Combined Nivolumab And Ipilimumab
Nivolumab and ipilimumab have complementary activity in metastatic melanoma. In the CheckMate 067 study, a randomized, double-blind, multicenter, phase 3 trial in 945 previously untreated patients with metastatic melanoma, nivolumab combined with ipilimumab and nivolumab alone resulted in significantly longer progression-free survival than ipilimumab alone in those patients with PD-L1negative tumors, combination therapy was more effective than either agent alone.
On 5-year follow-up of CheckMate 067 patients, overall survival was 52% in the nivolumab-plus-ipilimumab group, compared with 44% in the nivolumab group and 26% in the ipilimumab group. Median overall survival was more than 60.0 months in the nivolumab-plus-ipilimumab group, 36.9 months in the nivolumab group, and 19.9 months in the ipilimumab group. Hazard ratios for death were 0.52 with nivolumab plus ipilimumab vs ipilimumab, and 0.63 with nivolumab vs ipilimumab. Current National Comprehensive Cancer Network guidelines include nivolumab plus ipilimumab as one of the preferred first-line therapeutic options for unresectable or malignant melanoma.
Expert Review And References
- American Society of Clinical Oncology. Melanoma. 2015: .
- Cancer Care Nova Scotia. Guidelines for the Management of Malignant Melanoma. 2013: .
- National Cancer Institute. Melanoma Treatment for Health Professionals . 2016: .
- National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Melanoma . 2016.
- Princess Margaret Cancer Centre. Princess Margaret Cancer Centre Clinical Practice Guidelines: Melanoma. 2015: .
- Ribas A, Slingluff Cl Jr, Rosenberg SA. Cutaneous melanoma. DeVita VT Jr, Lawrence TS, Rosenberg SA. Cancer: Principles and Practice of Oncology. 10th ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins 2015: 94:1346-1394.
Prognostic Factors For Metastatic Melanoma
Many factors have been proposed to influence the prognosis in patients with metastatic melanoma. The impact of the initial site of metastasis on survival was studied in a multivariate analysis of 1,521 patients with stage IV melanoma. Three groups of patients were identified: those with cutaneous, nodal, or gastrointestinal tract metastases those with isolated pulmonary metastases and those with liver, brain, or bone metastases. The median survivals in these three groups were 12.5, 8.3, and 4.4 months, respectively. The 5-year actuarial survivals were 14%, 4%, and 3%, respectively. In addition to the site of disease, the presence of an elevated serum lactate dehydrogenase has also been associated with poor prognosis. The 2002 American Joint Committee on Cancer staging system of cutaneous melanoma classifies patients with metastatic disease into three categories based on the site of metastases and serum LDH level .
Don’t Miss: Grade 3 Cancer Treatment
The Stage Of Melanoma Depends On The Thickness Of The Tumor Whether Cancer Has Spread To Lymph Nodes Or Other Parts Of The Body And Other Factors
To find out the stage of melanoma, the tumor is completely removed and nearby lymph nodes are checked for signs of cancer. The stage of the cancer is used to determine which treatment is best. Check with your doctor to find out which stage of cancer you have.
The stage of melanoma depends on the following:
- The thickness of the tumor. The thickness of the tumor is measured from the surface of the skin to the deepest part of the tumor.
- Whether there are:
- Satellite tumors: Small groups of tumor cells that have spread within 2 centimeters of the primary tumor.
- Microsatellite tumors: Small groups of tumor cells that have spread to an area right beside or below the primary tumor.
- In-transit metastases: Tumors that have spread to lymph vessels in the skin more than 2 centimeters away from the primary tumor, but not to the lymph nodes.
Treatment And Prognosis Of Primary Malignant Melanoma Of The Esophagus

Lei Cheng1,2, Zheng-Ying Guo2, Lei Lei3, Wen-Xian Wang3, Chun-Wei Xu4, Mei-Yu Fang3
1 Chinese Academy of Sciences University Cancer Hospital , Institute of Cancer and Basic Medicine of Chinese Academy of Sciences , Chinese Academy of Sciences University Cancer Hospital , Department of Respiratory Medicine, Jinling Hospital , Nanjing University School of Medicine , , China
Contributions: Conception and design: L Cheng, CW Xu, MY Fang Administrative support: None Provision of study materials or patients: L Cheng, ZY Guo, L Lei, WX Wang Collection and assembly of data: L Cheng, L Lei Data analysis and interpretation: L Cheng, L Lei, WX Wang Manuscript writing: All authors Final approval of manuscript: All authors.
Correspondence to:
Background: Primary malignant melanoma of the esophagus is rare with high malignancy and poor prognosis. The aim of this study was to investigate the relationship between prognosis and clinicopathological characteristics of this disease.
Results: The 1-year disease-free survival and overall survival rates of stage II who received surgery were 50% and 100% respectively. The 2-year DFS and OS rates were 50% and 75% , respectively. However, patients with stage IIIIV have a very poor prognosis. The 1-year OS is 0%.
Due to the small sample size, the statistic efficacy is low, but it can provide a certain theoretical basis for future research.
Submitted Nov 01, 2019. Accepted for publication Feb 05, 2020.
doi: 10.21037/tcr-19-2349
Read Also: What Are The Causes Of Carcinoma Cancer
Treatment Of Stage Ii Melanoma
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of stage II melanoma may include the following:
- Surgery to remove the tumor and some of the normal tissue around it. Sometimes lymph node mapping and sentinel lymph node biopsy are done to check for cancer in the lymph nodes at the same time as the surgery to remove the tumor. If cancer is found in the sentinel lymph node, more lymph nodes may be removed.
- A clinical trial of new types of treatment to be used after surgery.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
What Are The Causes
The cause of melanoma is not entirely understood but there is strong evidence to suggest that ultraviolet radiation caused by exposure to high intensity sunshine is a major factor. People with fair or red complexions are particularly at risk especially if they have been sunburnt during childhood and early adulthood. A small group of people may have a genetic predisposition to the development of melanoma and the use of sun beds is also thought to increase the risk of developing skin cancer.
Recommended Reading: Carcinoma Causes
Deterrence And Patient Education
Patients need to receive counsel to engage in preventative activities, especially once they have been treated for melanoma. These actions include:
- Avoid midday sun
- Use sunscreen at all times of the year
- Don protective clothing to cover skin
- Avoid tanning beds
- Be familiar with their skin so they can promptly spot changes – this includes areas that may not receive much sun exposure
What Tests Are Used To Stage Melanoma
There are several tests your doctor can use to stage your melanoma. Your doctor may use these tests:
- Sentinel Lymph Node Biopsy: Patients with melanomas deeper than 0.8 mm, those who have ulceration under the microscope in tumors of any size or other less common concerning features under the microscope, may need a biopsy of sentinel lymph nodes to determine if the melanoma has spread. Patients diagnosed via a sentinel lymph node biopsy have higher survival rates than those diagnosed with melanoma in lymph nodes via physical exam.
- Computed Tomography scan: A CT scan can show if melanoma is in your internal organs.
- Magnetic Resonance Imaging scan: An MRI scan is used to check for melanoma tumors in the brain or spinal cord.
- Positron Emission Tomography scan: A PET scan can check for melanoma in lymph nodes and other parts of your body distant from the original melanoma skin spot.
- Blood work: Blood tests may be used to measure lactate dehydrogenase before treatment. Other tests include blood chemistry levels and blood cell counts.
You May Like: Invasive Ductal Carcinoma Grade 2 Survival Rate
How Does A Doctor Know The Stage Of A Patient’s Melanoma
When your dermatologist found a spot on your skin that looked like a skin cancer, your dermatologist performed a skin biopsy. This involved giving you an injection to numb the area and then removing all the spot.
The skin that your dermatologist removed was then sent to a lab, where another doctor looked at it under a microscope. This doctor saw melanoma cells.
When a doctor, who is either a dermatopathologist or pathologist, sees melanoma cells, this doctor also tries to determine the stage of the melanoma. When its possible to figure out the stage, the doctor includes this information in your biopsy report. This is a report that the doctor writes and sends to your dermatologist. It explains what the doctor saw under the microscope.
Because the doctor sees only the skin that your dermatologist removed, your dermatologist also uses the findings from your complete skin exam and physical to help determine the stage of the melanoma.
Sometimes, more information is needed to determine the stage.
Unusual Moles Exposure To Sunlight And Health History Can Affect The Risk Of Melanoma
Anything that increases your risk of getting a disease is called a risk factor. Having a risk factor does not mean that you will get cancer not having risk factors doesn’t mean that you will not get cancer. Talk with your doctor if you think you may be at risk.
Risk factors for melanoma include the following:
- Having a fair complexion, which includes the following:
- Fair skin that freckles and burns easily, does not tan, or tans poorly.
- Blue or green or other light-colored eyes.
- Red or blond hair.
Being White or having a fair complexion increases the risk of melanoma, but anyone can have melanoma, including people with dark skin.
See the following PDQ summaries for more information on risk factors for melanoma:
Read Also: Lobular Breast Cancer Stage 1
What Are Targeted Therapies
A targeted therapy is a drug that blocks the growth of cancer by interfering with specific molecules involved in tumour growth. This is different to non-specific treatments like chemotherapy that simply aim to kill rapidly dividing cells.
This new generation of drugs has resulted in a big improvement in melanoma treatment for patients with the spread of the disease to other organs.
Researchers have identified some of the key genetic mutations that drive the growth of melanoma in patients. These discoveries are opening new avenues for treatment options using drugs that selectively block activity of these driving mutations, known as targeted therapy.
The genetic mutations involved in melanoma development that have been discovered so far have interesting names. They include:
- BRAF
More mutations are continuing to be discovered.
Malignant Melanoma How Is It Diagnosed
Early diagnosis is essential. In a previous blog, I have emphasized the concept of #SeeSomethingDoSomething initiated by board-certified veterinary oncologist, Dr. Sue Ettinger . For example, any skin mass that has been present for more than one month and/or is larger than the size of a pea should be evaluated by a veterinarian. This evaluation should include either aspiration or biopsy of the mass. No veterinarian can simply look or touch a skin mass and know what it is. As Dr. Ettinger advocates, #WhyWaitAspirate!
An aspiration involves inserting a vaccine-sized needle into the tumor and removing some cells. Aspirating skin masses does not typically require sedation, but sampling from an oral often requires sedation. The aspirated cells should be evaluated by a board-certified veterinary clinical pathologist to obtain a definitive diagnosis. The evaluation of the aspirated cells is called cytology. Occasionally, cytology is not diagnostic. In such cases, a surgical biopsy is required to obtain a definitive diagnosis.
Once a malignant melanoma has been confirmed, some additional non-invasive testing is recommended to determine how involved the body is with the cancerous process. These tests include:
- Stage I: Primary tumor < 2 cm in diameter
- Stage II: Primary tumor 2 to < 4 cm in diameter
- Stage III: Primary tumor larger than 4 cm in diameter and/or metastasis to lymph node
- Stage IV: Distant metastasis present
Read Also: How Fast Does Cancer Kill
Can Changing My Diet Help Prevent Melanoma
The American Cancer Society advocates eating a plant-based diet over an animal-based diet as part of a healthy plan to avoid all cancers. Growing evidence suggests that plants pack a powerful punch in any fight against cancer because they’re nutritious, cholesterol-free and fiber-rich.
Theres no doubt that a healthy diet can protect your immune system. Having a strong immune system is important to help your body fight disease. Some research has shown that a Mediterranean diet is a healthy choice that may help prevent the development of cancer. Talk to your healthcare provider about the role food plays in lowering your cancer risks.
Some skin and immune-system healthy foods to consider include:
- Daily tea drinking: The polyphenols in tea help strengthen your immune system. Green tea contains more polyphenols than black tea.
- High vegetable consumption: Eating carrots, cruciferous and leafy vegetables is linked to the prevention of cutaneous melanoma.
- Weekly fish intake: Study participants who ate fish weekly seemed to avoid developing the disease when compared to those who did not eat fish weekly.
What Are The Signs Of Melanoma
Knowing how to spot melanoma is important because early melanomas are highly treatable. Melanoma can appear as moles, scaly patches, open sores or raised bumps.
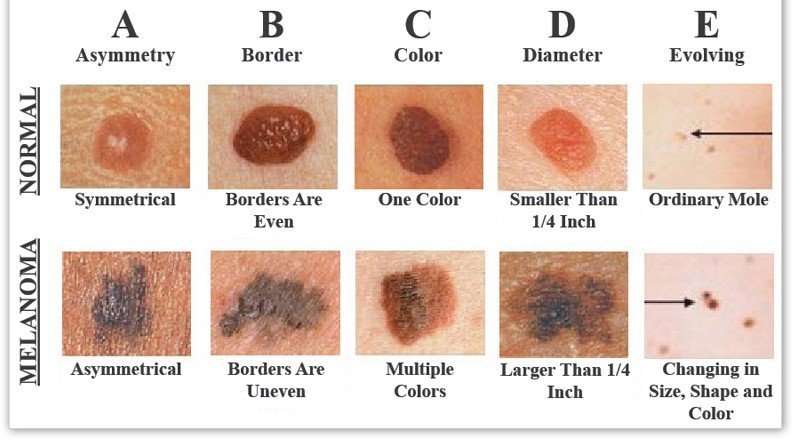
Use the American Academy of Dermatology’s “ABCDE” memory device to learn the warning signs that a spot on your skin may be melanoma:
- Asymmetry: One half does not match the other half.
- Border: The edges are not smooth.
- Color: The color is mottled and uneven, with shades of brown, black, gray, red or white.
- Diameter: The spot is greater than the tip of a pencil eraser .
- Evolving: The spot is new or changing in size, shape or color.
Some melanomas don’t fit the ABCDE rule, so tell your doctor about any sores that won’t go away, unusual bumps or rashes or changes in your skin or in any existing moles.
Another tool to recognize melanoma is the ugly duckling sign. If one of your moles looks different from the others, its the ugly duckling and should be seen by a dermatologist.
Also Check: Skin Cancer Spread To Lymph Nodes
Treatment Of Braf V600 Wild
The first choice of first-line treatment for patients with BRAF V600 wild-type, unresectable or metastatic melanoma is nivolumab plus ipilimumab.
Nivolumab , another PD-1 inhibitor, was granted accelerated approval in December 2014 for unresectable or metastatic melanoma and disease progression following ipilimumab treatment and, if BRAF V600 mutation positive, a BRAF inhibitor. Approval was based on interim results of a randomized clinical trial in patients with unresectable or metastatic melanoma that had progressed after ipilimumab. Interim analysis confirmed objective responses in 38 of the first 120 patients treated with nivolumab versus five of 47 patients who received investigator’s choice of chemotherapy .
Nivolumab monotherapy was approved in November 2015 on the basis of data from the randomized phase 3 CheckMate-066 trial, which compared nivolumab monotherapy with dacarbazine in the first-line treatment of 418 patients with advanced BRAF wild-type melanoma. In an interim analysis, nivolumab demonstrated superior overall survival, which was the primary outcome. The overall survival rate at 1 year was 72.9% in the nivolumab group versus 42.1% in the dacarbazine group.
A significant benefit with respect to overall survival was observed in the nivolumab group, as compared with the dacarbazine group . Median progression-free survival was also improved in the nivolumab-treated patients compared with dacarbazine .
How Do They Work
Messages are sent inside the cell by a series of molecules that tell the cell how to grow and divide. This process is called a signalling pathway.
Mutations, or abnormalities, in these signalling pathways can cause cells to rapidly divide and replicate out of control, resulting in tumour formation. The mutated signalling pathways in melanoma cells are the targets for therapy.
Not all melanomas have the same driving mutations. By identifying which molecules are mutated in different forms of the disease patients can be categorised and treated based on their specific mutation. Identifying all of these molecular mutations is what molecular oncology researchers around the world are working on.
Recommended Reading: Invasive Breast Cancer Survival Rate
Enhancing Healthcare Team Outcomes
Skin cancers are frequently seen by primary care providers, nurse practitioners, internists, and pharmacists this is why an interprofessional team approach is needed. While many skin lesions are benign, it is important always to consider melanoma- as it is potentially deadly if the diagnosis gets missed. If there is suspicion of melanoma, the patient should obtain a referral to the dermatologist/oncologist and pathologist for further workup, irrespective of which of the other healthcare providers first became suspicious. Surgery includes wide local excision with sentinel lymph node biopsy, elective node dissection, or both. These surgical procedures are the definitive treatment for early-stage melanoma.
When performing the wide local excision, first consider the surgical margins. If the primary closure is not feasible, skin grafting or tissue transfers may be needed. Medical management is reserved for adjuvant therapy of patients with advanced melanoma here again, the pharmacist can monitor medications and consult with the dermatologist. Dermatology nursing staff will assist at all stages of case management, and provide patient counsel and monitor the condition, reporting to the treating clinician as necessary. For localized lesions, the prognosis is with surgery, but advanced melanoma has a grim prognosis, but the interprofessional team approach to care will optimize the patient’s prospects for a better outcome.