Cancerous Tumours Of The Bladder
A cancerous tumour of the bladder can grow into nearby tissue and destroy it. It can also spread to other parts of the body. Cancerous tumours are also called malignant tumours.
Bladder cancer is often divided into 3 groups based on how much it has grown into the bladder wall.
- Non-invasive bladder cancer is only in the inner lining of the bladder .
- Nonâmuscle-invasive bladder cancer has only grown into the connective tissue layer .
- Muscle-invasive bladder cancer has grown into the muscles deep within the bladder wall and sometimes into the fat that surrounds the bladder.
Ajcc Stage Groupings And Tnm Definitions
The American Joint Committee on Cancer has designated staging by TNM classification to define bladder cancer.
| Stage |
|---|
| Poorly differentiated. |
References
What Is An Urothelial Neoplasm
Urothelial neoplasia is a unique cancer in that is consists of a spectrum of tumors with different biologic behaviors. The most common urothelial neoplasm is the low grade superficial papillary carcinoma or papilloma which may recur numerous times but does not result in significant morbidity or mortality.
Don’t Miss: What Are The Early Stages Of Skin Cancer
Papillary Vs Flat Cancer
Bladder cancers are also divided into 2 subtypes, papillary and flat, based on how they grow .
- Papillary carcinomas grow in slender, finger-like projections from the inner surface of the bladder toward the hollow center. Papillary tumors often grow toward the center of the bladder without growing into the deeper bladder layers. These tumors are called non-invasive papillary cancers. Very low-grade , non-invasive papillary cancer is sometimes called papillary urothelial neoplasm of low-malignant potential and tends to have a very good outcome.
- Flat carcinomas do not grow toward the hollow part of the bladder at all. If a flat tumor is only in the inner layer of bladder cells, itâs known as a non-invasive flat carcinoma or a flat carcinoma in situ .
If either a papillary or flat tumor grows into deeper layers of the bladder, itâs called an invasive urothelial carcinoma.
Donât Miss: What Is Papillary Urothelial Carcinoma
Cellular Classification Of Bladder Cancer
More than 90% of bladder cancers are transitional cell carcinomas derived from the uroepithelium. About 2% to 7% are squamous cell carcinomas, and 2% are adenocarcinomas. Adenocarcinomas may be of urachal origin or nonurachal origin the latter type is generally thought to arise from metaplasia of chronically irritated transitional epithelium. Small cell carcinomas also may develop in the bladder. Sarcomas of the bladder are very rare.
Pathologic grade of transitional cell carcinomas, which is based on cellular atypia, nuclear abnormalities, and the number of mitotic figures, is of great prognostic importance.
References
Don’t Miss: What Are The Symptoms Of Basal Cell Carcinoma
Low Grade And High Grade
Bladder cancer can also be described as either low grade or high grade.
Low grade bladder cancer means that your cancer is less likely to grow, spread and come back after treatment. High grade means your cancer is more likely to grow spread and come back after treatment.
For example, if you have early bladder cancer but the cells are high grade, youâre more likely to need further treatment after surgery. This is to reduce the risk of your cancer coming back.
Low grade is the same as grade 1. High grade is the same as grade 3. Grade 2 can be split into either low or high grade. Carcinoma in situ tumours are high grade.
You May Like: How Deadly Is Squamous Cell Carcinoma
Superficial Bladder Cancer Or Non
Bladder cancers are called superficial, or non-invasive, if they stay confined to the bladder tissue in which they began. For example, Urothelial cancer is considered superficial bladder cancer if it has not spread anywhere outside of the bladder lining. Typically, non-invasive cancers are easier to treat and less likely to recur.
Other helpful information about superficial bladder cancer includes:
- Superficial bladder cancer is an early-stage disease that affects the bladder lining only.
- Small, finger-like growths project from the inside surface of the bladder towards its hollow center. This is called papillary bladder cancer. These growths can be removed quite easily by your surgeon, and they may never come back .
- Some types of early-stage bladder cancer are more likely to recur. These include carcinoma in situ and high-grade T1 tumors.
Types of tumors and their treatment include:
Also Check: What Does Skin Cancer On Your Lip Look Like
Invasion Into The Lamina Propria
Urinary Bladder Tumour, Transurethral Resection: - INVASIVE HIGH-GRADE PAPILLARY UROTHELIAL CARCINOMA with lamina propria invasion.-- Muscularis propria present, NEGATIVE for muscularis propria invasion.-- NEGATIVE for lymphovascular invasion.-- Please see synoptic report.
Block letters
URINARY BLADDER LESION , TRANSURETHRAL RESECTION URINARY BLADDER TUMOUR : - INVASIVE HIGH-GRADE PAPILLARY UROTHELIAL CARCINOMA WITH LAMINA PROPRIA INVASION.- MUSCULARIS PROPRIA NEGATIVE FOR INVASIVE MALIGNANCY.- NEGATIVE FOR LYMPHOVASCULAR INVASION.
Recommended Reading: What Is Stage 4 Melanoma Cancer
Start And Spread Of Bladder Cancer
The wall of the bladder has many several layers. Each layer is made up of different kinds of cells .
Most bladder cancers start in the innermost lining of the bladder, which is called the urothelium or transitional epithelium. As the cancer grows into or through the other layers in the bladder wall, it has a higher stage, becomes more advanced, and can be harder to treat.
Over time, the cancer might grow outside the bladder and into nearby structures. It might spread to nearby lymph nodes, or to other parts of the body.
You May Like: What Is Infiltrating Ductal Carcinoma
Cystectomy Cystoprostatectomy And Pelvic Exenteration Specimens
Processing of these specimens may be summarized in three steps: orientation of the specimen and identification of relevant anatomic structures , fixation of the specimen and dissection of the specimen. Peritoneum covering the surface of the bladder is a reliable anatomic landmark. In both male and female patients, the peritoneum descends further along the posterior wall of the bladder than it does along the anterior wall. Other pelvic organs, if present, may also be used to orient the specimen. In the male, the bladder adjoins the rectum and seminal vesicles posteriorly, the prostate inferiorly, and the pubis and peritoneum anteriorly. In the female, the vagina is located posteriorly, and the uterus is located superiorly. Once the specimen is oriented, both ureters and, when present, the vasa deferentia should be identified. Location and dissection of the ureters is easier after fixation. The outer dimensions of the urinary bladder, as well as the length and diameter of ureters, should be recorded. The external surface of the bladder should be inked.
The minimum number of sections to be taken are as follows: tumor bladder neck , trigone , anterior wall , posterior wall , lateral walls , dome , ureteral orifices , margins , any abnormal appearing bladder mucosa and any perivesical lymph nodes .
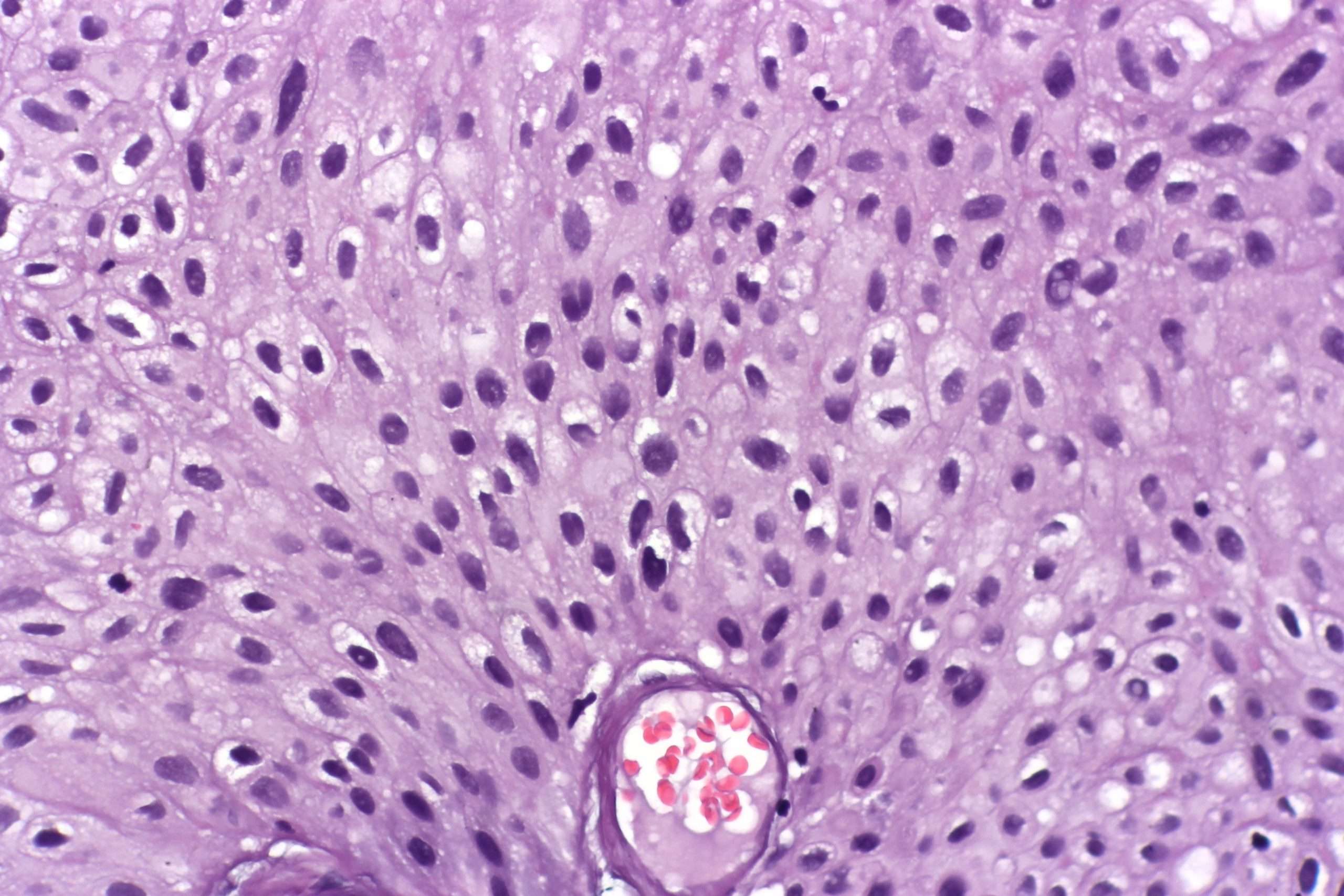
Figure 18
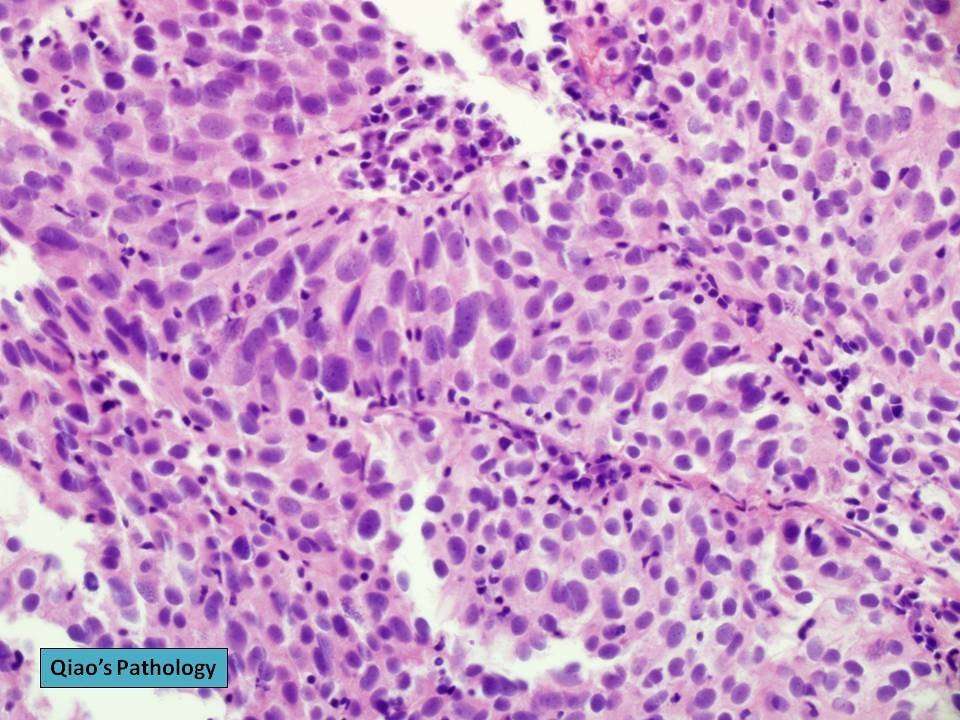
Morphologic Variants Of Urothelial Carcinoma
Some cases of urothelial carcinoma show morphologic patterns that are recognized as variants morphology. Those include nested variant, micropapillary, lymphoepithelioma-like, sarcomatoid, small cell carcinoma, and adenocarcinoma. These are frequently under-recognized in bladder biopsies and could have therapeutic implications with different criteria for surgery and different chemotherapy regimens.
Don’t Miss: What Do Melanoma Spots Look Like
Treating Stage 0 Bladder Cancer
Stage 0 bladder cancer includes non-invasive papillary carcinoma and flat non-invasive carcinoma . In either case, the cancer is only in the inner lining layer of the bladder. It has not invaded the bladder wall.
This early stage of bladder cancer is most often treated with transurethral resection with fulguration followed by intravesical therapy within 24 hours.
What Is The Prognosis For Someone With Prcc
The estimate of how a disease will affect you long-term is called prognosis. Every person is different and prognosis will depend on many factors, such as
- Where the tumor is in your body
- If the cancer has spread to other parts of your body
- How much of the tumor was taken out during surgery
If you want information on your prognosis, it is important to talk to your doctor. NCI also has resources to help you understand cancer prognosis.
Doctors estimate survival rates by how groups of people with PRCC have done in the past. Because there are so few people with PRCC, these rates may not be very accurate. They also cant consider newer treatments being developed.
In general, type 2 papillary renal cell carcinoma has a poorer prognosis than type 1.
Related Resources
Also Check: How Often Does Squamous Cell Carcinoma Spread
What Is Bladder Cancer
Bladder cancer starts when cells that make up the urinary bladder start to grow out of control. As more cancer cells develop, they can form a tumor and, with time, spread to other parts of the body.
The bladder is a hollow organ in the lower pelvis. It has flexible, muscular walls that can stretch to hold urine and squeeze to send it out of the body. The bladder’s main job is to store urine. Urine is liquid waste made by the 2 kidneys and then carried to the bladder through 2 tubes called ureters. When you urinate, the muscles in the bladder contract, and urine is forced out of the bladder through a tube called the urethra.
What Is Urothelial Carcinoma
Urothelial Carcinoma is a multifocal malignancy associated with the reno-urinary system. Renal parenchyma often develops a high-grade scirrhous mass formation and turns to a malignant tumor. In urothelial carcinoma, the organ which can get affected with malignant attacks is renal pelvis, ureters, and bladder. The possibility of this organ get affected with Urothelial Carcinoma can be estimated as 1:3:50 respectively.
It has been observed that upper urinary tract cancer affected patients have a 30 to 50 percent tendency to develop bladder cancer, whereas bladder cancer affected individuals also has a 2 to 3 percent tendency to develop urinary tract cancer. Therefore, the reno-urinary system is interconnected and the scope of cancer progression also inter-related1,2.
You May Like: What Is The Life Expectancy Of Someone With Metastatic Melanoma
Stage Iv Bladder Cancer Treatment
Only a small fraction of patients with stage IV bladder cancer can be cured, and for many patients, the emphasis is on palliation of symptoms. The potential for cure is restricted to patients with stage IV disease with involvement of pelvic organs by direct extension or metastases to regional lymph nodes.
How Will My Doctor Test For It
Youll need a few different tests to see if a nodule is cancer.
Physical exam. Your doctor will feel for unusual growths in your neck and ask about any symptoms you might have.
Blood tests. You may get your thyroid hormone levels checked. This wont tell you if you have cancer, but it gives more information about how your thyroid is working.
Ultrasound. Youll get this test, which uses sound waves to make a picture of things inside your body, to learn more about nodules you have. Your doctor will find out about their shape, size, and other features. That will give important clues to decide how much of a problem they are.
Biopsy. Your doctor will use a very fine needle to take a sample of the nodule to test for cancer. Typically, the most youll feel during it is a small pinch.
Youll likely get this done for any nodule thats bigger than 1 centimeter . Nodules with calcium buildup, lots of blood vessels, or without clear borders raise red flags. So do unusual-looking nearby lymph nodes bean-shaped organs that help fight infections.
Read Also: How To Remove Skin Cancer Yourself
Also Check: What Causes Renal Cell Carcinoma Cancer
Urothelial Tumors Of The Urinary Bladder In Young Patients: A Clinicopathologic Study Of 59 Cases
Melissa L. Stanton, Li Xiao, Bogdan A. Czerniak, Charles C. Guo Urothelial Tumors of the Urinary Bladder in Young Patients: A Clinicopathologic Study of 59 Cases. Arch Pathol Lab Med 1 October 2013 137 : 13371341. doi:
Context.Urothelial tumors are rare in young patients. Because of their rarity, the natural history of the disease in young patients remains poorly understood.
Objective.To understand the pathologic and clinical features of urothelial tumors of the urinary bladder in young patients.
Design.We identified 59 young patients with urothelial tumors of the urinary bladder treated at our institution and analyzed the tumors’ pathologic features and the patients’ clinical outcomes.
.Urothelial tumors in young patients are mostly noninvasive, papillary carcinomas and have an excellent prognosis however, a small subset of patients may present with high-grade invasive urothelial carcinomas that result in poor clinical outcomes.
Prognosis And Life Expectancy
In general, papillary urothelial cancers have a better prognosis than other types of bladder cancer. Your specific outlook depends on the stage and grade of your cancer. High-grade cancers can spread. Low-grade papillary cancers are less likely to spread. Papillary cancers can also return after theyve been treated.
Read Also: What Is Merkel Cell Skin Cancer
Standard Treatment Options For Stage I Bladder Cancer
Patients with stage I bladder tumors are unlikely to die from bladder cancer, but the tendency for new tumor formation is high. In a series of patients with Ta or T1 tumors who were followed for a minimum of 20 years or until death, the risk of bladder recurrence after initial resection was 80%. Of greater concern than recurrence is the risk of progression to muscle-invasive, locally-advanced, or metastatic bladder cancer. While progression is rare for low-grade tumors, it is common among high-grade cancers.
One series of 125 patients with TaG3 cancers followed for 15 to 20 years reported that 39% progressed to more advanced stage disease, while 26% died of urothelial cancer. In comparison, among 23 patients with TaG1 tumors, none died and 5% progressed. Risk factors for recurrence and progression include the following:
- High-grade disease.
TUR with fulguration followed by an immediate postoperative instillation of intravesical chemotherapy
TUR and fulguration are the most common and conservative forms of management. Careful surveillance of subsequent bladder tumor progression is important. Because most bladder cancers recur after TUR, one immediate intravesical instillation of chemotherapy after TUR is widely used. Numerous randomized, controlled trials have evaluated this practice, and a meta-analysis of seven trials reported that a single intravesical treatment with chemotherapy reduced the odds of recurrence by 39% .
TUR with fulguration
Evidence :
Standard Treatment Options For Stages Ii And Iii Bladder Cancer
The most common treatments for muscle-invasive bladder cancer are radical cystectomy and radiation therapy. There is no strong evidence from randomized controlled trials to determine whether surgery or radiation therapy is more effective. There is strong evidence that both therapies become more effective when combined with chemotherapy. The treatments with the highest level of evidence supporting their effectiveness are radical cystectomy preceded by multiagent cisplatin-based chemotherapy and radiation therapy with concomitant chemotherapy.
Radical cystectomy
Radical cystectomy is a standard treatment option for stage II and stage III bladder cancer, and its effectiveness at prolonging survival increases if it is preceded by cisplatin-based multiagent chemotherapy. Radical cystectomy is accompanied by pelvic lymph node dissection and includes removal of the bladder, perivesical tissues, prostate, and seminal vesicles in men and removal of the uterus, fallopian tubes, ovaries, anterior vaginal wall, and urethra in women. Studies of outcomes after radical cystectomy report increased survival in patients who had more, rather than fewer, lymph nodes resected whether this represents a therapeutic benefit of resecting additional nodes or stage migration is unknown. There are no randomized controlled trials evaluating the therapeutic benefit of lymph node dissection in this setting.
Evidence :
Evidence :
Segmental cystectomy
Read Also: What Is Pigmented Basal Cell Carcinoma
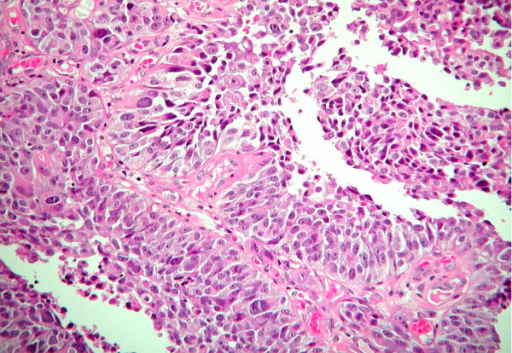
Sarcomatoid Carcinoma Of The Urinary Bladder
The sarcomatoid areas may merge with foci of urothelial carcinoma , squamous cell carcinoma, adenocarcinoma or small-cell carcinoma, and most commonly resemble a high-grade sarcoma, not otherwise specified, or have a malignant fibrous histiocytoma histology. Heterologous differentiation may be present but has no definite prognostic significance . In decreasing order of frequency, areas of osteosarcoma, chondrosarcoma, rhabdomyosarcoma, liposarcoma, angiosarcoma or a mixture of sarcoma histologies may be seen. In the absence of an obvious invasive carcinoma , in a primarily malignant spindle cell tumor of the bladder, history of prior urothelial neoplasia, coexistence of in situ disease such as urothelial carcinoma in situ or strong and relatively diffuse cytokeratin immunoreactivity is helpful in making the diagnosis of sarcomatoid carcinoma over a primary sarcoma. Earlier treatment with radiation therapy and intravesical cyclophosphamide chemotherapy has been associated with sarcomatoid carcinoma, as also with external beam radiation for prostate cancer.
Figure 9
Sarcomatoid carcinoma of the urinary bladder. Urothelial carcinoma and high-grade spindle cell morphology of sarcomatoid component. Heterologous cartilaginous differentiation.
Clinical Behavior Of Bladder Urothelial Carcinoma In Young Patients: A Single Center Experience
Volkan Sen
1Department of Urology, Dokuz Eylul University School of Medicine, 35330 Izmir, Turkey
Academic Editor:
Abstract
Background. There is not enough evidence about clinical behavior of bladder cancer in younger patients. Objective. We aimed to evaluate the clinical characteristics and prognosis of bladder urothelial carcinoma patients under the age of 40 years. Methods. Medical records of patients listed in our cancer database were retrospectively reviewed. A total of 40 patients who were initially diagnosed with bladder urothelial carcinoma at the age less than 40 years were included in the study. Patients records were reviewed for recurrence and progression rates, demographic data, medical history, and treatment modalities. Results. Pathological results revealed 33 Ta low-grade, 6 T1 high-grade, and 1 T2 high-grade urothelial carcinomas. Recurrence was detected in 14/39 patients but progression was not observed in any patients. The mean age of recurrent patients was significantly higher than nonrecurrent patients . Besides, recurrence was detected in only 1 patient with the age under 30 years and 13 patients between 30 and 40 years old, respectively .. Bladder urothelial carcinoma diagnosed at young age tends to be a low pathologic stage, with relatively low rate of recurrence and progression.
1. Introduction
2. Materials and Methods
2.1. Statistical Analysis
3. Results
| Age range |
4. Discussion
5. Conclusions
Competing Interests
References
Copyright
You May Like: What Are The Symptoms Of Squamous Cell Carcinoma