Small And Large Cell Cervical Cancer
Small cell cervical cancer and large cell cervical cancer make up a rare subtype of cervical cancer. They are aggressive forms of a larger group of tumors called neuroendocrine cancers. These cancers occur in the hormone-producing cells of the bodys neuroendocrine system, which is composed of cells that are a cross between endocrine cells and nerve cells.
Of the 11,000 new cases of cervical cancer diagnosed in the United States each year, approximately 100 cases will be small cell or large cell cervical cancer. Unlike other types of cervical cancer, SCCC and LCCC have no definitive link to the human papilloma virus . Because these tumors are so rare, the cause is not yet fully understood.
Small cell and large cell cervical cancers are the most common type of neuroendocrine tumor in the cervix, but still accounts for less than 1% of all cervical cancers.
What Are The Risk Factors For Small Cell Neuroendocrine Carcinoma Of Pancreas
The specific risk factors for Small Cell Neuroendocrine Carcinoma of Pancreas are not well characterized, due to the rarity of this condition. However, in general, the risk factors for pancreatic cancer include:
- Advancing age
- A family history of pancreatic cancer
- Family history of breast cancer
- Certain genetic syndromes, such as the following:
- Multiple endocrine neoplasia type 1 , caused by genetic mutations in the MEN1 gene. This condition may increase the risk of tumors in the parathyroid gland, the pituitary gland, and the islet cells of the pancreas
- Neurofibromatosis, type 1, caused by genetic mutations in the NF1 gene. This syndrome may lead to an increased risk of developing many different types of tumors, such as somatostatinomas
- Von Hippel-Lindau syndrome, which occurs owing to genetic mutations in the VHL gene. This syndrome may lead to an increased risk of pancreatic cancer and ampullary carcinoma
- Tuberous sclerosis complex : It occurs as a result of mutations in the TSC1 and TSC2 genes. This inherited condition predisposes an affected individual to three different types of lesions in the brain, as well as other organs of the body
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What Are The Signs And Symptoms Of Small Cell Neuroendocrine Carcinoma Of Pancreas
The symptoms of Small Cell Neuroendocrine Carcinoma of Pancreas depend on a number of factors such as:
- Size of the tumor
- Histological type of the tumor
- Whether the tumor produces hormones
- Local spread of the tumor
- Rupture of the cystic mass
- Extent of bleeding within the tumor
- Whether the tumor is present as part of a syndrome, in which case, the signs and symptoms associated with the accompanying syndrome may be noted
Typically, the signs and symptoms of Small Cell Neuroendocrine Carcinoma of Pancreas do not occur until later stages of the disease. The type and severity of symptoms may vary among the affected individuals, and the symptoms include:
- Anorexia
Some other features of Small Cell Neuroendocrine Carcinoma of Pancreas include:
- The tumor may present as a single mass or multiple nodules within the organ
- If there is cyst formation, it may occasionally rupture, spilling its contents into the belly
- These tumors are aggressive, and may spread to local areas
Read Also: What Does Melanoma In Situ Look Like
Large Cell And Small Cell Tumors
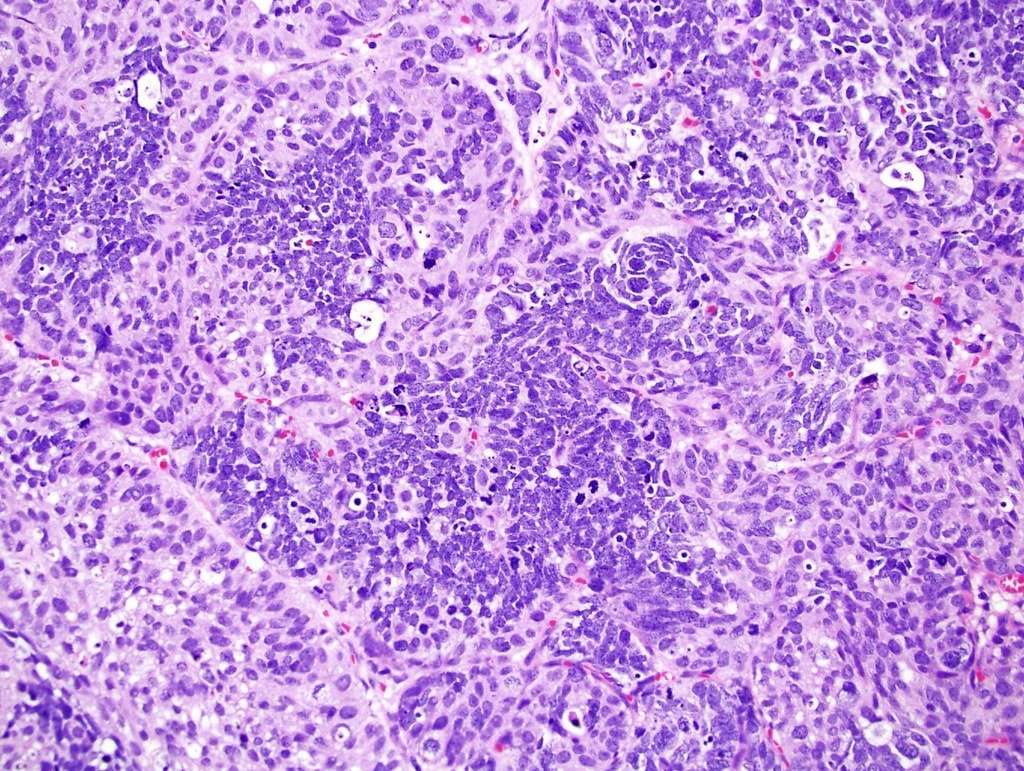
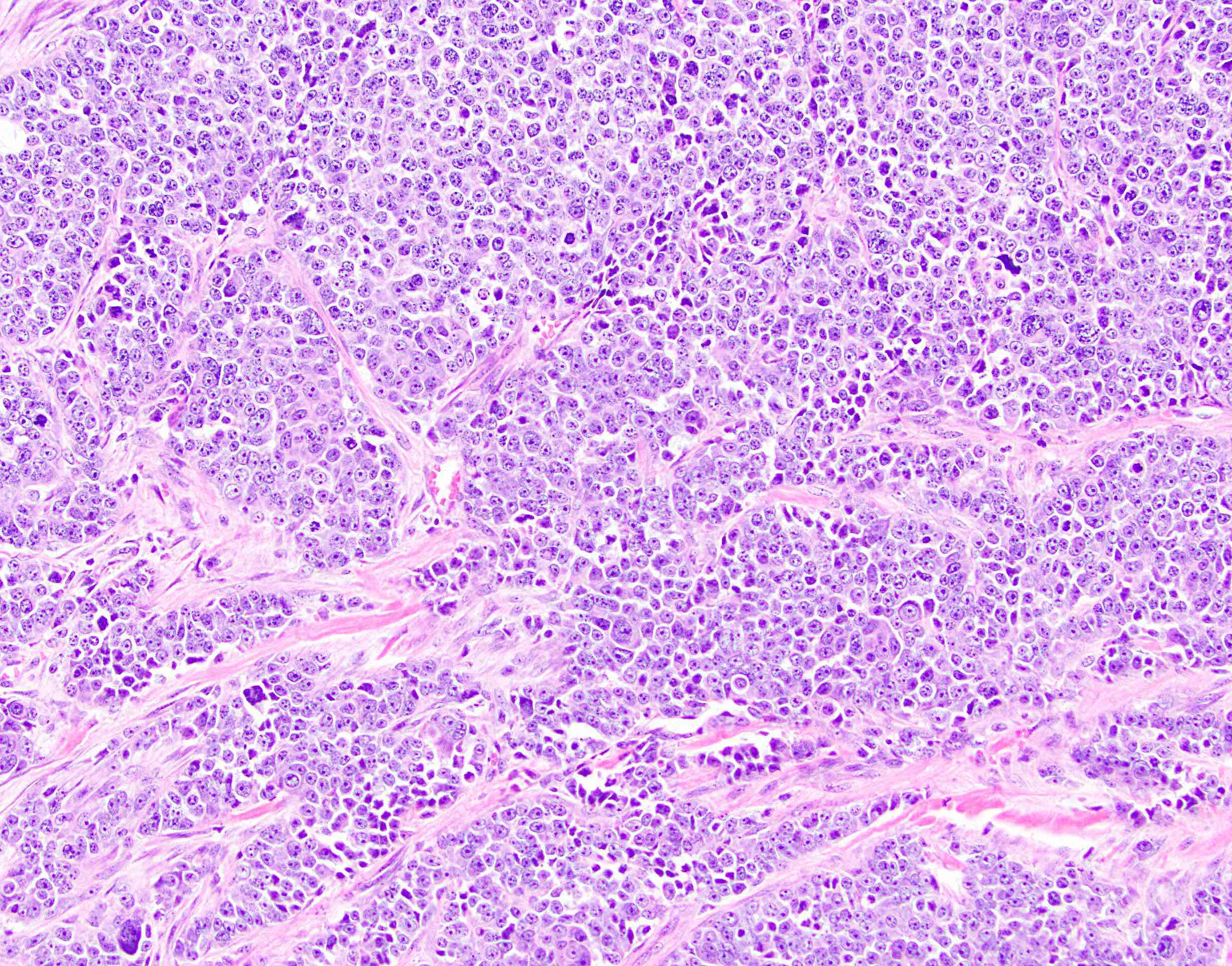
High-grade or aggressive neuroendocrine tumors are divided into a large cell and small cell tumors, which differ based on the appearance of the cells under a microscope. Both types of cancer are considered highly undifferentiated, which essentially means that the cells appear very primitive relative to normal neuroendocrine cells and behave very aggressively.
In some ways, high-grade neuroendocrine tumors are similar to small cell lung cancer, and often respond to similar treatments, but are less likely to be associated with smoking than small cell lung cancers and are less likely to have metastases to bones and the brain.
Some studies have found that the tumors occur more commonly on the right side of the colon whereas a recent study found that the most common location for these tumors was the rectum and sigmoid colon.
Colon cancer screening hasnt led to a significant increase in the prognosis of these tumors.
How Is Small Cell Neuroendocrine Carcinoma Of Esophagus Treated
There are no well-established treatment protocols for Small Cell Neuroendocrine Carcinoma of Esophagus. However, surgery is the preferred treatment modality for esophageal neuroendocrine carcinomas . The treatment may also include a combination of radiation therapy and chemotherapy.
- When the tumor is confined to the surface, then endoscopic mucosal/submucosal resection is undertaken. Tumors less than 1.5 cm size may be removed through endoscopic resection
- Esophagectomy or surgery to remove part of esophagus
- If the tumor has metastasized, then a combination of chemotherapy, radiation therapy, and invasive procedures may be used to treat the tumor
- In some cases, neoadjuvant therapy is considered prior to surgery
- Palliative care is provided for advanced cancer stages
- Follow-up care with regular screening and check-ups are very important and encouraged
Read Also: Melanoma Forearm
What Are The Causes Of Small Cell Neuroendocrine Carcinoma Of Esophagus
The exact cause of development of Small Cell Neuroendocrine Carcinoma of Esophagus is unknown.
- In general, it is known that cancers form when normal, healthy cells begin transforming into abnormal cells – these cancer cells grow and divide uncontrollably , resulting in the formation of a mass or a tumor
- Many cancer types are caused by genetic mutations. These can occur, due to inherited mutations, or mutations that occur due to environmental factors
- The transformation of normally healthy cells into cancerous cells may be the result of genetic mutations. Mutations allow the cancer cells to grow and multiply uncontrollably to form new cancer cells
- These tumors can invade nearby tissues and adjoining body organs, and even metastasize and spread to other regions of the body
An Extremely Rare Case Of Advanced Metastatic Small Cell Neuroendocrine Carcinoma Of Sinonasal Tract
Yu Yu Thar
1Department of Medicine, Division of Hematology and Oncology, The Brooklyn Hospital Center, Brooklyn, NY 11201, USA
2Department of Medicine, The Brooklyn Hospital Center, Brooklyn, NY 11201, USA
3Department of Pathology, The Brooklyn Hospital Center, Brooklyn, NY 11201, USA
Academic Editor:
Abstract
Small cell neuroendocrine carcinoma is a rare form of malignancy. It mainly presents as bronchogenic neoplasm, and the extrapulmonary form accounts for only 0.1% to 0.4% of all cancers. These extrapulmonary tumors have been described most frequently in the urinary bladder, prostate, esophagus, stomach, colon and rectum, gall bladder, head and neck, cervix, and skin. Primary SNEC of the sinonasal tract is extremely rare with only less than 100 cases reported in the literature. Because of extreme rarity and aggressiveness of the tumor, the management for this entity varies considerably mandating multimodality approach. In this paper, we report a patient presented with left-sided facial swelling, and the histopathologic examination confirmed primary SNEC of left sinonasal tract. The tumor involved multiple paranasal sinuses with invasion into the left orbit and left infratemporal fossa and metastasized to cervical lymph nodes and bone. The patient encountered devastating outcome in spite of optimal medical management and treatment with palliative chemotherapy highlighting the necessity for further research of primary SNEC of head and neck.
1. Introduction
Don’t Miss: Clear Cell Carcinoma Symptoms
The Importance Of Immediate Chemotherapy And Locoregional Control
The mainstay of therapy for small-cell prostate carcinomas is combination chemotherapy. In general, the duration of response is short, but it frequently provides marked palliation of symptoms and occasionally results in durable remissions. Multiple case reports and series have described the response of small-cell prostate carcinomas to various chemotherapy combinations, but only two prospective, single-arm clinical trials of this disease entity have been published.
In the first trial, the goal was to explore the hypothesis that the combination of doxorubicin, etoposide, and cisplatin would improve the response rate of these cancers over what had been observed historically with etoposide and cisplatin alone. Of the 36 patients who were assessable for response, 22 achieved a partial response in measurable disease. Notably, 21 of 25 symptomatic patients experienced pain reduction, with a concomitant decrease in their daily opioid analgesic requirement. Median time to progression and overall survival were 5.8 months and 10.5 months , respectively. However, toxicity was significant, and the authors concluded that the addition of doxorubicin to etoposide and cisplatin was not an improvement.
How Is Small Cell Neuroendocrine Carcinoma Of Pancreas Treated
The treatment methods for detect Small Cell Neuroendocrine Carcinoma of Pancreas are determined by several factors, such as, how advanced the cancer is, the overall health of the affected individual, as well as his/her personal preference. These cancers are extremely aggressive. The healthcare provider determines and plans the best course of treatment on a case-by-case basis.
Once the extent of cancer has been determined, the following treatment methods may be employed:
- A debulking surgery to reduce the tumor mass
- The debulking procedure helps the chemotherapy treatment in being more effective, since there is lesser tumor mass left for the drugs to act on
Surgery for tumors located in the pancreatic head: Pancreatoduodenectomy
- A surgical procedure that involves the removal of part of the pancreas, part of the small intestine, and the gallbladder
- This procedure is typically used when the tumor is confined to the head of the pancreas
- The technique is also known as a Whipple procedure
Surgery for tumors in the pancreatic tail and body of the pancreas: Distal pancreatectomy
- A surgical procedure that involves the removal of the lower half or tail end of the pancreas
- Post-operative care is important: A minimal physical activity is advised, until the surgical wound heals
Chemotherapy: It may be administered before or after the debulking procedure, depending on the individuals specific circumstances.
Radiation therapy:
Don’t Miss: Immunotherapy For Malignant Melanoma
Is Stage 4 Neuroendocrine Cancer Curable
Neuroendocrine cancer/tumor starts in the neuroendocrine cells in your body. These cells have features of both the type of cells- endocrine cells and nerve cells. Most of these tumors are benign while some are malignant. These can occur anywhere in the body where neuroendocrine cells are present, but most commonly they are seen in the intestine.
New Molecular Classification Of Large Cell Neuroendocrine Carcinoma And Small Cell Lung Carcinoma With Potential Therapeutic Impacts
Sylvie Lantuejoul1,2, Lynnette Fernandez-Cuesta3, Francesca Damiola1, Nicolas Girard4, Anne McLeer2,5
1Department of Biopathology, Pathology Research Platform- Synergie Lyon Cancer- CRCL, Centre Léon Bérard Unicancer International Agency for Research on Cancer , Institut du Thorax Curie Montsouris , 5Department of Pathology and Cancer Molecular Genetics Platform, CHU Grenoble Alpes, Grenoble , France
Contributions: Conception and design: All authors Administrative support: All authors Provision of study materials or patients: All authors Collection and assembly of data: All authors Data analysis and interpretation: All authors Manuscript writing: All authors Final approval of manuscript: All authors.
Correspondence to:
Keywords: Lung cancer neuroendocrine high-grade molecular classification
Submitted Feb 16, 2020. Accepted for publication May 12, 2020.
doi: 10.21037/tlcr-20-269
Read Also: What Is The Survival Rate Of Invasive Ductal Carcinoma
What Is The Survival Rate For Neuroendocrine Cancer
The 5-year survival rate for people with a GI tract NET that has not spread to other parts of the body from where it started is 97%. If the tumor has spread to nearby tissue or the regional lymph nodes, the 5-year survival rate is 95%. If the tumor has spread to distant areas of the body, the survival rate is 67%.
What Is Small Cell Neuroendocrine Carcinoma Of Esophagus
- Small Cell Neuroendocrine Carcinoma of Esophagus is high-grade neuroendocrine carcinoma of esophagus that is extremely rare. The esophagus is a part of the upper gastrointestinal tract and is also known as the food-pipe
- Esophageal neoplasms with neuroendocrine differentiation include low, intermediate, and high- grade tumors and carcinomas. These are extremely rare and malignant
- Neuroendocrine carcinomas of esophagus are poorly-differentiated high-grade tumors that are histologically graded G3. NECs are highly-aggressive, show deep penetration into the walls, and are found in advanced stages. They used to be called carcinoid tumors
- High-grade neuroendocrine carcinomas are of 3 types
- Small Cell Neuroendocrine Carcinoma of Esophagus
- Large cell neuroendocrine carcinoma of esophagus
- Mixed adenoneuroendocrine carcinoma of esophagus
You May Like: Invasive Ductal Breast Cancer Survival Rate
Collision Carcinoma Involving Small Cell Neuroendocrine Carcinoma And Squamous Cell Carcinoma Of The Ureter: A Case Report And Review Of The Literature
- 1Department of Urology, The Second Affiliated Hospital of Hainan Medical University, Haikou, China
- 2Department of Pathology, The Second Affiliated Hospital of Hainan Medical University, Haikou, China
Background: Small cell neuroendocrine carcinoma of the ureter is a rare tumour, accounting for less than 0.5% of all ureteral tumours. SCNEC tumours are highly aggressive and patients have a poor prognosis. Ureteral SCNEC colliding with other pathological types of tumours is extremely rare. In this paper, we present the case of a patient with ureteral small cell carcinoma colliding with squamous cell carcinoma and review the literature regarding the clinicopathological features, treatment and prognosis of thus tumour. To the best of our knowledge, this is the second identified case of ureteral SCNEC colliding with SCC.
Case Presentation: A 64-year-old male patient presented with a history of 1 month of gross haematuria and 3 months of left flank pain. CT urography revealed a soft tissue mass in the upper ureter, which was slightly enhanced on contrast-enhanced CT. Nephroureterectomy was performed after the patient was diagnosed with a tumour in the left ureter. Microscopy and immunohistochemical examination confirmed the mass to be a SCNEC collision with SCC. Two months after the surgery, the patient received adjuvant chemotherapy . After 14 months of follow-up, no local recurrence or distant metastasis was found.
How Is Small Cell Neuroendocrine Carcinoma Of Esophagus Diagnosed
A diagnosis of Small Cell Neuroendocrine Carcinoma of Esophagus may involve the following:
- A thorough medical history and physical examination
- X-ray of the chest
- Multi-phasic CT or MRI scan of the chest: For advanced cases and to check cancer growth and spread, including lymph node involvement
- Upper GI endoscopy: An endoscopic procedure is performed using an instrument called an endoscope, which consists of a thin tube and a camera. Using this technique, the radiologist can have a thorough examination of the insides of the upper gastrointestinal tract
- Endoscopic ultrasonography: During this procedure, fine needle aspiration biopsy can be performed on the affected area. This is good technique for tumor detection including tumor invasion parameters, and whether nearby lymph nodes are affected
- Endocytoscopy: It is a non-invasive technique helpful for invasive carcinomas that are located superficially
- Early cancer lesions may be detected using narrow band imaging technique
- Barium swallow
- Whole body PET scans to determine how far the cancer has spread to other organ systems
Although the above modalities can be used to make an initial diagnosis, a tissue biopsy of the tumor is necessary to make a definitive diagnosis to begin treatment. The tissue for diagnosis can be procured in multiple different ways which include:
Tissue biopsy:
Note:
You May Like: Stage Iiia Melanoma Prognosis
What Is The Prognosis Of Small Cell Neuroendocrine Carcinoma Of Esophagus
- The prognosis of Small Cell Neuroendocrine Carcinoma of Esophagus is generally poor. In general, the survival period following the diagnosis of a neuroendocrine carcinoma is about or less than 6 months
- Individuals with locally-confined disease , are known to do better than those with distant spread of the cancer
- In general, the prognosis of the tumor depends upon a set of several factors, which include:
- Stage of tumor: With lower-stage tumors, when the tumor is confined to site of origin, the prognosis is usually excellent with appropriate therapy. In higher-stage tumors, such as tumors with metastasis, the prognosis is poor
- Overall health of the individual: Individuals with overall excellent health have better prognosis compared with those with poor health
- Age of the individual: Older individuals generally have poorer prognosis than younger individuals
- The size of the tumor: Individuals with small-sized tumors fare better than those with large-sized tumors
- Individuals with bulky disease may have a poorer prognosis
- Involvement of vital organs may complicate the condition
- The surgical resectability of the tumor
- Whether the tumor is occurring for the first time, or is a recurrent tumor. Recurring tumors have worse prognosis compared to tumors that do not recur
- Response to treatment: Tumors that respond to treatment have better prognosis compared to tumors that do not respond to treatment
- Progression of the condition makes the outcome worse
Cellular Pathways Affected In Sclc
Although SCLC tumours are highly metastatic, how cell adhesion and cell migration are affected by the genetic and transcriptional changes in SCLC cells is not completely understood. It is possible that the migration potential of SCLC cells is inherently related to the striking migratory phenotypes of neuroendocrine cells during lung development. Interactions between laminin and fibro nectin in the extracellular matrix and adhesion molecules, such as integrins, have been associated with survival and resistance to therapy. Similarly, high levels of CXCR4, a receptor for the chemokine stromal cell-derived factor 1 , promote the migration and survival of SCLC cells. Interestingly, 31 integrin-mediated adhesion stimulates the growth of axon-like protrusions on SCLC cells, which might promote cell migration by mechanisms similar to those observed in the migration of neuronal progenitors during brain development. The epithelial-to-mesenchymal transition has been implicated in the resistance to treatment in SCLC,, but has not been explored as a driver of cell migration. The interplay between adhesion, migration, survival and proliferation may be relevant to the strong metastatic potential of SCLC cells.
You May Like: Invasive Ductal Carcinoma Stage 2 Survival Rate