How Is Merkel Cell Carcinoma Treated
Your treatment plan depends on how early your doctor diagnoses the cancer, your overall health, and whether cancer cells have spread to other tissues in your body. Treatment for MCC usually involves one or a combination of therapies, including:
- Immunotherapy, which uses specific medications to help your immune system fight cancer. Immune agents in use for MCC include avelumab , nivolumab, and pembrolizumab .
- Surgery, which is a procedure that cuts out cancerous tissues. This type of therapy often involves a type of surgery called Mohâs micrographic surgery, a layer-by-layer skin removal method. Mohâs allows doctors to assess tissue under a microscope during the treatment and to save skin appearance and function. This is especially beneficial to people who have cancer on their faces.
- Radiation therapy, which uses highly charged particles to kill cancer cells. This method is often combined with Mohâs surgery to improve results.
- Chemotherapy, which uses drugs to kill cancer. This method of treatment was previously used more often, but was not found to give lasting results.
Tests Treatment And Medications
Before diagnosing this condition, the affected person should confirm it with a second opinion to make sure the diagnosis is right. The treatment plan is started after the confirmation of the diagnosis. Physical examination is also done to look and feel for the nodules or lumps. Biopsy is also recommended to test for this carcinoma. Other treatment option includes:
-Surgery is performed to remove the lumps or nodules
-Chemotherapy is done most especially when the metastatic carcinoma has infected the underlying tissues
-Radiation is also done to target the metastatic nodules
-Biopsy is done to detect if the nodule is benign or malignant
-CT scan, PET scan and X-ray is recommended to view if the carcinoma has already spread to the entire body
Merkel Cell Carcinoma: Causes Symptoms And Treatment
Merkel cell carcinoma is a rare, aggressive type of skin cancer.
Merkel cell carcinoma gets its name because these skin cancer cells resemble Merkel cells, which are located in the top layer of skin. Merkel cells are most concentrated in the fingertips, lips, and face, but MCC cells are most likely to develop on the head, neck, and other areas that have received the most sun exposure.
Below, learn about the causes of MCC, its symptoms, and how to prevent it. We also describe the diagnosis and treatment options.
Carcinoma is a type of cancer that develops in the skin or tissues covering or lining internal organs. Cancer occurs when cells begin to randomly divide and grow out of control. This cellular growth eventually forms a mass called a cancerous tumor.
MCC is one type of skin cancer, and its cells resemble Merkel cells. These are located close to the skins nerve endings and help provide a sense of light touch. They also relay information from the skin to the brain about details such as pressure and texture.
Merkel cells share traits with nerve and hormone-producing cells. As a result, they are classed as neuroendocrine cells, and MCC, in turn, is sometimes called neuroendocrine carcinoma of the skin. Another name for MCC is trabecular carcinoma.
MCC is very rare. In 2018, around 2,000 people in the United States received the diagnosis. However, its prevalence seems to be growing.
Don’t Miss: How To Identify Basal Cell Carcinoma
Merkel Cell Carcinoma Incidence Trends And Survival Rates Among Adults Aged 50 Years From United States Cancer Statistics
J Am Acad Dermatol.J Am Acad Dermatol.
National Program of Cancer Registries and Surveillance, Epidemiology, and End Results SEER*Stat Database: NPCR and SEER Incidence US Cancer Statistics 20012015 Public Use Research Database, United States Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute. Released June 2018, based on the November 2017 submission. Accessed at www.cdc.gov/cancer/npcr/public-use.
| Category |
|---|
Merkel Cell Carcinoma Treatment Health Professional Version
On This Page
Merkel cell carcinoma was originally described by Toker in 1972 as trabecular carcinoma of the skin. Other names include Toker tumor, primary small cell carcinoma of the skin, primary cutaneous neuroendocrine tumor, and malignant trichodiscoma.
MCC is an aggressive neuroendocrine carcinoma arising in the dermoepidermal junction , and it is the second most common cause of skin cancer death after melanoma. Although the exact origin and function of the Merkel cell remains under investigation, it is thought to have features of both epithelial and neuroendocrine origin and arise in cells with touch-sensitivity function .
Therapeutic options have been historically limited for patients with advanced disease however, new immunotherapeutic approaches are associated with durable responses.
Don’t Miss: Metastatic Basal Cell Carcinoma Survival Rate
Who Gets Merkel Cell Carcinoma
Merkel cell carcinoma has an estimated incidence of 0.23 per 100,000 people in Caucasian populations, which is much less common than melanoma.
- Increasing numbers of Merkel cell carcinomas have been reported by some centres in recent years.
- Merkel cell carcinoma mainly affects older people, with most cases occurring after the age of 50.
- It is slightly more common in men.
- It occurs on parts of the body commonly exposed to sunlight, most often the head and neck.
- It is also more common and more serious in those that are immune suppressed, such as patients with solidorgan transplants, human immunodeficiency virus infection, haematologicalmalignancy or on drugs such as azathioprine.
Symptoms: Know The Early Warning Signs Of Merkel Cell Carcinoma
The shape and color of MCC nodules are less distinctive than other skin cancers. In fact, many mistake them for other skin issues, such as bug bites, sores, cysts, sties, or pimples, according to the American Academy of Dermatology. Often, it is only the speed with which these lesions grow that attracts the attention of patients and their doctors.
With early detection and treatment, MCC can be well contained and often cured. Treatment becomes more difficult as the tumor grows and spreads. Thats why its critical to recognize this cancer in its earliest stage.
Common characteristics of MCC:
RELATED: Is It Toenail Fungus or Something Else?
You May Like: What Is The Most Aggressive Skin Cancer
Statistics: How Common Is Merkel Cell Carcinoma
Skin cancer is the most common form of cancer in the United States.
Though MCC is much less common than other types of skin cancer roughly 30 times less common than melanoma incidence has been increasing quickly, having quadrupled in the past few decades.
According to the Skin Cancer Foundation, roughly 2,500 new cases of MCC are diagnosed annually in the United States.
Though MCC is very rare, incidence has been rising quickly. A study published in the March 2018 issue of the Journal of the American Academy of Dermatology found that between 2000 and 2013, MCC increased by 95 percent. This trend is expected to continue, with annual incidence reaching 3,250 cases per year by 2025.
Some of the uptick in MCC is likely due to the fact that lab tests to diagnose MCC have become more accurate. But it might also be caused by increases in risk factors. More people are living longer, and many people over age 65 did not regularly protect their skin from the sun.
RELATED: The Difference Between Chemical and Mineral Sunscreen
Surgery For The Primary Lesion
In a review of 18 case series, 279 of 926 patients developed local recurrence during follow-up, excluding those presenting with distant metastatic disease at presentation. These recurrences have been typically attributed to inadequate surgical margins or possibly a lack of adjuvant radiation therapy.
Given the propensity of MCC to recur locally , wide local excision to reduce the risk of local recurrence has been recommended for patients with clinical stage I or stage II disease.
Recommendations about the optimal minimum width and depth of normal tissue margin to be excised around the primary tumor differ among the various retrospective case series, but this question has not been studied systematically. No definitive data suggest that extremely wide margins improve overall survival , although some reports suggest that wider margins appear to improve local control. Frozen-section evaluation of margins may be useful, especially when the tumor is in an anatomical site that is not amenable to wide margins.
Some authors have advocated the use of Mohs micrographic surgery as a tissue-sparing technique. The relapse rate has been reported to be similar to or better than that of wide excision, but comparatively few cases have been treated in this manner and none in randomized, controlled trials.
Read Also: Does Amelanotic Melanoma Blanch When Pressed
Preventing Merkel Cell Carcinoma
There are a number of measures you can take to reduce your risk of developing MCC . Its never too late to start.
- Limit UV exposure. You can practice prevention every day by wearing protective hats and clothing, avoiding the midday sun and tanning beds, and using broad-spectrum sunscreen with an SPF of at least 30 even on cloudy days. Reapply sunscreen every two hours when swimming or sweating.
- Keep an eye out. MCC lesions dont have the dramatic look or color of other skin cancers. Thats why its so important to closely examine your skin from head to toe once a month. If you notice a new or unusual spot or a raised bump that seems to be growing, contact your doctor right away.
- Get screened. See a dermatologist once every year for a professional skin exam.
If youve been treated for MCC, also be sure to:
- Follow up regularly with your dermatologist once treatment is complete. Stick to the exam schedule your doctor recommends its the best way to quickly detect a recurrence.
- Play close attention to the site and surrounding region. MCC can return suddenly. Contact your medical team immediately if you see any suspicious changes.
- Consider getting the blood test that can help pick up recurrences early. The Merkel polyomavirus serology test measures antibodies to the Merkel polyomavirus in the blood. It can help pick up recurrences of MCC early, when they can be most effectively treated.
Radiation Therapy And Chemotherapy
Localized radiation therapy is commonly used to destroy any remaining cancer cells following surgery to remove Merkel cell tumors. Radiation is also occasionally used to treat the area surrounding lymph nodes that have been surgically removed. Radiation therapy delivers penetrating beams of energy waves or streams of particles to the cancer cells and a small margin around the tumor. Radiation therapy can also be used to treat patients who are not candidates for surgery because of ill health or the location of their tumor, or to treat tumors that have returned after an initial round of treatment.
Chemotherapy is another treatment option following surgery. The same platinum-based chemotherapy that is used for small cell lung cancer can be used against Merkel cell carcinoma that has spread to the lymph nodes. Patients whose tumors have spread to distant areas of the body or returned following initial treatment may also be treated with chemotherapy.
Neoadjuvant chemotherapy may be recommended for some patients with large Merkel cell tumors or lymph node involvement. Before this step is taken, however, consideration is needed to ensure that a patient treated with chemotherapy will still be healthy enough to subsequently undergo the surgery or radiation.
Although the rarity of Merkel cell carcinoma has made it difficult to study, researchers continue to evaluate the best ways to use radiation therapy and chemotherapy in caring for patients with the disease.
Also Check: Does Skin Cancer Burn And Itch
What Is The Survival Rate For Merkel Cell Carcinoma
It is also known as trabecular cancer. In some occasions, the skin above the tumor breaks open and bleeds.Characteristic features of the nodule are: 1. Together, were making a difference and you can, too. Weve invested more than $4.9 billion in cancer research since 1946, all to find more and better treatments, uncover factors that may cause cancer, and improve cancer patients quality of life.We couldnt do what we do without our volunteers and donors. Its also important to follow recommended screening guidelines, which can help detect certain cancers early.Whether you want to learn about treatment options, get advice on coping with side effects, or have questions about health insurance, were here to help. Become a volunteer, make a tax-deductible donation, or participate in a fundraising event to help us save lives.The American Cancer Society couldnt do what we do without the support of our partners. A Its prognosis is good if it is detected and treated at an early stage. Our articles are resourced from reputable online pages. Merkel cell carcinoma is a skin cancer characterized by uncontrolled and abnormal growth of Merkel cells in the skin.
If these cancer cells become malignant and spread to other parts of the body, then, it is severe and the survival rate of the patient may reduce inversely.
For reprint requests, please see our Cancer Information, Answers, and Hope.
This process is called a skin biopsy. These cells are found in the top layer of the skin.
Is Merkel Cell Carcinoma Worse Than Melanoma
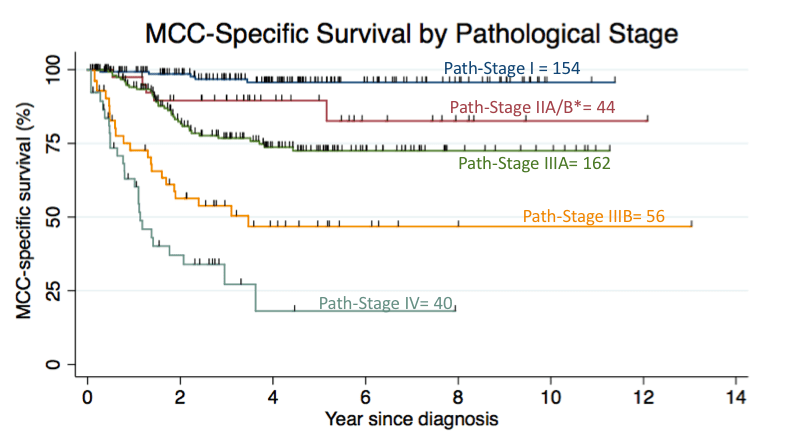
Based on statistical data of 5-year survival rate of both the skin cancers, Merkel cell carcinoma is more aggressive of the two and is more fatal as compared to melanoma. In the case of localized cancer, the 5-year survival rate of Merkel cell carcinoma is about 78% while that of melanoma is 98%4. The survival rate of Merkel cell carcinoma and melanoma, when cancer has spread to regional level is 51% and 64% respectively while in case of distant metastasis, the 5-year survival rate for Merkel cell carcinoma and melanoma is 17% and 23% respectively.
Don’t Miss: Does Amelanotic Melanoma Blanch When Pressed
What Are The Clinical Features Of Merkel Cell Carcinoma
Merkel cell carcinoma usually presents as a rapidly enlarging, solitary, irregular red nodule. It is often similar in appearance to other more common skin cancers such as basal cell carcinoma but grows much more quickly.
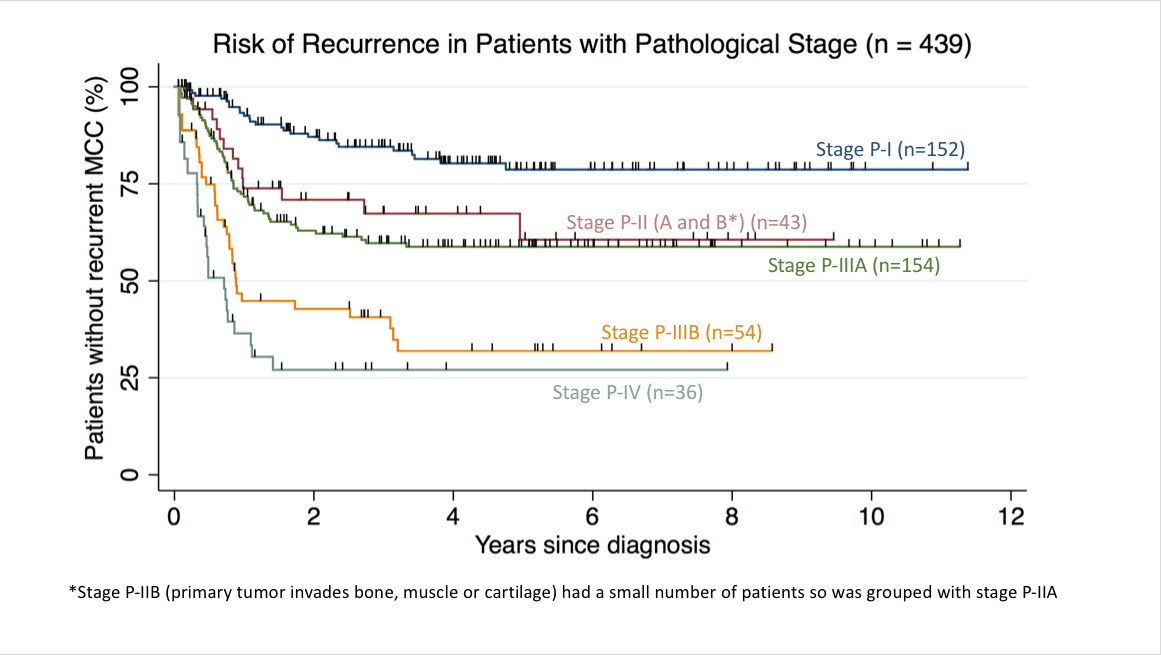
Merkel cell cancers spread through the lymphatic system and multiple metastases can develop around the main tumour . Merkel cell carcinoma may also spread to lymph nodes in the neck, axillae and groin. This is more likely in thicker tumours. Most recurrences occur within the first two years after diagnosis.
Merkel cell carcinoma
Prognosis & Survival Rate
The prognosis depended on the age and the severity of the carcinoma in the affected person. Survival rate of this is depends if it is benign or malignant cases. If benign, the survival rate can be higher if the treatment is done immediately. If malignant cases, it needs to assess whether the cancer cells has already metastasize deep down the underlying tissues in the body. In the research studies they found this type of cancer to mutate when detected. It also shows the inhibition of production of MVC proteins causing the MVC-infected merkell cell carcinoma cells to die but no effect on malignant ones. About 20% of this carcinoma is still having no known cause. However, there is a 5-year and 80% survival rate of chances of living when detected early.
Also Check: Soderstrom Skin Cancer Screening
Merkel Cell Carcinoma Survival Rate
Its difficult to assess the true Merkel cell carcinoma survival rate due to the rarity of the disease. When studying outcomes, researchers have been able to track the experiences of only a few individuals. Additionally, many of these patients were diagnosed several years ago, when treatments were not as advanced as they are today. As a result, theres no accurate way to predict any patients specific outcome.
What research does tell us is that:
At Moffitt Cancer Center, our expert oncologists take a comprehensive approach to Merkel cell carcinoma treatment. Skilled professionals from numerous disciplines come together to review each patients case and develop a highly individualized treatment plan. Moffitts patients have access to a wide range of options, including clinical trials. And, behind the scenes, our dedicated researchers are continually evaluating new treatments that could ultimately improve the Merkel cell carcinoma survival rate.
Patients can make an appointment at Moffitt with or without referrals. To schedule a visit, call or submit a new patient registration form online.
- BROWSE
How Dangerous Is Mcc
While MCC is about three to five times more likely to be deadly than melanoma, with early detection, MCC can be treated successfully. If you think you might have MCC, see your doctor. Treatment becomes increasingly difficult once the disease has spread, but new options are now available. Thanks to advances in the field of immunotherapy, MCC survival rates are improving.
Don’t Miss: Squamous Cell Carcinoma Skin Metastasis
Who Is Likely To Have Merkel Cell Carcinoma
Anyone can develop MCC. You are at higher risk of developing this type of cancer if you:
- Have lighter-colored skin
- Have a weakened immune system
- Use tanning beds or ultraviolet light therapy for psoriasis
- Have another type of cancer, especially another type of skin cancer
The incidence of MCC in the US is about 0.6 per 100,000 people per year. This is up about 4X since 1986. However, it must be noted that diagnosis has improved, the population is getting older, and immunosuppressant medications are rising. It is estimated that about 700 people with MCC die per year. The rate of death is about one in three. Melanoma, also a dangerous cancer, is said to kill about one in nine people per year.
Merkel Cell Carcinoma & Merkel Cell Polyoma Virus
Merkel cell carcinoma is also known as primary neuroendocrine carcinoma of the skin or trabecular cancer. While patients with a small tumor that has not yet metastasized have an expected 5-year survival rate of more than 80 percent, the rate drops to about 50 percent once the cancer has metastasized. Standard treatment options include surgery, radiation therapy and chemotherapy.
Approximately 80% of Merkel cell carcinomas are caused by Merkel cell polyomavirus . Additional risk factors are sun exposure and having a weak immune system.
MCPyV is the only polyomavirus discovered to date that is associated with a human cancer. MCPyV infection is highly prevalent in the general population. Nearly all healthy adults asymptomatically shed MCPyV from their skin. However, in elderly and immunosuppressed individuals, the infection can lead to Merkel cell carcinoma.
Because of the viral origin for this cancer, immunotherapies are a promising avenue for research to treat virus-positive Merkel cell carcinoma.
You May Like: Osteomyoma