Ductal Carcinoma In Situ Causes
Its not clear what causes ductal carcinoma in-situ . Ductal carcinoma in-situ forms when genetic mutations occur in the DNA of breast duct cells. The genetic mutations cause the cells to appear abnormal, but the cells dont yet have the ability to break out of the breast duct.
Researchers dont know exactly what triggers the abnormal cell growth that leads to ductal carcinoma in-situ . Factors that may play a part include your lifestyle, your environment and genes passed to you from your parents.
What Is Squamous Cell Carcinoma In Situ Of Vulva
- Squamous Cell Carcinoma In Situ of Vulva is a malignant condition affecting the skin or mucosal membranes of the vulva . The carcinoma may be present as a well-defined red patch it is frequently solitary, but sometimes are many in number
- The lesion may itch, ulcerate, or even bleed. The condition may be diagnosed definitively through a tissue biopsy
- Middle-aged and elderly women are at risk for the condition. The cause of Squamous Cell Carcinoma In Situ of Vulva is unknown, but it is influenced by factors such as HPV infection, poor immunity, high-risk sexual practices, etc.
- Any combination of radiation therapy and invasive procedures are used to treat Vulvar Squamous Cell Carcinoma In Situ. The prognosis depends upon early diagnosis and treatment that is administered
What Is The Prognosis For Patients Who Have Ductal Carcinoma In Situ
Because DCIS is contained within a specific area of the breast and has not spread, the disease can be controlled and cured with appropriate treatment. After treatment, the outcome for the patient with DCIS is usually excellent.
However, those patients who have had DCIS, even if treated successfully, are at a greater risk than people who have never had breast cancer to have the cancer return or for another type of breast cancer to develop.
Recommended Reading: How Long Does It Take Melanoma To Metastasize
How Is Cervical Cis Diagnosed
A Pap smear can collect abnormal cells that are then identified in a lab. An HPV test may be performed on the sample to check for the virus and to see whether high-risk or low-risk strains are present.
A colposcopy is an in-office procedure that allows your doctor to view your cervix with a special magnifying tool called a colposcope. Your doctor will apply a solution to the surface of your cervix to show any abnormal cells. They can then take a small piece of tissue called a biopsy. Theyll send this to a lab for a more definitive diagnosis.
If the biopsy shows CIS, your doctor might want to remove a larger piece of your cervix. If they remove the area with abnormal cells, theyll also remove a surrounding margin of healthy tissue.
The treatment for cervical CIS is similar to that for cervical dysplasia. Although its called carcinoma in situ, its often treated like a precancerous growth because its not invasive.
Possible treatments include the following:
Talk with your doctor about your treatment options to find the best one for you. Your treatment will depend on your age, desire to preserve your fertility, general health, and other risk factors.
What Are The Signs And Symptoms Of Squamous Cell Carcinoma In Situ Of Vulva
Squamous Cell Carcinoma In Situ of Vulva signs and symptoms may include:
- The presence of a single patch-like red lesion on the vulva that is poorly-defined they may be many in number, in some cases
- Itching sensation may be felt around the red patch
- They may or may not ulcerate and bleed
- Crusting of the lesions can occur
- In squamous cell carcinoma in situ, the malignancy is confined to the skin surface and no invasion or metastasis is observed
Don’t Miss: Skin Cancer Metastasis To Lymph Nodes
Moffitt Cancer Centers Approach To Squamous Cell Carcinoma
At Moffitt Cancer Center, our multispecialty team of cancer experts takes a highly individualized approach to squamous cell carcinoma treatment. We offer the latest diagnostic and treatment options, and we work closely with each patient to offer customized guidance and help ensure the best possible outcome. For instance, there are many steps a patient can take to improve his or her own squamous cell carcinoma prognosis regardless of the general survival rate such as:
- Performing self-examinations from head to toe, including parts of the body that are not regularly exposed to UV rays, at least monthly, and promptly reporting any suspicious or unusual changes in skin texture or appearance to a physician
- Seeing a physician for a professional skin cancer examination yearly
- Avoiding exposure to the suns ultraviolet rays while outdoors, preventive measures include seeking shade, wearing sunglasses and a brimmed hat, covering up with clothing and using a broad spectrum sunscreen with both UVA and UVB protection
- Never using indoor tanning beds
If youd like to learn more about the squamous cell carcinoma survival rate, the experts at Moffitt can put this information into the proper context for you and help you take appropriate steps to achieve the best possible outcome. Call or complete a new patient registration form online. We see patients with and without referrals.
Squamous Cell Carcinomas In
As squamous cell carcinoma in-situ is confined to the surface of the skin, there are various ways to remove it. Recurrence rates are high, whatever method is used, particularly in immune suppressed patients.
Observation
As the risk of invasive squamous cell carcinoma is low, it may not be necessary to remove all lesions particularly in elderly patients. Keratolytic emollients, e.g., containing urea or salicylic acid, may be sufficient to improve symptoms.
Excision
Solitary lesions can be cut out, and the defect repaired by stitching it up. Excision is often recommended if there is suspicion of invasive squamous cell carcinoma.
Superficial skin surgery
Superficial skin surgery refers to shave, curettage and electrosurgery, and is a good choice for solitary or few hyperkeratotic lesions. The lesion is sliced off or scraped out, then the base is cauterized. Dressings are applied to the open wound to encourage moist wound healing over the next few weeks.
Cryotherapy
Cryotherapy means removing a lesion by freezing it, usually with liquid nitrogen. Moderately aggressive cryotherapy is suitable for multiple, small, flat patches of squamous cell carcinomas in-situ. It leaves a permanent white mark at the site of treatment.
Fluorouracil cream
5-fluorouracil cream contains a cytotoxic agent and can be applied to multiple lesions. The cream may be applied to squamous cell carcinomas in-situ for 4 weeks, and repeated if necessary. It causes a vigorous skin reaction that may ulcerate.
Read Also: When Squamous Cell Carcinoma Spreads
Treating Squamous Cell Carcinoma Of The Skin
Treatment options for squamous cell skin cancer depend on the risk of the cancer coming back, which is based on factors like the size and location of the tumor and how the cancer cells look under a microscope, as well as if a person has a weakened immune system.
Most squamous cell skin cancers are found and treated at an early stage, when they can be removed or destroyed with local treatment methods. Small squamous cell cancers can usually be cured with these treatments. Larger squamous cell cancers are harder to treat, and fast-growing cancers have a higher risk of coming back.
In rare cases, squamous cell cancers can spread to lymph nodes or distant parts of the body. If this happens, treatments such as radiation therapy, immunotherapy, and/or chemotherapy may be needed.
What Are The Risk Factors For Squamous Cell Carcinoma In Situ Of Vulva
The following factors increase the risk of Squamous Cell Carcinoma In Situ of Vulva:
- Infection with human papilloma virus subtypes 16, 18, 31, 33, and 45,
- High-risk sexual behavior sexual promiscuity
- Weakened immune system as a result of HIV infection or AIDS, or due to administration of immunosuppressants
- Smoking
- Lack of proper hygiene
- Longstanding ulcerative lichen planus
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases ones chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
Don’t Miss: What Does Stage 3b Melanoma Mean
Ductal Carcinoma In Situ Symptoms
Ductal carcinoma in-situ doesnt typically have any signs or symptoms. However, ductal carcinoma in-situ can sometimes cause signs such as:
- A breast lump
- Bloody nipple discharge
Ductal carcinoma in-situ is usually found on a mammogram and appears as small clusters of calcifications that have irregular shapes and sizes.
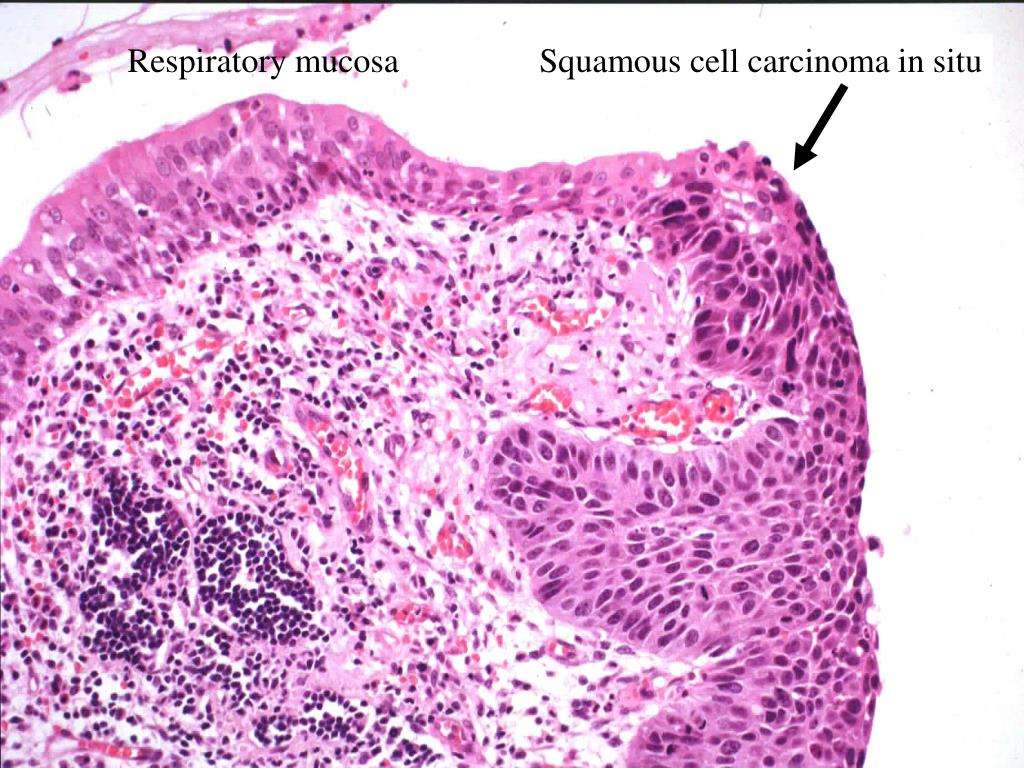
Carcinoma In Situ Cervix
In carcinoma in situ cervix is also called cervical intraepithelial neoplasia grade 3 or high-grade squamous intraepithelial lesions , the full thickness of the lining covering the cervix has abnormal cells. These abnormal cells may become cancer and spread into nearby normal tissue.
Cervical intraepithelial neoplasia grade 3 is defined by nuclear pleomorphism involving the full thickness of the squamous epithelium with mitotic activity at all levels. Cervical intraepithelial neoplasia grade 3 and severe dysplasia equates to carcinoma in situ , which term is seldom used nowadays.
Risk of progression is highest for cervical intraepithelial neoplasia grade 3 and inter-observer variation is considerably less than for CIN1 or CIN2 1). Microinvasive carcinoma is almost always seen in a background of widespread CIN3 further demonstrating its malignant potential. The exact risk is difficult to calculate because most cervical intraepithelial neoplasia grade 3 /carcinoma in situ is treated when diagnosed.
Treatment of carcinoma in situ cervix or cervical intraepithelial neoplasia grade 3 may include the following:
- Conization, such as cold-knife conization, loop electrosurgical excision procedure , or laser surgery.
- Hysterectomy for women who cannot or no longer want to have children. This is done only if the tumor cannot be completely removed by conization.
- Internal radiation therapy for women who cannot have surgery.
Figure 4. Carcinoma in situ cervix
Read Also: What Are The Forms Of Skin Cancer
Symptoms Of Bowens Disease
Bowenâs disease usually appears as a patch on the skin that has clear edges and does not heal.
Some people have more than 1 patch.
- up to a few centimetres across
- itchy
The patch can appear anywhere on the skin, but is especially common on exposed areas like the lower legs, neck and head.
Sometimes they can affect the groin area and, in men, the penis.
If the patch bleeds, starts to turn into an open sore or develops a lump, it could be a sign itâs turned into squamous cell skin cancer.
Future Directions In Dcis
DCIS research is directed mainly at improving treatment and, above all, at preventing progression to invasive disease. As researchers continue to study the pathology of DCIS, they are finding that certain tumor characteristics help predict the treatment most likely to reduce the chance of recurrence. For example, some forms of breast cancer require estrogen in order to grow tumors that do are termed estrogen receptorpositive . Tamoxifen belongs to a class of drugs called selective estrogen-receptor modulators , which act by blocking estrogen receptors. Tamoxifen is more likely to prevent a recurrence in women with ER-positive DCIS than in women with ER-negative disease.
The use of aromatase inhibitors, which block estrogen production in the peripheral tissues and breast tissue, is being investigated in a trial of postmenopausal women with ER-positive DCIS. For women whose DCIS is ER-negative but who have the HER-2/neu gene, researchers are exploring the use of trastuzumab and lapatinib , which block the tumor growth factors produced by that gene.
A new way to administer radiation that is showing some promise in clinical trials is accelerated partial breast irradiation, in which the tumor site alone is treated for five days with a lighter dose of radiation. In another approach, intraoperative radiation therapy, a one-time dose of radiation is delivered to the involved area of the breast after the tumor has been removed but before the incision is closed.
You May Like: Skin Cancer Spreading To Lymph Nodes
How Will Your Doctor Diagnose Squamous Cell Carcinoma
Your doctor will first examine the area in question, looking for things such as: the size, whether or not the borders are clearly or poorly defined, and location, including whether or not the spot is situated on top of a previous injury. The next step is a biopsy, which is the removal of tissue for examination under a microscope. If a tumor is considered to be high-risk, your doctor might order imaging scans to determine if nearby lymph nodes are involved or if the tumor has invaded other tissue in the area.
What Are The Signs And Symptoms Of Squamous Cell Carcinoma In Situ Of Anus
Squamous Cell Carcinoma In Situ of Anus signs and symptoms may include:
- The presence of a single patch-like red lesion on the anus that is poorly-defined they may be many in number, in some cases
- Itching sensation may be felt around the red patch
- They may or may not ulcerate and bleed
- Crusting of the lesions can occur
- In squamous cell carcinoma in situ, the malignancy is confined to the skin surface and no invasion or metastasis is observed
You May Like: Brain Melanoma Treatment
How Is Squamous Cell Carcinoma In Situ Of Vulva Treated
The treatment options for Squamous Cell Carcinoma In Situ of Vulva may include:
- Surgery: Complete surgical excision can be curative
- Laser ablation: The use of laser to remove solid tumors or lesions
- Radiation therapy: The use of high-energy beams to kill cancer cells
- Close monitor and follow-up reviews of the condition are important
Causes & Risk Factors Of Bowens Disease Or Squamous Cell Carcinoma In Situ
The cause of Bowens disease or Squamous Cell Carcinoma In Situ is not clear. What is clear is that this disease is not hereditary, is not infectious and does not occur from allergy.
Risk Factors of Bowens Disease or Squamous Cell Carcinoma In Situ include:
- Prolonged sun exposure, especially in fair skinned individuals however, it can also occur in those regions which have not been exposed to the sun.
- Previous treatment for a different cancer, such as radiation therapy.
- Exposure to engineering oils or arsenic can also cause Bowens disease however, this is very rare.
- Individuals who take immunosuppressant medications are at a higher risk for Bowens disease.
- Sometimes, Bowens disease can also affect the genital regions and is commonly associated with the HPV .
- Individuals aged above 60 and especially women are at an increased risk for Bowens disease.
Don’t Miss: Malignant Breast Cancer Survival Rate
Risk Factors For Ductal Carcinoma In
Factors that may increase your risk of ductal carcinoma in-situ include:
- Increasing age
- Having your first baby after age 30
- Having your first period before age 12
- Beginning menopause after age 55
- Genetic mutations that increase the risk of breast cancer, such as those in the breast cancer genes BRCA1 and BRCA2
Stage Of Cancer Carcinoma In Situ And Additional Terms
A common question is, “What stage of cancer is carcinoma in situ?” Carcinoma in situ is referred to as stage 0 cancer. At this stage, cancer is considered non-invasive. Stage 1 cancers and beyond are considered invasive, meaning that even if low, there is a potential they could spread. Other terms that may be used in defining the same thing as carcinoma in situ or stage 0 cancer include:
- Non-infiltrating
- Intra-epithelial
You May Like: Does Skin Cancer Burn And Itch
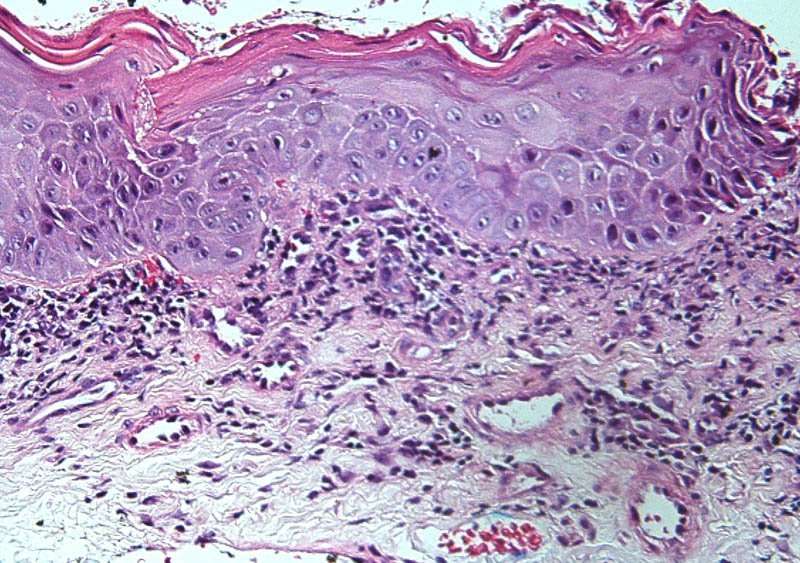
What Causes Intraepidermal Scc
Ultraviolet radiation is the main cause of intraepidermal SCC. It damages the skin cell nucleic acids , resulting in a mutantclone of the genep53, setting off uncontrolled growth of the skin cells. UV also suppresses the immune response, preventing recovery from damage.
Human papillomavirus is another major cause of intraepidermal SCC. Oncogenic strains of HPV are the main cause of squamous intraepithelial lesions , that is, squamous cell carcinoma in situ in mucosal tissue.
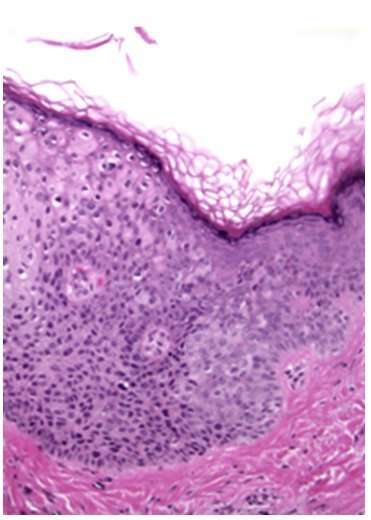
Squamous Carcinoma In Situ Of The Skin
What is squamous carcinoma in situ?
Squamous carcinoma in situ is a type of non-invasive skin cancer. The tumour starts from the cells normally found on the surface of the skin. Another name for squamous carcinoma in situ in the skin is Bowens disease. If left untreated, most tumours will eventually turn into a type of cancer called invasive squamous cell carcinoma.
What is skin?
Skin is made up of three layers: epidermis, dermis, and subcutaneous fat. The surface and the part you can see when you look at your skin is called the epidermis. The cells that make up the epidermis include squamous cells, basal cells, melanocytes, Merkel cells, and cells of the immune system. The squamous cells in the epidermis produce a material called keratin which makes the skin waterproof and strong and protects us from toxins and injuries. The dermis is directly below the epidermis. The dermis is separated from the epidermis by a thin layer of tissue called the basement membrane. The dermis contains blood vessels and nerves. Below the dermis is a layer of fat called subcutaneous adipose tissue.
What causes squamous carcinoma in situ?
Most tumours that occur in older adults develop as a result of the cells in the epidermis being damaged by UV light from the sun. Long-term exposure to UV radiation from tanning beds can cause similar damage. People who have immunosuppression due to organ transplantation or HIV infection are also at increased risk of developing squamous carcinoma in situ.
Read Also: Cure For Melanoma Stage 4
Comedo Dcis Usually Shows Small Groups Of Dead Cells
What typically happens in a breast comedo carcinoma is that some of the cells die off and form small groups. . It is a fast growing type of breast cancer with some risk of future invasive cancer status, but most of the time comedo breast carcinoma is considered to be intraductal, meaning, that it will be confined to the breast ducts. DCIS-comedo is generally diagnosed when at least one duct in the breast is filled and expanded by large, markedly atypical cells, and which also has abundant central luminal necrosis.