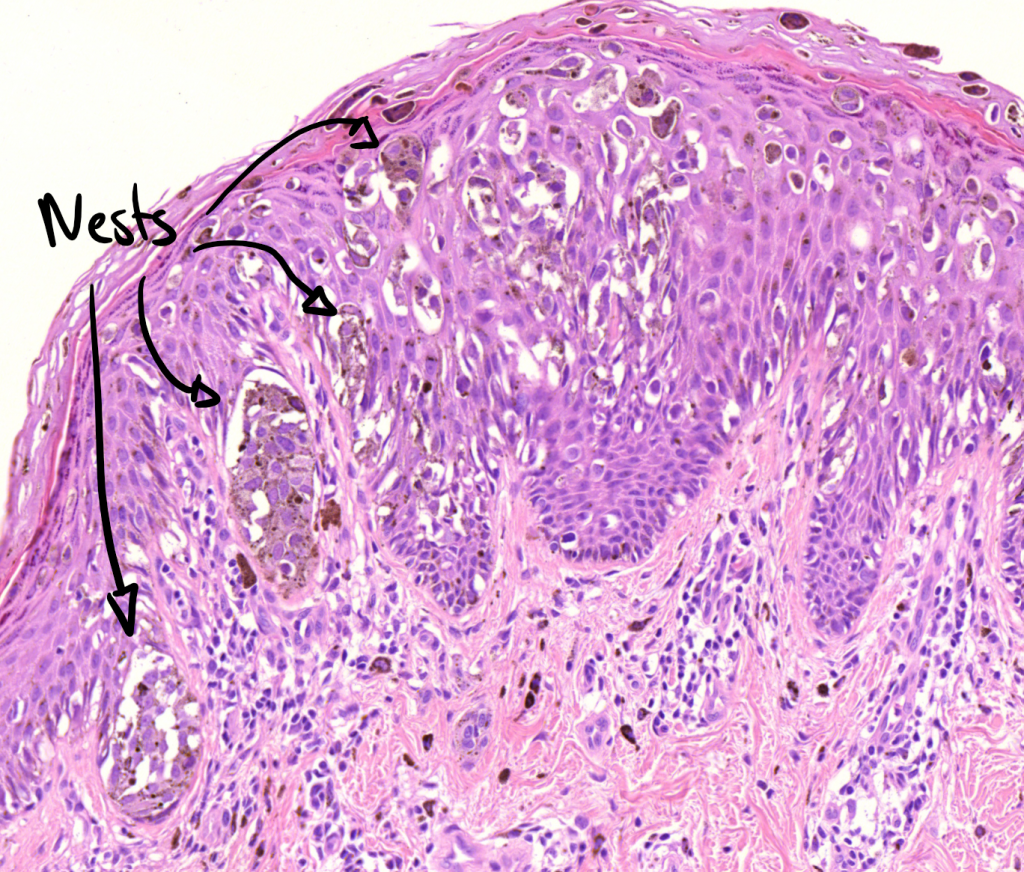
If you have a mole or other spot that looks suspicious, your doctor may remove it and look at it under the microscope to see if it contains cancer cells. This is called a biopsy.
After your doctor receives the skin biopsy results showing evidence of melanoma cells, the next step is to determine if the melanoma has spread. This is called staging. Once diagnosed, melanoma will be categorized based on several factors, such as how deeply it has spread and its appearance under the microscope. Tumor thickness is the most important characteristic in predicting outcomes.
Melanomas are grouped into the following stages:
- Stage 0 : The melanoma is only in the top layer of skin .
- Stage I: Low-risk primary melanoma with no evidence of spread. This stage is generally curable with surgery.
- Stage II: Features are present that indicate higher risk of recurrence, but there is no evidence of spread.
- Stage III: The melanoma has spread to nearby lymph nodes or nearby skin.
- Stage IV: The melanoma has spread to more distant lymph nodes or skin or has spread to internal organs.
Don’t Miss: Carcinoma Cancer Symptoms
What They Look Like
Melanomas in situ tend to be flat and asymmetric with irregular borders. They can be black, brown, tan, gray or even pink if the person has very fair skin. Areas that receive the greatest sun exposure, such as the scalp, face and neck, are more likely to develop melanoma in situ than the arms or legs. However, non-sun exposed areas, such as the buttocks, are also at risk. We dont always understand the causes of these melanomas, though heredity can play a role. To detect melanoma in situ as early as possible, it helps to monitor your own skin. Head-to-toe self-examinations are a good place to start, including the areas where the sun doesnt shine. When evaluating your skin, focus on the ABCDEs of melanoma detection. A stands for asymmetry B for irregular borders C for more than one color D for diameter greater than 6mm , or the size of a pencil eraser and E for evolving, meaning any lesion that is new or changing. View helpful photos showing the ABCDEs of melanoma.
What Kind Of Treatment Will I Need
There are many ways to treat melanoma. The main types of treatment are:
- Surgery
Most early stage melanomas can be treated with surgery alone. More advanced cancers need other treatments.
The treatment plan thats best for you will depend on:
- The stage of the cancer
- The results of lab tests on the cancer cells
- The chance that a type of treatment will cure the melanoma or help in some way
- Your age
- Other health problems you have
- Your feelings about the treatment and the side effects that come with it
You May Like: Melanoma Braf Positive
How Do Doctors Determine The Staging And Prognosis Of A Melanoma
The most useful criterion for determining prognosis is tumor thickness. Tumor thickness is measured in fractions of millimeters and is called the Breslow’s depth. The thinner the melanoma, the better the prognosis. Any spread to lymph nodes or other body locations dramatically worsens the prognosis. Thin melanomas, those measuring less than 0.75 millimeters when examined microscopically, have excellent cure rates, generally with local surgery alone. For thicker melanomas, the prognosis is guarded.
Melanoma is staged according to thickness, ulceration, lymph node involvement, and the presence of distant metastasis. The staging of a cancer refers to the extent to which it has spread at the time of diagnosis, and staging is used to determine the appropriate treatment. Stages 1 and 2 are confined to the skin only and are treated with surgical removal with the size of margins of normal skin to be removed determined by the thickness of the melanoma. Stage 3 refers to a melanoma that has spread locally or through the usual lymphatic drainage. Stage 4 refers to distant metastases to other organs, generally by spread through the bloodstream.
Can Metastasis Be Prevented
Melanoma can spread “silently,” meaning that you may not experience any symptoms of metastasis. Therefore, if you’ve been treated for early-stage melanoma in the past, it is extremely important to perform regular self-examinations of your skin and lymph nodes, to keep all your appointments for checkups, and practice sun safety. There is nothing else an individual can do to prevent metastasis from being very diligent.
Catching a recurrence early greatly increases your chances of successful treatment. If the melanoma does spread, it is important to remain positive: remember that while the average prognosis is poor, some people do survive stage IV melanoma.
Skin Cancer Doctor Discussion Guide
Get our printable guide for your next doctor’s appointment to help you ask the right questions.
Recommended Reading: Can You Get Cancer In The Back Of Your Neck
Factors Used For Staging Melanoma
To determine the stage of a melanoma, the lesion and some surrounding healthy tissue need to be surgically removed and analyzed using a microscope. Doctors use the melanomas thickness, measured in millimeters , and the other characteristics described in Diagnosis to help determine the diseases stage.
Doctors also use results from diagnostic tests to answer these questions about the stage of melanoma:
-
How thick or deep is the original melanoma, often called the primary melanoma or primary tumor?
-
Where is the melanoma located?
-
Has the melanoma spread to the lymph nodes? If so, where and how many?
-
Has the melanoma metastasized to other parts of the body? If so, where and how much?
The results are combined to determine the stage of melanoma for each person. The stages of melanoma include: stage 0 and stages I through IV . The stage provides a common way of describing the cancer, so doctors can work together to create the best treatment plan and understand a patient’s prognosis.
What Does A Normal Vs An Abnormal Mole Look Like
Normal moles are usually round or oval and smaller than a pencil eraser. They are one consistent color , with a clear border. Most people have less than 50 moles. You can be born with moles, develop them with age or even have some disappear.
Cancerous, or malignant, moles may vary greatly in appearance. To help identify moles that might indicate melanoma, think of the letters A-B-C-D-E:
- A | Asymmetry: Mole is an irregular shape, such as if one side looks different than the other
- B | Border: Mole has irregular, ragged, notched or scalloped borders
- C | Color: Mole has more than one color or uneven shading
- D | Diameter: Mole is bigger than a pencil eraser
- E | Evolution: Mole changes in some way
Talk to your doctor, if you notice any skin changes that seem unusual.
Don’t Miss: Stage 3 Invasive Ductal Carcinoma Survival Rate
Red Flag #: Unexplained Weight Loss And Loss Of Appetite
Unintentional weight loss is a common side effect of any cancer. When it comes to melanoma, extreme weight loss usually only happens after the cancer has spread from the skin to other parts of the body. Dr. Zaba says she can sometimes tell if a patients melanoma has metastasized because it looks like they have cachexia, a syndrome marked by drastic loss of fat and muscle and increased weakness. Cachexia can also cause loss of appetite, which further contributes to the problem.
What Symptoms Develop When Melanoma Spreads To The Brain
Many patients feel the same. They dont have any symptoms that would indicate the cancer has spread.
If your doctor thinks that you are at risk for melanoma spreading to your brain, you may need an MRI. An MRI can find cancer in the brain before you have symptoms. Not everyone who has melanoma needs to have an MRI.
When melanoma spreads to the brain and symptoms occur, they may include:
-
Headaches
-
Paralysis on one side of your body
-
Problems with your eyesight
Symptoms tends to occur when the cancer has spread to more than one area of the brain. A large tumor can also cause symptoms.
Also Check: Tumor Calcification
Causes And Risk Factors For Metastatic Melanoma
Everyone of every age, sex, race, and ethnicity faces some level of risk when it comes to melanoma, including the metastatic kind, but certain factors raise the odds. These include:
Ultraviolet Light Exposure Whether it comes from the sun or from tanning beds, UV light is a very significant risk factor for melanoma. UV light damages the genes in melanocytes that control their growth. These genetic mutations direct the cells to multiply with abnormal speed, forming tumors. Blistering sunburns in early childhood are especially dangerous.
Moles Certain kinds of atypical moles known as dysplastic nevi, which can be larger than regular moles and an abnormal shape or color, raise melanoma risk. People with an inherited condition called dysplastic nevus syndrome, which causes them to have many dysplastic nevi, are at very high risk. Congenital melanocytic nevi moles present at birth, especially very large ones are another risk factor.
Fair Skin, Freckling, and Light Hair Caucasians with this kind of coloring are at higher risk than other racial groups.
Family History of Melanoma Around 10 percent of people with melanoma have a first-degree family member with the disease, such as a parent, sibling, or children.
Personal History of Melanoma or Other Skin Cancers Having had melanoma raises the risk of getting it again. Having another type of skin cancer, such as basal or squamous cell skin cancer, is also a risk factor.
How Does The Doctor Know I Have Melanoma
A new spot on your skin or a spot thats changing in size, shape, or color may be a warning sign of melanoma. If you have any of these changes, have your skin checked by a doctor.
The doctor will ask you questions about when the spot on your skin first showed up and if it has changed in size or the way it looks. The rest of your skin will be checked. During the exam your doctor will check the size, shape, color and texture of any skin changes. If signs are pointing to melanoma, more tests will be done.
Also Check: What Is Braf Melanoma
Red Flag #: Abdominal Pain And Tenderness
Early on, there may be no noticeable symptoms that melanoma has spread to the liver. When symptoms do show up, they commonly include an enlarged, hard, or tender liver and pain in the upper right area of your abdomen, just below your ribs. Other signs cancer has spread to the liver are similar to symptoms of liver disease: fluid buildup in the belly and yellowing of the skin and eyes .
Tests That May Be Done
The doctor will ask you questions about when the spot on your skin first showed up and if it has changed in size or the way it looks or feels. The rest of your skin will be checked. During the exam your doctor will check the size, shape, color and texture of any skin changes. If signs are pointing to skin cancer, more tests will be done.
Skin biopsy
In a biopsy, the doctor takes out a small piece of tissue to check it for cancer cells. A biopsy is the only way to tell for sure if you have skin cancer and what kind it is.
There are many types of skin biopsies. Ask your doctor what kind you will need. Each type has pros and cons. The choice of which type to use depends on your own case.
In rare cases basal and squamous cell skin cancer can spread to the nearby lymph nodes Ask your doctor if your lymph nodes will be tested.
Basal and squamous cell cancers don’t often spread to other parts of the body. But if your doctor thinks your skin cancer might spread, you might need imaging tests, such as MRI or CT scans.
Read Also: How Long Until Melanoma Spreads
Melanoma Of The Head And Neck Treatment
Surgical resection with wide margins and often sentinel lymph node biopsy is required for melanoma that has not spread. Thin tumors, up to 1 millimeter thick, can be resected with 1-centimeter margins around the tumor. The greater the depth of invasion, the larger the margin required, up to 2 centimeters. Mohs surgery is not suitable for melanoma because the diagnosis often requires special pathologic staining that is not part of the Mohs technique.
To obtain a sentinel lymph node biopsy, a preoperative sentinel node localization study is performed: A radionuclide tracer is injected in the melanoma, then a radionuclide uptake SPECT or SPECT-CT scan shows which nodes the tracer spreads to first. These sentinel nodes may or may not contain melanoma: They are the nodes that a melanoma that has spread would first encounter, and contain melanoma cells when melanoma has spread to lymph nodes. Because there are hundreds of lymph nodes in the head and neck, your surgeon will use a gamma probe at surgery to identify and confirm that the nodes selected for removal are the sentinel nodes.
When enlarged lymph nodes are present, a neck dissection is performed at the time of surgery. If distant spread is detected during the workup that is, melanoma has spread to other organs immunotherapy and sometimes radiation therapy are used for treatment.
Johns Hopkins Head and Neck Cancer Surgery
What Is Metastatic Melanoma
Melanoma is a type of skin cancer. When it spreads to other places in your body, it’s called metastatic, or advanced. You may also hear your doctor refer to it as stage IV melanoma.
Melanoma often spreads to:
Although in many cases metastatic melanoma canât be cured, treatments and support can help you live longer and better. Doctors have therapies that have greatly increased survival rates. And researchers are working to find new medications that can do even more.
Remember: You still have control over the decisions you make about your treatment and your life. It’s important to have people you can talk to about your plans, your fears, and your feelings. So find support and learn about your treatment options. That will help you make the most of your life.
Also Check: Rare Cancer Symptoms