Risk Of Further Melanomas
Most people treated for early melanoma do not have further trouble with the disease. However, when there is a chance that the melanoma may have spread to other parts of your body, you will need regular check-ups. Your doctor will decide how often you will need check-ups everyone is different. They will become less frequent if you have no further problems. After treatment for melanoma it is important to limit exposure to the sun’s UV radiation. As biological family members usually share similar traits, your family members may also have an increased risk of developing melanoma and other skin cancers. They can reduce their risk by spending less time in the sun and using a combination of sun protection measures during sun protection times. It is important to monitor your skin regularly and if you notice any changes in your skin, or enlarged lymph glands near to where you had the cancer, see your specialist as soon as possible.
Different Types Of Cancer Start In The Skin
Skin cancer may form in basal cells or squamous cells. Basal cell carcinoma and squamous cell carcinoma are the most common types of skin cancer. They are also called nonmelanoma skin cancer. Actinic keratosis is a skin condition that sometimes becomes squamous cell carcinoma.
Melanoma is less common than basal cell carcinoma or squamous cell carcinoma. It is more likely to invade nearby tissues and spread to other parts of the body.
This summary is about basal cell carcinoma, squamous cell carcinoma of the skin, and actinic keratosis. See the following PDQ summaries for information on melanoma and other kinds of cancer that affect the skin:
How Immunotherapy Comes Into Play
Immunotherapy helps your natural immune system to attack cancer cells.
One group of immunotherapy drugs in particular has shown great promise for treating advanced-stage melanoma. These drugs are known as checkpoint inhibitors. They help the immune systems T cells recognize and attack melanoma cells.
Studies have found these medications improve survival rates for people with advanced-stage melanoma, report the authors of a review article in the American Journal of Clinical Dermatology. Research published in The Oncologist has also found that people with melanoma can potentially benefit from treatment with these drugs, regardless of their age.
But immunotherapy doesnt work for everyone. According to a research letter published in the journal Nature Medicine, only a portion of people with melanoma benefit from treatment with checkpoint inhibitors. More research is needed to learn which people are most likely to respond well to this treatment.
Recommended Reading: What Is The Survival Rate For Invasive Ductal Carcinoma
What Tests Are Used To Stage Melanoma
There are several tests your doctor can use to stage your melanoma. Your doctor may use these tests:
- Sentinel Lymph Node Biopsy: Patients with melanomas deeper than 0.8 mm, those who have ulceration under the microscope in tumors of any size or other less common concerning features under the microscope, may need a biopsy of sentinel lymph nodes to determine if the melanoma has spread. Patients diagnosed via a sentinel lymph node biopsy have higher survival rates than those diagnosed with melanoma in lymph nodes via physical exam.
- Computed Tomography scan: A CT scan can show if melanoma is in your internal organs.
- Magnetic Resonance Imaging scan: An MRI scan is used to check for melanoma tumors in the brain or spinal cord.
- Positron Emission Tomography scan: A PET scan can check for melanoma in lymph nodes and other parts of your body distant from the original melanoma skin spot.
- Blood work: Blood tests may be used to measure lactate dehydrogenase before treatment. Other tests include blood chemistry levels and blood cell counts.
When Melanoma Can’t Be Cured
If your cancer has spread and it is not possible to cure it by surgery, your doctor may still recommend treatment. In this case, treatment may help to relieve symptoms, might make you feel better and may allow you to live longer.Whether or not you choose to have anti-cancer treatment, symptoms can still be controlled. For example, if you have pain, there are effective treatments for this. General practitioners, specialists and palliative care teams in hospitals all play important roles in helping people with cancer.
You May Like: Skin Cancer Metastasis To Lymph Nodes
How Is Melanoma Staged
Melanoma stages are assigned using the TNM system.
The stage of the disease indicates how much the cancer has progressed by taking into account the size of the tumor, whether its spread to lymph nodes, and whether its spread to other parts of the body.
A doctor can identify a possible melanoma during a physical exam and confirm the diagnosis with a biopsy, where the tissue is removed to determine if its cancerous.
But more sophisticated technology, such as PET scans and sentinel lymph node biopsies, are necessary to determine the cancers stage or how far its progressed.
There are five stages of melanoma. The first stage is called stage 0, or melanoma in situ. The last stage is called stage 4. Survival rates decrease with later stages of melanoma.
Its important to note that survival rates for each stage are just estimates. Each person with melanoma is different, and your outlook can vary based on a number of different factors.
New Types Of Treatment Are Being Tested In Clinical Trials
This summary section describes treatments that are being studied in clinical trials. It may not mention every new treatment being studied. Information about clinical trials is available from the NCI website.
Vaccine therapy
Vaccine therapy is a cancer treatment that uses a substance or group of substances to stimulate the immune system to find the tumor and kill it. Vaccine therapy is being studied in the treatment of stage III melanoma that can be removed by surgery.
Recommended Reading: Invasive Ductal Carcinoma Grade 2 Survival Rate
Treating Stage Iv Melanoma
Stage IV melanomas have already spread to distant lymph nodes or other areas of the body. Skin tumors or enlarged lymph nodes causing symptoms can often be removed by surgery or treated with radiation therapy.
Metastases in internal organs are sometimes removed, depending on how many there are, where they are, and how likely they are to cause symptoms. Metastases that cause symptoms but cannot be removed may be treated with radiation, immunotherapy, targeted therapy, or chemotherapy.
The treatment of widespread melanomas has changed in recent years as newer forms of immunotherapy and targeted drugs have been shown to be more effective than chemotherapy.
Immunotherapy drugs called checkpoint inhibitors such as pembrolizumab or nivolumab are typically the first drugs tried, especially in people whose cancer cells do not have BRAF gene changes. These drugs can shrink tumors for long periods of time in some people. Ipilimumab , a different type of checkpoint inhibitor, is not typically used by itself as the first treatment, although it might be combined with nivolumab or pembrolizumab. This slightly increase the chances that the tumor will shrink, although itâs also more likely to result in serious side effects, which needs to be considered carefully. People who get any of these drugs need to be watched closely for serious side effects..
Itâs important to carefully consider the possible benefits and side effects of any recommended treatment before starting it.
The Following Stages Are Used For Melanoma:
Stage 0
Stage I
- Stage IA: The tumor is not more than 1millimeter thick, with or without ulceration.
- Stage IB: The tumor is more than 1 but not more than 2 millimeters thick, without ulceration. Enlarge Stage I melanoma. In stage IA, the tumor is not more than 1 millimeter thick, with or without ulceration . In stage IB, the tumor is more than 1 but not more than 2 millimeters thick, without ulceration. Skin thickness is different on different parts of the body.
Stage II
- Stage IIA: The tumor is either:
- more than 1 but not more than 2 millimeters thick, with ulceration or
- more than 2 but not more than 4 millimeters thick, without ulceration. Enlarge Stage IIA melanoma. The tumor is more than 1 but not more than 2 millimeters thick, with ulceration OR it is more than 2 but not more than 4 millimeters thick, without ulceration. Skin thickness is different on different parts of the body.
Stage III
Stage III is divided into stages IIIA, IIIB, IIIC, and IIID.
Also Check: Can You Die From Basal Cell Skin Cancer
Staging For Basal Cell Carcinoma And Squamous Cell Carcinoma Of The Skin Depends On Where The Cancer Formed
Staging for basal cell carcinoma and squamous cell carcinoma of the eyelid is different from staging for basal cell carcinoma and squamous cell carcinoma found on other areas of the head or neck. There is no staging system for basal cell carcinoma or squamous cell carcinoma that is not found on the head or neck.
Surgery to remove the primary tumor and abnormal lymph nodes is done so that tissue samples can be studied under a microscope. This is called pathologic staging and the findings are used for staging as described below. If staging is done before surgery to remove the tumor, it is called clinical staging. The clinical stage may be different from the pathologic stage.
Where Research Is Headed
A 2017 review of phase III clinical trials found that current targeted therapies and immunotherapy work well to improve overall survival rates in people with advanced-stage melanoma. But the authors say that more research is needed to learn which therapy to try first.
Scientists are developing and testing strategies to identify which patients are most likely to benefit from which treatments. For example, researchers have found that people who have high levels of certain proteins in their blood may respond better than others to checkpoint inhibitors.
Studies are also underway to develop and test new therapies. According to an article in Gland Surgery, early research findings suggest that personalized anti-tumor vaccines may be a safe treatment approach. Scientists are also testing drugs that target melanoma with certain abnormal genes, reports the American Cancer Society.
New combinations of existing treatments might also help improve outcomes for some people with melanoma. Scientists are continuing to study the safety, efficacy, and optimal use of medications that have already been approved to treat this disease.
Read Also: Basal Skin Cancer Survival Rates
Survival Rates For Melanoma Skin Cancer
Survival rates can give you an idea of what percentage of people with the same type and stage of cancer are still alive a certain amount of time after they were diagnosed. They cant tell you how long you will live, but they may help give you a better understanding of how likely it is that your treatment will be successful.
Keep in mind that survival rates are estimates and are often based on previous outcomes of large numbers of people who had a specific cancer, but they cant predict what will happen in any particular persons case. These statistics can be confusing and may lead you to have more questions. Talk with your doctor about how these numbers may apply to you, as he or she is familiar with your situation.
What Could Be The Harm In Trying Home Remedies For Skin Cancer First

First, you may not know exactly what kind of lesion you are self-treating. Accurate diagnosis of skin cancer requires examination by a healthcare professional. There are three main types of skin cancer, and several subtypes of each. Although there are typical features of each type, cancerous lesions may have atypical features. Even dermatologists use special magnifying glasses and handheld imaging devices. These tools help them to identify suspicious lesions. A skin biopsy is needed to confirm that a lesion is cancerous.
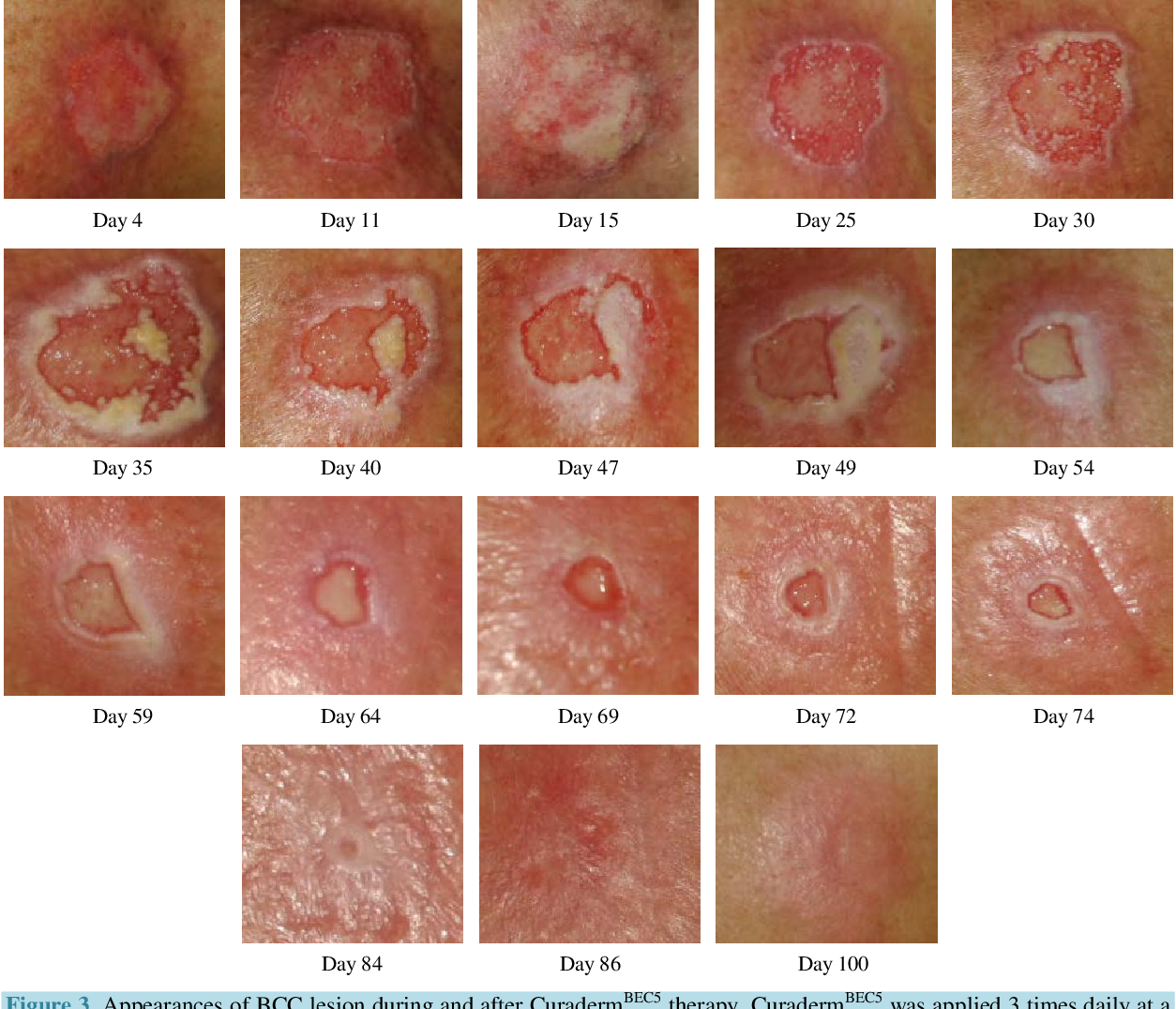
Second, delaying effective treatment for skin cancer can lead to worse outcomes. One risk of using a home remedy is that it will not work, giving the cancer time to grow. Of the three major skin cancers, melanoma is the most likely to invade and spread if it is not treated early.1 About 5% to 10% of squamous cell carcinoma is aggressive.2 Squamous cell carcinoma is difficult to treat once it spreads. Although basal cell carcinoma rarely spreads to distant parts of the body, it can grow into bone or the tissue below the skin if left untreated.3
Don’t Miss: Can You Die From Basal Cell Skin Cancer
Choosing To Stop Treatment Or Choosing No Treatment At All
For some people, when treatments have been tried and are no longer controlling the cancer, it could be time to weigh the benefits and risks of continuing to try new treatments. Whether or not you continue treatment, there are still things you can do to help maintain or improve your quality of life.
Some people, especially if the cancer is advanced, might not want to be treated at all. There are many reasons you might decide not to get cancer treatment, but its important to talk to your doctors and you make that decision. Remember that even if you choose not to treat the cancer, you can still get supportive care to help with pain or other symptoms.
Unusual Moles Exposure To Sunlight And Health History Can Affect The Risk Of Melanoma
Anything that increases your risk of getting a disease is called a risk factor. Having a risk factor does not mean that you will get cancer not having risk factors doesn’t mean that you will not get cancer. Talk with your doctor if you think you may be at risk.
Risk factors for melanoma include the following:
- Having a fair complexion, which includes the following:
- Fair skin that freckles and burns easily, does not tan, or tans poorly.
- Blue or green or other light-colored eyes.
- Red or blond hair.
Being White or having a fair complexion increases the risk of melanoma, but anyone can have melanoma, including people with dark skin.
See the following PDQ summaries for more information on risk factors for melanoma:
Don’t Miss: What Is Braf Testing In Melanoma
There Are Three Ways That Cancer Spreads In The Body
Cancer can spread through tissue, the lymph system, and the blood:
- Tissue. The cancer spreads from where it began by growing into nearby areas.
- Lymph system. The cancer spreads from where it began by getting into the lymph system. The cancer travels through the lymph vessels to other parts of the body.
- Blood. The cancer spreads from where it began by getting into the blood. The cancer travels through the blood vessels to other parts of the body.
Skin Color And Being Exposed To Sunlight Can Increase The Risk Of Basal Cell Carcinoma And Squamous Cell Carcinoma Of The Skin
Anything that increases your chance of getting a disease is called a risk factor. Having a risk factor does not mean that you will get cancer not having risk factors doesnt mean that you will not get cancer. Talk with your doctor if you think you may be at risk.
Risk factors for basal cell carcinoma and squamous cell carcinoma of the skin include the following:
- Being exposed to natural sunlight or artificial sunlight over long periods of time.
- Having a fair complexion, which includes the following:
- Fair skin that freckles and burns easily, does not tan, or tans poorly.
- Blue, green, or other light-colored eyes.
- Red or blond hair.
Although having a fair complexion is a risk factor for skin cancer, people of all skin colors can get skin cancer.
Older age is the main risk factor for most cancers. The chance of getting cancer increases as you get older.
Also Check: Can You Die From Basal Cell Skin Cancer
Types Of Cutaneous Malignant Melanoma
The four main types of cutaneous malignant melanoma are superficial spreading, lentigo maligna, nodular, and acral lentiginous. Other, rarer subtypes of melanoma include desmoplastic, amelanotic, spitzoid, and mucosal.
Superficial spreading melanoma accounts for approximately 70% of all melanomas. The growth of superficial spreading melanoma is biphasic. An initial radial growth phase, in which growth is confined to the epidermis, is followed by a vertical phase, during which melanocytes invade deeply into the papillary and reticular dermis. More than 60% of superficial spreading melanomas present as a thin lesion these lesions have a high cure rate and may appear in multiple shades of red, blue, gray, black, and white. This type of lesion is most likely associated with a preexisting nevus, even though approximately two thirds of melanomas overall arise without an associated nevus.
Approximately 13% of melanomas are of the lentigo maligna type. These typically are flat lesions with a long radial growth phase. Lentigo maligna is regarded as the least invasive form of melanoma. These lesions commonly arise in sun-exposed areas, particularly the face, neck, and extremities. Each lesion begins as a tan or brown macule that enlarges over years to become a darker, asymmetrical foci of pigmentation and color variegation with vertical growth. The incidence of lentigo maligna melanoma is increasing, especially in the older population.