What Is Urothelial Carcinoma
Urothelial Carcinoma is a multifocal malignancy associated with the reno-urinary system. Renal parenchyma often develops a high-grade scirrhous mass formation and turns to a malignant tumor. In urothelial carcinoma, the organ which can get affected with malignant attacks is renal pelvis, ureters, and bladder. The possibility of this organ get affected with Urothelial Carcinoma can be estimated as 1:3:50 respectively.
It has been observed that upper urinary tract cancer affected patients have a 30 to 50 percent tendency to develop bladder cancer, whereas bladder cancer affected individuals also has a 2 to 3 percent tendency to develop urinary tract cancer. Therefore, the reno-urinary system is interconnected and the scope of cancer progression also inter-related1,2.
Risk Groups For Early Bladder Cancer
Doctors put early bladder cancer into 3 risk groups. These groups describe how likely it is that your cancer will spread further, or come back after treatment.
The 3 risk groups are:
- low risk
- intermediate risk
- high risk
Your doctor tells you whether your cancer is low risk, intermediate risk or high risk. Knowing your risk group helps them decide which tests and treatment are best for you.
Your risk group depends on:
- the size of your tumour
- what the cells look like under a microscope
- how many tumours there are
- the type of bladder tumour
- whether you have had treatment in the last year for early bladder cancer
Irocker Cruiser Paddle Board
Newbie boarders with a spot of curiosity and magical journey in their spirit. Outfitted with an extra-wide 33 base, broad tail, as well as balance functions making this board the steadiest iSUP on the marketplace. With a 400lbs weight capability, its developed to manage any kind of rider.
Stand up with convenience and also try some on-board yoga sensation secure above water the perfect novice board to feed that daring side. A smooth introduction to paddleboarding that will certainly make you rely on yourself!
Read Also: Basal Skin Cancer Survival Rates
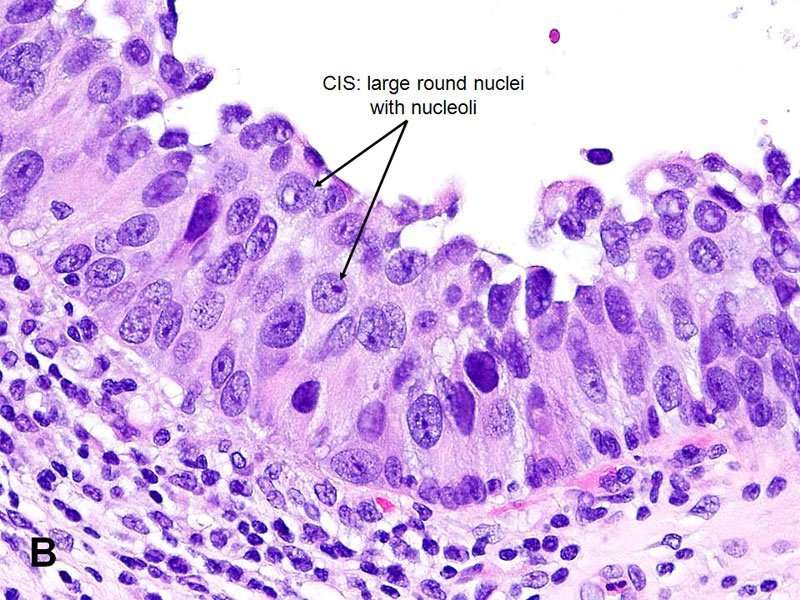
Meaning Of Carcinoma In Situ
In many ways, the term “carcinoma” is simply equated with cancer. Roughly 85 percent of cancers are carcinomas. Carcinomas are composed of epithelial cells the type of cells that line the skin, breast ducts, and other surfaces of organs in the body.
The subtypes of carcinomas include adenocarcinoma, squamous cell carcinoma, transitional cell carcinoma , and basal cell carcinoma.
Carcinoma in situ can be further defined by the tissue type in which cancer is beginning. For example, squamous cell carcinoma in situ of the cervix would represent a cancer that had started in squamous cells which line the cervix and has not yet become invasive.
Tumors such as sarcomas arise in tissues which do not have a basement membrane so that for these types of cancer there is not a stage of carcinoma in situ. In other words, tumors such as bone cancer do not have a pre-invasive stage and the cells would either be considered normal or cancer. Likewise, blood-related cancers, such as leukemias and lymphomas, do not have a preinvasive but cancerous stage for which people can be screened. For cancers that don’t have a CIS stage, screening tests are not as effective in early detection, because once the abnormal cells are detected, it would already be considered invasive with the potential to spread .
Intravesical Bcg Plus Ifn
Prior investigators have reported use of BCG and Interferon alpha therapy after BCG failure and have shown a 5060% complete response rate . In a subsequent large phase II trial on this combination therapy, 45% of patients with BCG failure and 59% of patients naïve to BCG remained disease free at a median of 24-month follow up . Unfavorable factors that were significant for recurrence after BCG and INF therapy included multifocality, large size , presence of T1, and prior BCG failure more than once .
However, combination therapy with INF should not be used as first-line therapy as it has not been shown to be effective. A multicenter, prospective study randomized 670 patients who were BCG naïve with NMIBC to receive BCG or BCG plus INF. At 24-month median follow up, there was no difference in recurrence-free survival between the two groups . There is also limited efficacy for CIS after two BCG failures and it is important to note that patients with significant unfavorable risk factors mentioned earlier are most difficult to deal with, as combination therapy with INF is the least effective.
Read Also: Metastatic Basal Cell Carcinoma Survival Rate
Carcinoma In Situ Vs Precancerous Cells Vs Dysplasia
There are many terms describing the spectrum of normal cells and invasive cancer cells. One of these is dysplasia. Dysplasia can run the spectrum from mild dysplasia in which the cells are barely abnormal appearing, to carcinoma in situ, which some pathologists describe as severe dysplasia involving the full thickness of the epithelium. The term precancerous cells may also be used to describe cells on this continuum between normal and cancer cells.
These terms are also used in different ways depending on the sample analyzed. For example, cells visualized on a pap smear may show dysplasia , but since the cells are “loose,” nothing can be said about whether carcinoma in situ is present or not. With cervical dysplasia, a biopsy is required before the diagnosis of CIS is made. A biopsy sample provides a view of the cells as they occur in relation to the basement membrane and other cells, and is needed to understand if abnormal cells seen on a pap smear are concerning.
Cystectomy Cystoprostatectomy And Pelvic Exenteration Specimens
Processing of these specimens may be summarized in three steps: orientation of the specimen and identification of relevant anatomic structures , fixation of the specimen and dissection of the specimen. Peritoneum covering the surface of the bladder is a reliable anatomic landmark. In both male and female patients, the peritoneum descends further along the posterior wall of the bladder than it does along the anterior wall. Other pelvic organs, if present, may also be used to orient the specimen. In the male, the bladder adjoins the rectum and seminal vesicles posteriorly, the prostate inferiorly, and the pubis and peritoneum anteriorly. In the female, the vagina is located posteriorly, and the uterus is located superiorly. Once the specimen is oriented, both ureters and, when present, the vasa deferentia should be identified. Location and dissection of the ureters is easier after fixation. The outer dimensions of the urinary bladder, as well as the length and diameter of ureters, should be recorded. The external surface of the bladder should be inked.
The minimum number of sections to be taken are as follows: tumor bladder neck , trigone , anterior wall , posterior wall , lateral walls , dome , ureteral orifices , margins , any abnormal appearing bladder mucosa and any perivesical lymph nodes .
Figure 18
You May Like: Does Amelanotic Melanoma Blanch When Pressed
Urothelial Carcinoma With Trophoblastic Differentiation
More than 30 cases of urothelial carcinoma with areas of trophoblastic differentiation have been reported and a small subset has had symptoms related to excess human chorionic gonadotropin production including gynecomastia., , , , Although some of the early reports have described tumors that apparently were composed solely of tissue resembling choriocarcinoma, most tumors reported in the last three decades or so have been composed of a mixture of urothelial carcinoma with trophoblastic elements. A single case of micropapillary carcinoma with trophoblastic elements has been reported.
Figure 11
Urothelial carcinoma with trophoblastic differentiation. Choriocarcinoma component with biphasic histology including syncytiotrophoblastic giant cells.
Invasion Into The Lamina Propria
Urinary Bladder Tumour, Transurethral Resection: - INVASIVE HIGH-GRADE PAPILLARY UROTHELIAL CARCINOMA with lamina propria invasion.-- Muscularis propria present, NEGATIVE for muscularis propria invasion.-- NEGATIVE for lymphovascular invasion.-- Please see synoptic report.
Block letters
URINARY BLADDER LESION , TRANSURETHRAL RESECTION URINARY BLADDER TUMOUR : - INVASIVE HIGH-GRADE PAPILLARY UROTHELIAL CARCINOMA WITH LAMINA PROPRIA INVASION.- MUSCULARIS PROPRIA NEGATIVE FOR INVASIVE MALIGNANCY.- NEGATIVE FOR LYMPHOVASCULAR INVASION.
Recommended Reading: What Is Stage 4 Melanoma Cancer
Recommended Reading: How To Identify Basal Cell Carcinoma
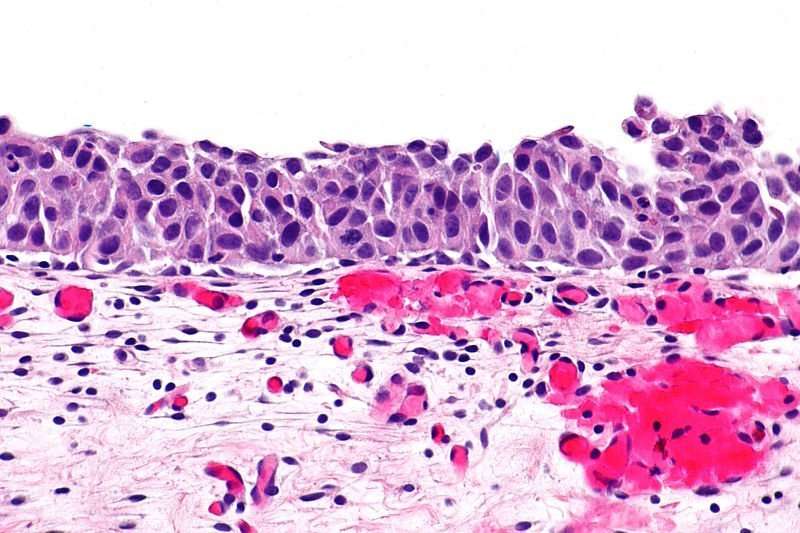
Start And Spread Of Bladder Cancer
The wall of the bladder has many several layers. Each layer is made up of different kinds of cells .
Most bladder cancers start in the innermost lining of the bladder, which is called the urothelium or transitional epithelium. As the cancer grows into or through the other layers in the bladder wall, it has a higher stage, becomes more advanced, and can be harder to treat.
Over time, the cancer might grow outside the bladder and into nearby structures. It might spread to nearby lymph nodes, or to other parts of the body.
Diagnosis Of Upper Tract Urothelial Carcinoma
Often times a CT scan, usually a CT urogram is done. Somtimes depending on the kidney function, a MR urogram, which is MRI test, can be used instead. Somtimes the urologist has to diagnose UTUC by looking into the ureter and kidney.
Retrograde pyelogram is where a urologist takes the patient to the operating roomand uses a tiny camera passed up the urethra into the bladder and up into the ureter. Then some contrast dye is injected into the ureter, which then fills up the collecting system and can demonstrate a tumor.
A simple urine sample called a urine cytology is often helpful. The pathologist looks under the microscope and tells us that these are cancerous cells that are coming from the urinary system.
Its not a very sensitive test but it is a specific test. So see if a tumor is there then we have to use a camera and a very small scope to go and look at the ureter and the renal pelvis and try to get a biopsy.
Read Also: How To Identify Basal Cell Carcinoma
What Is A Urothelial Neoplasm
Urothelial neoplasm, or transitional carcinoma , is a type of cancer that begins in transitional tissue, which is found in the urinary system, including the kidneys, bladder, and ureters, as well as certain parts of the prostate. Transitional epithelium is a kind of tissue having the ability to stretch, accommodating the primary function of the urinary tract the collection, production, and storage of urine. Manifest by express growth of abnormal epithelial cells, chief symptoms of urothelial neoplasm are abdominal pain and blood in the urine. Though no known cause of TCC exists, certain risk factors may be contributors such as smoking cigarettes and chemotherapy.
Unless the cancer condition is significantly advanced or the health of the patient is poor, typical treatment for urothelial neoplasm is surgery, as well as chemotherapy and immunotherapy. Drugs taken for the purpose of destroying cancerous cells, chemotherapeutic agents are administered locally via catheter into the renal pelvis or systemically. Given to strengthen the patient’s immunity either alone or in conjunction with chemotherapy, immunotherapy is more effective against low-stage, low-grade cancer.
Prognosis For Bladder Cancer
Superficial bladder cancer rarely causes death. Carcinoma in situ may be more aggressive. For patients with invasion of the bladder musculature, the 5-year survival rate is about 50%, but neoadjuvant chemotherapy improves these results in chemosensitive patients. Generally, prognosis for patients with progressive or recurrent invasive bladder cancer is poor. Prognosis for patients with squamous cell carcinoma or adenocarcinoma of the bladder is also poor because these cancers are usually highly infiltrative and often detected at an advanced stage.
Don’t Miss: Can Squamous Cell Carcinoma Metastasis
Carcinomas With Deceptively Bland Features
The vast majority of invasive urothelial carcinomas of the bladder and upper tract are diagnostically relatively straightforward from the histological characterization perspective because of the obvious cytologic atypia and infiltrative growth. In recent years, there has been an increased attention on subtle forms of cancer, which may be underdiagnosed either because of their relatively innocuous cytological features or because of their striking similarity to the slightly more commonly occurring benign proliferations in the urinary bladder. Dr Young and colleagues, have pointed out that to appreciate these subtle and diagnostically difficult small groups of tumors, it is important to recognize that these tumors re-capitulate what is seen in various benign lesions. The homology between the neoplastic and non-neoplastic lesions modified from their original observations is summarized in ., ,
Table 2 Similarities between neoplastic and non-neoplastic lesions based on architecture*
Intravesical Taxane And Mycobacterial Cell Wall Extract
Docetaxel is a cytotoxic chemotherapy agent that has shown potential in BCG failure in a phase I trial . This trial enrolled 18 patients whose condition had failed to respond to two courses of BCG or BCG plus INF. Fifty-six percent of patients had no evidence of disease at post-treatment cystoscopy and biopsy with minimal toxicity. Barlow and colleagues reported their experience of intravesical docetaxel after BCG failure . With a median follow up of 39 months, 32 of 54 patients had a complete response after induction therapy with 25% recurrence-free survival at 3 years. Fifty-four percent of these patients had a history of CIS and 83% had a history of high-grade disease.
Paclitaxel is a taxane-type agent with potential neoplastic activity when bound to albumin. A phase I study in recurrent high-grade NMIBC after failure of at least one standard intravesical regimen showed that nanoparticle albumin-bound paclitaxel had increased solubility and lower toxicity compared with docetaxel . A subsequent phase II trial showed a 35.7% complete response rate in a cohort of 28 patients with NMIBC and previous BCG failure .
Studies on intravesical taxanes and M. phlei extracts are limited with small treatment arms. Additional studies are necessary in the future to determine the ideal treatment schedule and efficacy.
You May Like: Osteomyoma
Carcinoma In Situ Of The Bladder
Carcinoma in situ of the bladder was first described in 1952 by Melicow . The diffuse nature of CIS was demonstrated in a subsequent report of 30 cases in which CIS extended from the renal pelvis to the penile urethra . Carcinoma in situ may occur as a primary disease, in association with papillary or solid tumors, or following tumor resection.
Irritative symptoms are common in patients with primary or concurrent CIS . Hematuria also is a frequent presenting feature. Urinary cytology is positive in more than 90% of patients with CIS and is an important diagnostic procedure because cystoscopic findings and even bladder biopsy may be falsely negative.
Clinical Course
The clinical course of CIS is highly variable, but overall, prior to the advent of BCG immunotherapy, 54% of patients progressed to muscle-invasive disease . Extensive, diffuse disease is considered to pose an increased risk for progression, whereas focal disease may exist for years and has a reported incidence of progression as low as 8% .
Focal CIS is the earliest stage in the evolution of invasive bladder cancer, and although its course is often protracted, regression virtually never occurs. Patients with focal disease are optimal candidates for intravesical therapy.
Radiation and Systemic Chemotherapy
Intravesical Chemotherapy
Biopsy And Tur Specimens
Small, noninvasive papillary neoplasms are often excised using biopsy with cold-cup forceps, diathermy forceps or a small diathermy loop. To avoid tissue distortion, these specimens should be transferred to fixative with minimal handling. Larger neoplasms are often sampled by TURB with a diathermy loop that produces strips of tissue approximately 6mm in width and of variable length. Additional resection of the tumor base may be obtained to assess the level of invasion . Any erythematous or velvety area of urothelium is sampled to exclude CIS. Random biopsies are also taken from cystoscopically normal urothelium remote from the tumor site to determine the extent of urothelial involvement. It has been suggested that random biopsy samples be obtained from predetermined sites in four quadrants of the urinary bladder. Some urologists also submit biopsy specimens of the urethra to assess the extent of disease.
Recommended Reading: Does Skin Cancer Itch And Burn
Early Bladder Cancer Staging
Early bladder cancer means the cancer cells are only in the inner lining of the bladder. They have not grown through the inner lining and into the deeper muscle layer of the bladder. It is early in its development.
Early bladder cancer is also called superficial bladder cancer, or non muscle invasive bladder cancer.
Ial Cystectomy And Urachal Resection Specimens
Partial cystectomy specimens should be fixed and dissected according to the guidelines of radical cystectomy . The edges of the specimen are inked because these represent the surgical margins of the bladder wall. A variation of the partial cystectomy is performed for resections of urachal tract neoplasms. These specimens consist of the dome of the bladder in continuity with the urachal tract including the umbilicus. After inking the soft tissue margin, the urachal tract should be serially sectioned at right angles to the long axis from the bladder to the umbilicus. Submit for histology a number of these urachal tract cross-sections, as well as the standard bladder sections. Appropriate samples of the soft tissue margin surrounding the urachus and of the skin margin around the umbilicus should be submitted for histology.
Read Also: Soderstrom Skin Cancer Screening
Micropapillary Variant Of Urothelial Carcinoma
Approximately 120 cases of this variant have been reported since the first description of a series of cases in the urinary bladder in 1994., , , , , , , , , , , This rare histological variant comprises 0.61% of urothelial carcinomas and shows a definite male predominance , which is higher than in conventional urothelial carcinoma . This histological variant of urothelial carcinoma has a micropapillary architecture, which is reminiscent of the papillary configuration seen in ovarian papillary serous tumors . The majority of tumors are muscle invasive at the time of presentation. Histologically, the micropapillary component of these tumors may be encountered in the non-invasive component, invasive component and in metastasis. This pattern may be focal, extensive or exclusive. The percentage of micropapillary component has been shown to be a significant adverse prognostic factor. There is no specified criterion required to designate a case as micropapillary carcinoma, and most series in the literature have included cases with < 10% to almost pure micropapillary histology. The author personally diagnoses cases specifying the percentage of micropapillary histology using terminology such as Urothelial carcinoma, high grade, with micropapillary histology and invasion into muscularis propria accompanying urothelial carcinoma in situ, non-papillary mucosa.
Figure 7