World Health Organisation Grades
Another grading system sometimes used for early bladder cancer. This divides bladder cancers into 4 groups:
- urothelial papilloma means it is a non cancerous tumour
- papillary urothelial neoplasm of low malignant potential means it is a very slow growing tumour that is unlikely to spread
- low grade papillary urothelial carcinoma is a slow growing cancer that is unlikely to spread
- high grade papillary urothelial carcinoma is a quicker growing cancer that is more likely to spread
-
American Joint Committee on Cancer manual S Edge and othersSpringer, 2017
-
The 2016 WHO Classification of Tumours of the Urinary System and Male Genital Organs Part B: Prostate and Bladder TumoursP A Humphrey and othersEuropean Urology, 2016. Volume 70, Issue 1, Pages 106-119
-
Bladder cancer: diagnosis and management of bladder cancerNational Institute of Health and Clinical Excellence, 2015
-
BMJ Best Practice. Bladder CancerD Lamm and othersBMJ Publishing Group,
-
Bladder cancer
Urothelial Tumors Of The Urinary Bladder In Young Patients: A Clinicopathologic Study Of 59 Cases
Melissa L. Stanton, Li Xiao, Bogdan A. Czerniak, Charles C. Guo Urothelial Tumors of the Urinary Bladder in Young Patients: A Clinicopathologic Study of 59 Cases. Arch Pathol Lab Med 1 October 2013 137 : 13371341. doi:
Context.Urothelial tumors are rare in young patients. Because of their rarity, the natural history of the disease in young patients remains poorly understood.
Objective.To understand the pathologic and clinical features of urothelial tumors of the urinary bladder in young patients.
Design.We identified 59 young patients with urothelial tumors of the urinary bladder treated at our institution and analyzed the tumors pathologic features and the patients clinical outcomes.
.Urothelial tumors in young patients are mostly noninvasive, papillary carcinomas and have an excellent prognosis however, a small subset of patients may present with high-grade invasive urothelial carcinomas that result in poor clinical outcomes.
Clinical Behavior Of Bladder Urothelial Carcinoma In Young Patients: A Single Center Experience
Volkan Sen
1Department of Urology, Dokuz Eylul University School of Medicine, 35330 Izmir, Turkey
Academic Editor:
Abstract
Background. There is not enough evidence about clinical behavior of bladder cancer in younger patients. Objective. We aimed to evaluate the clinical characteristics and prognosis of bladder urothelial carcinoma patients under the age of 40 years. Methods. Medical records of patients listed in our cancer database were retrospectively reviewed. A total of 40 patients who were initially diagnosed with bladder urothelial carcinoma at the age less than 40 years were included in the study. Patients records were reviewed for recurrence and progression rates, demographic data, medical history, and treatment modalities. Results. Pathological results revealed 33 Ta low-grade, 6 T1 high-grade, and 1 T2 high-grade urothelial carcinomas. Recurrence was detected in 14/39 patients but progression was not observed in any patients. The mean age of recurrent patients was significantly higher than nonrecurrent patients . Besides, recurrence was detected in only 1 patient with the age under 30 years and 13 patients between 30 and 40 years old, respectively .. Bladder urothelial carcinoma diagnosed at young age tends to be a low pathologic stage, with relatively low rate of recurrence and progression.
1. Introduction
Read Also: Invasive Ductal Breast Cancer Survival Rate
Urinalysis And Urine Culture
Urinalysis is used routinely to evaluate for the presence of red blood cells , WBCs, and protein and to assess for urinary tract infection. The presence of RBCs in the urine mandates an evaluation by a urologist to investigate for any serious disease. American Urological Association guidelines recommend against relying on dipstick testing alone to diagnose microhematuria, and instead advise following up a positive dipstick test with a formal evaluation the AUA defines microhematuria as 3 red blood cells per high-power field on microscopic evaluation of a single properly collected urine specimen.” Workup of microhematuria should be based on history and physical exam findings while taking into consideration the patient’s individual risk factors for genitourinary malignancy.
Gross hematuria always requires a careful assessment with imaging studies of the entire urinary tract and cystoscopy. However, prior to performing an endoscopic examination or initiating any therapy, a urine culture should be performed to confirm that the urine is free of evidence of infection. Although microhematuria may be present in healthy persons, 13-34.5% of patients with gross hematuria and 0.5-10.5% of patients with microscopic hematuria will be diagnosed with bladder cancer on initial evaluation.
About The Bladder Renal Pelvis And Ureter
The bladder is a hollow organ in the pelvis that stores urine before it leaves the body during urination. This function makes the bladder an important part of the urinary tract. The urinary tract is also made up of the kidneys, ureters, and urethra. The renal pelvis is a funnel-like part of the kidney that collects urine and sends it into the ureter. The ureter is a tube that runs from each kidney into the bladder. The urethra is the tube that carries urine out of the body. The prostate gland is also part of the urinary tract.
The bladder, like other parts of the urinary tract, is lined with a layer of cells called the urothelium. This layer of cells is separated from the bladder wall muscles, called the muscularis propria, by a thin, fibrous band called the lamina propria.
Don’t Miss: Invasive Ductal Carcinoma Grade 3 Survival Rate
Prognosis And Life Expectancy
In general, papillary urothelial cancers have a better prognosis than other types of bladder cancer. Your specific outlook depends on the stage and grade of your cancer. High-grade cancers can spread. Low-grade papillary cancers are less likely to spread. Papillary cancers can also return after theyve been treated.
Stage Iv Bladder Cancer Treatment
Only a small fraction of patients with stage IV bladder cancer can be cured, and for many patients, the emphasis is on palliation of symptoms. The potential for cure is restricted to patients with stage IV disease with involvement of pelvic organs by direct extension or metastases to regional lymph nodes.
Also Check: Prognosis Of Skin Cancer
Treatment Options Under Clinical Evaluation For Patients With Any T Any N M1 Disease
Prognosis is poor in patients with stage IV disease and consideration of entry into a clinical trial is appropriate.
Other chemotherapy regimens appear to be active in the treatment of metastatic disease. Chemotherapy agents that have shown activity in metastatic bladder cancer include paclitaxel, docetaxel, ifosfamide, gallium nitrate, and pemetrexed.
Also Check: Can Melanoma Be Treated Successfully
Irocker Cruiser Paddle Board
Newbie boarders with a spot of curiosity and magical journey in their spirit. Outfitted with an extra-wide 33 base, broad tail, as well as balance functions making this board the steadiest iSUP on the marketplace. With a 400lbs weight capability, its developed to manage any kind of rider.
Stand up with convenience and also try some on-board yoga sensation secure above water the perfect novice board to feed that daring side. A smooth introduction to paddleboarding that will certainly make you rely on yourself!
Read Also: How Long Does It Take Melanoma To Metastasize
Cancerous Tumours Of The Bladder
A cancerous tumour of the bladder can grow into nearby tissue and destroy it. It can also spread to other parts of the body. Cancerous tumours are also called malignant tumours.
Bladder cancer is often divided into 3 groups based on how much it has grown into the bladder wall.
- Non-invasive bladder cancer is only in the inner lining of the bladder .
- Nonâmuscle-invasive bladder cancer has only grown into the connective tissue layer .
- Muscle-invasive bladder cancer has grown into the muscles deep within the bladder wall and sometimes into the fat that surrounds the bladder.
What Is Urothelial Carcinoma
Urothelial Carcinoma is a multifocal malignancy associated with the reno-urinary system. Renal parenchyma often develops a high-grade scirrhous mass formation and turns to a malignant tumor. In urothelial carcinoma, the organ which can get affected with malignant attacks is renal pelvis, ureters, and bladder. The possibility of this organ get affected with Urothelial Carcinoma can be estimated as 1:3:50 respectively.
It has been observed that upper urinary tract cancer affected patients have a 30 to 50 percent tendency to develop bladder cancer, whereas bladder cancer affected individuals also has a 2 to 3 percent tendency to develop urinary tract cancer. Therefore, the reno-urinary system is interconnected and the scope of cancer progression also inter-related1,2.
Don’t Miss: Invasive Ductal Carcinoma Survival Rate
Treating Stage I Bladder Cancer
Stage I bladder cancers have grown into the connective tissue layer of the bladder wall , but have not reached the muscle layer.
Transurethral resection with fulguration is usually the first treatment for these cancers. But itâs done to help determine the extent of the cancer rather than to try to cure it. If no other treatment is given, many people will later get a new bladder cancer, which often will be more advanced. This is more likely to happen if the first cancer is high-grade .
Even if the cancer is found to be low grade , a second TURBT is often recommended several weeks later. If the doctor then feels that all of the cancer has been removed, intravesical BCG or intravesical chemo is usually given. If all of the cancer wasnât removed, options are intravesical BCG or cystectomy .
If the cancer is high grade, if many tumors are present, or if the tumor is very large when itâs first found, radical cystectomy may be recommended.
For people who arent healthy enough for a cystectomy, radiation therapy might be an option, but the chances for cure are not as good.
Micropapillary Variant Of Urothelial Carcinoma
Approximately 120 cases of this variant have been reported since the first description of a series of cases in the urinary bladder in 1994., , , , , , , , , , , This rare histological variant comprises 0.61% of urothelial carcinomas and shows a definite male predominance , which is higher than in conventional urothelial carcinoma . This histological variant of urothelial carcinoma has a micropapillary architecture, which is reminiscent of the papillary configuration seen in ovarian papillary serous tumors . The majority of tumors are muscle invasive at the time of presentation. Histologically, the micropapillary component of these tumors may be encountered in the non-invasive component, invasive component and in metastasis. This pattern may be focal, extensive or exclusive. The percentage of micropapillary component has been shown to be a significant adverse prognostic factor. There is no specified criterion required to designate a case as micropapillary carcinoma, and most series in the literature have included cases with < 10% to almost pure micropapillary histology. The author personally diagnoses cases specifying the percentage of micropapillary histology using terminology such as Urothelial carcinoma, high grade, with micropapillary histology and invasion into muscularis propria accompanying urothelial carcinoma in situ, non-papillary mucosa.
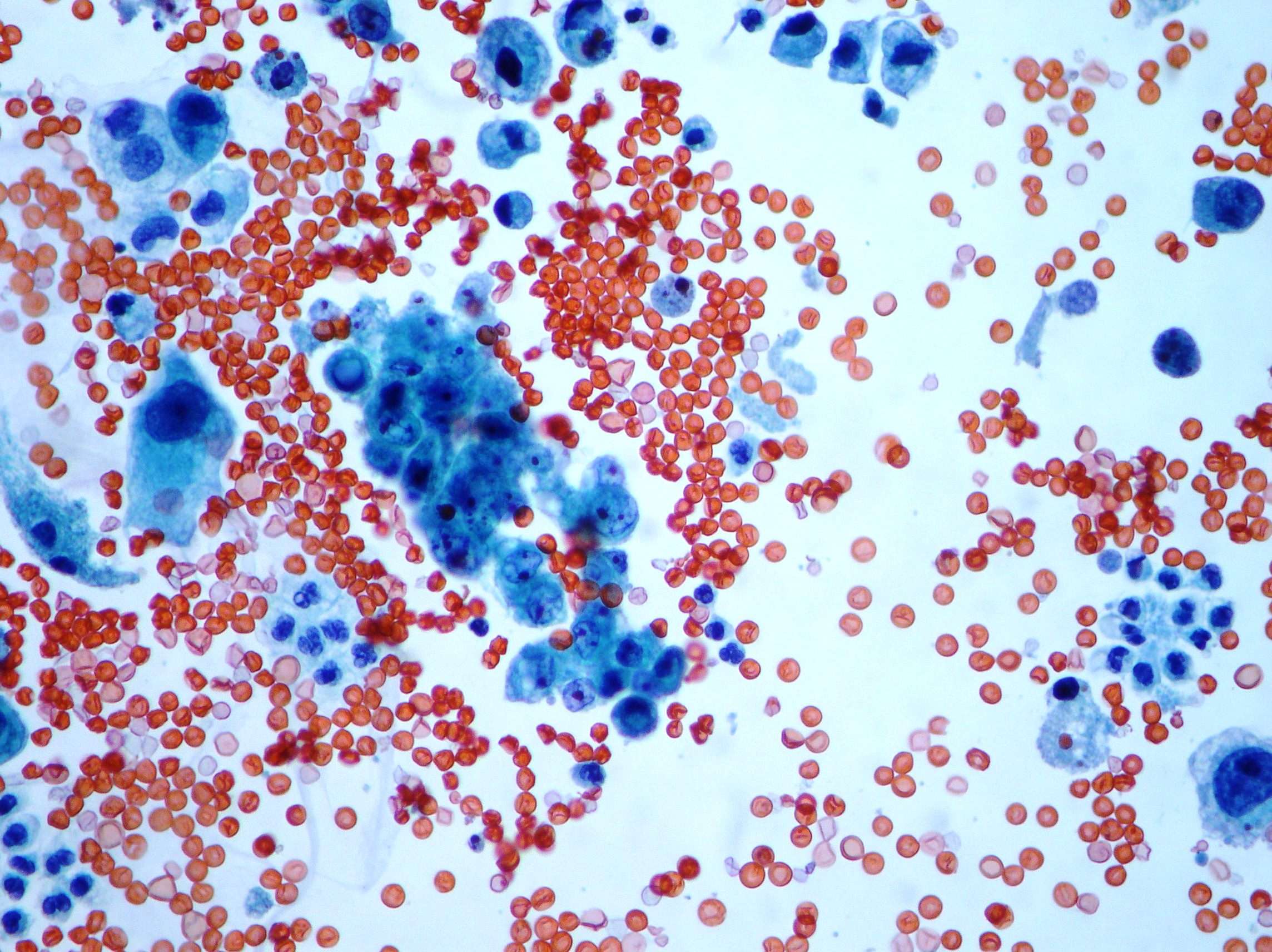
Figure 7
Read Also: How Many Types Of Skin Cancer Exist
Also Check: Lobular Carcinoma Survival Rate
Prognosis & Survival Rate
The prognosis of the Urothelial Carcinoma depends upon the invasive nature of the malignancy and spreading of metastasizing. In the case of initial stage low-grade cancerous lesion provides a good prognosis, whereas poor prognosis is reported with the high grade cancerous lesion. The local invasion of the carcinoma can provide 5 years survival, whereas involvement of the lymph nodes can cause 0 to 30 percent 5 years survival1.
References
Discuss The Differential Diagnosis Of Hematuria And The Preliminary Working Diagnosis
Gross hematuria is when blood is visible in the urine, while microscopic hematuria is defined as 3 or more red blood cells per high-power field in a urine specimen. Hematuria can arise from anywhere along the urinary tract, including the kidney, ureter, bladder, prostate, and urethra. Etiologies include glomerular disease, neoplastic processes, calculi, trauma, and infections such as urethritis, prostatitis, and pyelonephritis. Other less common causes include uretero-arterial fistulas, hemorrhagic cystitis, and urethral strictures. Elements crucial to distinguishing between these etiologies include urinary symptoms, the presence and location of pain, fever, recent trauma, prior obstruction, and radiotherapy or family history. Unilateral flank pain is highly suggestive of calculi but may also be present in malignancy. Findings suggestive of infection include fever, dysuria, and white blood cells and bacteria in the urine. This patients microhematuria with dysuria and lack of flank pain suggests a diagnosis of benign prostatic hyperplasia or malignancy.
Don’t Miss: What Is The Survival Rate For Invasive Ductal Carcinoma
What Is Papillary Renal Cell Carcinoma
Papillary renal cell carcinoma, or PRCC, is a type of kidney cancer. The kidneys work by removing waste products from the blood. Papillary renal cell carcinoma is a cancer of the tubes that filter those waste products from the blood. There are two types of papillary renal cell carcinoma. Type 1 is more common and grows slowly. Type 2 is more aggressive and grows more quickly.
How Will My Doctor Test For It
Youll need a few different tests to see if a nodule is cancer.
Physical exam. Your doctor will feel for unusual growths in your neck and ask about any symptoms you might have.
Blood tests. You may get your thyroid hormone levels checked. This wont tell you if you have cancer, but it gives more information about how your thyroid is working.
Ultrasound. Youll get this test, which uses sound waves to make a picture of things inside your body, to learn more about nodules you have. Your doctor will find out about their shape, size, and other features. That will give important clues to decide how much of a problem they are.
Biopsy. Your doctor will use a very fine needle to take a sample of the nodule to test for cancer. Typically, the most youll feel during it is a small pinch.
Youll likely get this done for any nodule thats bigger than 1 centimeter . Nodules with calcium buildup, lots of blood vessels, or without clear borders raise red flags. So do unusual-looking nearby lymph nodes bean-shaped organs that help fight infections.
Read Also: How To Remove Skin Cancer Yourself
Also Check: Large Cell Carcinoma Lung Cancer
Sarcomatoid Carcinoma Of The Urinary Bladder
The sarcomatoid areas may merge with foci of urothelial carcinoma , squamous cell carcinoma, adenocarcinoma or small-cell carcinoma, and most commonly resemble a high-grade sarcoma, not otherwise specified, or have a malignant fibrous histiocytoma histology. Heterologous differentiation may be present but has no definite prognostic significance . In decreasing order of frequency, areas of osteosarcoma, chondrosarcoma, rhabdomyosarcoma, liposarcoma, angiosarcoma or a mixture of sarcoma histologies may be seen. In the absence of an obvious invasive carcinoma , in a primarily malignant spindle cell tumor of the bladder, history of prior urothelial neoplasia, coexistence of in situ disease such as urothelial carcinoma in situ or strong and relatively diffuse cytokeratin immunoreactivity is helpful in making the diagnosis of sarcomatoid carcinoma over a primary sarcoma. Earlier treatment with radiation therapy and intravesical cyclophosphamide chemotherapy has been associated with sarcomatoid carcinoma, as also with external beam radiation for prostate cancer.
Figure 9
Sarcomatoid carcinoma of the urinary bladder. Urothelial carcinoma and high-grade spindle cell morphology of sarcomatoid component. Heterologous cartilaginous differentiation.
What Systems Are Used To Classify The Pathology Identified On Urine Cytology What Are The Advantages Of The Paris System For Reporting Urine Cytology
The original criteria for the cytomorphological description of cancer cells in urine cytology were established by Drs Papanicolaou and Marshall in 1947. Dr Leopold Koss expounded upon urine cytology by describing the features used in the classification system and recognizing the limited utility of urine cytology in diagnosing low-grade urothelial carcinoma . Numerous reporting systems have been suggested, but none gained broad acceptance. The Paris System for Reporting Urine Cytology, published in 2016, addressed numerous pitfalls of the previous reporting systems by focusing on the diagnosis of high-grade urothelial carcinoma . The Paris System divides specimens into the following categories: negative for HGUC, atypical, suggestive of HGUC, HGUC, low-grade urothelial neoplasia, and other malignancies.
The Paris System acknowledges the limitations of urine cytology in the diagnosis of LGUC. Although urine cytology has a greater than 95% specificity for HGUC, the sensitivity is highly limited, especially for LGUC. As a result, TPS focuses on detecting high-grade lesions. Although a negative urine test under these criteria does not exclude the possibility of a low-grade lesion, the low risk of progression of LGUC combined with the limited sensitivity of urine cytology for such lesions increases the clinical value of the cytology results.,
Recommended Reading: Merkel Cell Carcinoma Immunotherapy
Diagnostic Yield Sensitivity And Specificity
Changing the threshold to considering the atypical, unclear category among the positive results significantly increased the sensitivity of cytology for high-grade lesions , albeit with a smaller but still significant decrease in specificity .
Considering any atypical diagnosis as positive resulted in a significantly lower degree of specificity for high- and low-grade lesions .
In general, the specificity was lower for low- and high-grade lesions in voided specimens or in a follow-up setting, and this was true regardless of the considered threshold of a positive cytologic diagnosis. On the other hand, the sensitivity for low-grade lesions was higher in voided specimens in contrast with high grade lesions, which were detected more often on instrumented specimens. Complete results are shown in .
Looking For More Of An Introduction
If you would like more of an introduction, explore this related item. Please note that this link will take you to another section on Cancer.Net.
- ASCO Answers Fact Sheet:Read a 1-page fact sheet that offers an introduction to bladder cancer. This free fact sheet is available as a PDF, so it is easy to print.
Don’t Miss: What Type Of Skin Cancer Spreads The Fastest
Standard Treatment Options For Stage I Bladder Cancer
Patients with stage I bladder tumors are unlikely to die from bladder cancer, but the tendency for new tumor formation is high. In a series of patients with Ta or T1 tumors who were followed for a minimum of 20 years or until death, the risk of bladder recurrence after initial resection was 80%. Of greater concern than recurrence is the risk of progression to muscle-invasive, locally-advanced, or metastatic bladder cancer. While progression is rare for low-grade tumors, it is common among high-grade cancers.
One series of 125 patients with TaG3 cancers followed for 15 to 20 years reported that 39% progressed to more advanced stage disease, while 26% died of urothelial cancer. In comparison, among 23 patients with TaG1 tumors, none died and 5% progressed. Risk factors for recurrence and progression include the following:
- High-grade disease.
TUR with fulguration followed by an immediate postoperative instillation of intravesical chemotherapy
TUR and fulguration are the most common and conservative forms of management. Careful surveillance of subsequent bladder tumor progression is important. Because most bladder cancers recur after TUR, one immediate intravesical instillation of chemotherapy after TUR is widely used. Numerous randomized, controlled trials have evaluated this practice, and a meta-analysis of seven trials reported that a single intravesical treatment with chemotherapy reduced the odds of recurrence by 39% .
TUR with fulguration
Evidence :