Detection Of Residual Disease And Tumour Upstaging
The significant risk of residual tumour after initial TURB of TaT1 lesionshas been demonstrated .
A SR analysing data of 8,409 patients with Ta or T1 HG BCdemonstrated a 51% risk of justify persistence and an 8% risk of under-staging in T1tumours. The analysis also showed a high risk of residual disease in Ta tumours, but thisobservation was based only on a limited number of cases. Most of the residual lesions weredetected at the original tumour location .
Another meta-analysis of 3,556 patients with T1 tumoursshowed that the prevalence rate of residual tumours and upstaging to invasive disease afterTURB remained high in a subgroup with detrusor muscle in the resection specimen. In thesubgroup of 1,565 T1 tumours with detrusor muscle present, persistent tumour was found in58% and under-staging occurred in 11% of cases .
Individual Treatment Strategy In Primary Orrecurrent Tumours After Turb Without Previous Bcg Intravesical Immunotherapy
The type of further therapy after TURB should be based on the risk groupsshown in Section 6.3 and Table 6.1. The stratification and treatment recommendations arebased on the risk of disease progression. In particular in intermediate-risk tumours, the2006 EORTC scoring model may be used to determine a patientsindividual risk of disease recurrence as the basis to decide further treatment on.
Any decisions should reflect the following principles :
- Patients in the low-risk group have a negligible risk of disease progression. The singlepost-operative instillation of chemotherapy reduces the risk of recurrence and isconsidered as sufficient treatment in these patients.
- Patients in the intermediate-risk group have a low risk of disease progression . In these patientsone-year full-dose BCG treatment , or instillations of chemotherapy for amaximum of one year, is recommended. The final choice should reflect the individualpatients risk of recurrence and progression as well as the efficacy and sideeffects of each treatment modality.
- Patients in the high-risk group have a high risk of disease progression . In these patientsfull-dose intravesical BCG for one to three years , is indicated. The additional beneficial effectof the second and third years of maintenance should be weighed against its added costs,side-effects and problems connected with BCG shortage.
Figure 7.1: Treatment strategy in primary or recurrent tumourwithout previous BCG*
Prognosis And Life Expectancy
In general, papillary urothelial cancers have a better prognosis than other types of bladder cancer. Your specific outlook depends on the stage and grade of your cancer. High-grade cancers can spread. Low-grade papillary cancers are less likely to spread. Papillary cancers can also return after theyve been treated.
The most common treatments for muscle-invasive bladder cancer are radical cystectomy and radiation therapy. There is no strong evidence from randomized controlled trials to determine whether surgery or radiation therapy is more effective. There is strong evidence that both therapies become more effective when combined with chemotherapy. The treatments with the highest level of evidence supporting their effectiveness are radical cystectomy preceded by multiagent cisplatin-based chemotherapy and radiation therapy with concomitant chemotherapy.
Radical cystectomy
Evidence :
Segmental cystectomy
Also Check: Stage 3 Lobular Breast Cancer
Standard Treatment Options For Stage Iv Bladder Cancer
Standard treatment options for patients with T4b, N0, M0 disease
Treatment options for patients with T4b, N0, M0 disease include the following:
Chemotherapy alone or as an adjunct to local treatment
Cisplatin-based combination chemotherapy regimens are the standard of care for first-line therapy for stage IV bladder cancer in patients who can tolerate it. The only chemotherapy regimens that have been shown to result in longer survival in randomized controlled trials are MVAC, dose-dense MVAC, and CMV. GC was compared with MVAC in a randomized controlled trial and neither regimen was associated with a statistically significant difference in response rate or survival. The two regimens are generally considered equivalent, but they have never been compared in a noninferiority trial. Of note, patients with good performance status and lymph node-only disease have a low but significant rate of achieving a durable complete remission with MVAC or GC. In the large, randomized, controlled trial comparing MVAC with GC, for example, 5-year OS in patients with lymph node-only disease was 20.9%. Dose-dense MVAC and standard-dose MVAC were compared in a randomized controlled trial, and dose-dense MVAC was associated with longer survival.
Ongoing studies are evaluating new chemotherapy combinations.
Evidence :
Ongoing studies are evaluating new chemotherapy combinations.
Immunotherapy
Noninvasive Diagnosis Of High
*Anal. Chem.
Publication History
Article Views are the COUNTER-compliant sum of full text article downloads since November 2008 across all institutions and individuals. These metrics are regularly updated to reflect usage leading up to the last few days.
Citations are the number of other articles citing this article, calculated by Crossref and updated daily. Find more information about Crossref citation counts.
The Altmetric Attention Score is a quantitative measure of the attention that a research article has received online. Clicking on the donut icon will load a page at altmetric.com with additional details about the score and the social media presence for the given article. Find more information on the Altmetric Attention Score and how the score is calculated.
Recommended Reading: Prognosis Of Skin Cancer
Treatment For Hg T1 Bladder Cancer With Pt0 Histology At Second Tur
TURBT followed by intravesical BCG therapy provides lower incidences of recurrence and progression than those obtained by TURBT alone . Sylvester et al. performed a meta-analysis on the efficacy of intravesical BCG therapy. They evaluated 24 trials involving a total of 4863 patients and concluded that intravesical BCG significantly reduces the risk of progression after TURBT in NMIBC patients who receive maintenance treatment. Since T1 bladder cancer is considered to be high-risk cancer regardless of the pathological findings for the second TUR specimen , various guidelines recommend full-dose intravesical BCG for 13 years except in the case of immediate cystectomy. Alternatively, mitomycin C is also recommended by the National Comprehensive Cancer Network guidelines . This is based on a meta-analysis that showed no statistically significant difference between BCG and MMC for progression and survival .
Protocol and study design of the JCOG1019 trial .
Summary Of Evidence And Guidelines Forstratification Of Non
|
Summary of evidence |
|
|
The EAU NMIBC 2021 scoring model and risk tablespredict the short- and long-term risks of disease progression in individualpatients with primary NMIBC using either the WHO 1973 or the WHO 2004/2016classification system . |
|
|
The 2006 EORTC scoring model and risk tables predictthe short- and long-term risks of disease recurrence and progression inindividual patients with NMIBC using the WHO 1973 classification system . |
|
|
Patients with TaG1/G2 tumours receiving chemotherapyhave been further stratified into three risk groups for recurrence, taking intoaccount the history of recurrences, history of intravesical treatment, tumourgrade , number of tumours and adjuvant chemotherapy . |
2a-b |
|
In patients treated with 5 to 6 months of BCG, theCUETO scoring model predicts the short- and long-term risks of diseaserecurrence and progression using the WHO 1973 classification system . |
|
|
In patients receiving at least 1 year of BCGmaintenance prior recurrence rate and number of tumours are the most importantprognostic factors for disease recurrence. Stage and grade are the mostimportant prognostic factors for disease progression and disease-specificsurvival patient age and grade are the most important prognosticfactors for overall survival . |
Don’t Miss: Invasive Ductal Carcinoma Grade 3 Life Expectancy
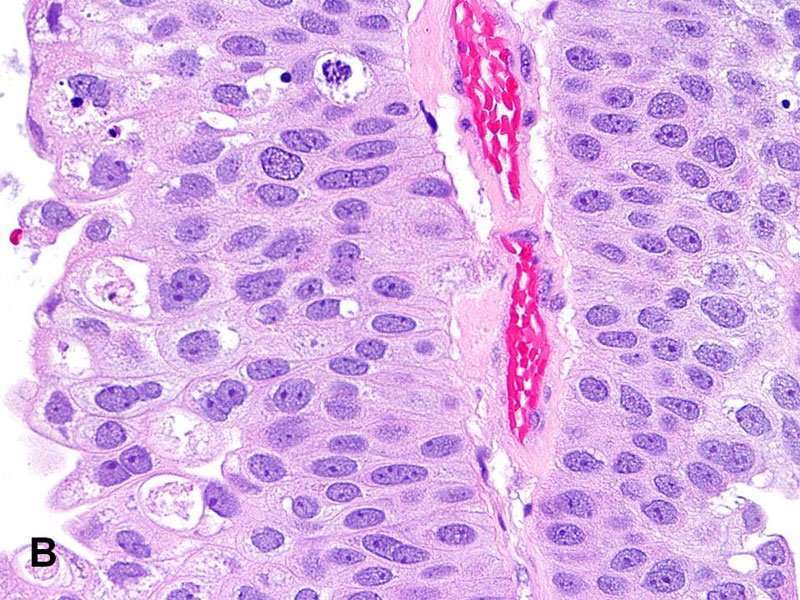
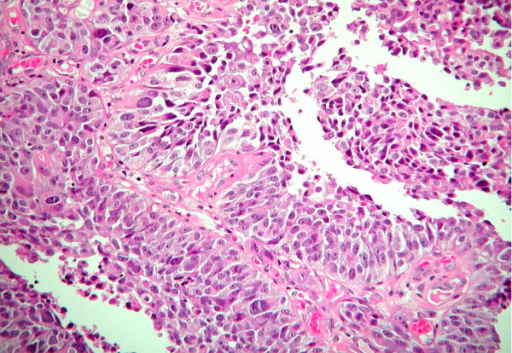
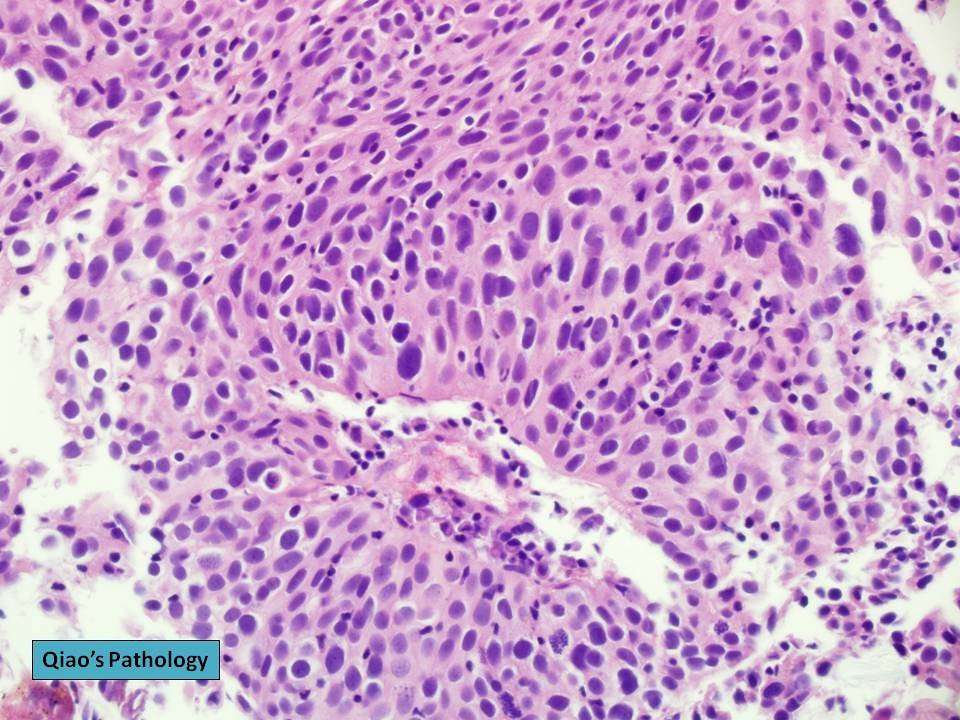
Morphologic Variants Of Urothelial Carcinoma
Some cases of urothelial carcinoma show morphologic patterns that are recognized as variants morphology. Those include nested variant, micropapillary, lymphoepithelioma-like, sarcomatoid, small cell carcinoma, and adenocarcinoma. These are frequently under-recognized in bladder biopsies and could have therapeutic implications with different criteria for surgery and different chemotherapy regimens.
Computed Tomography Urography And Intravenousurography
Computed tomography urography is used to detect papillary tumours inthe urinary tract, indicated by filling defects and/or hydronephrosis .
Intravenous urography is an alternative if CT isnot available , but particularly in muscle-invasivetumours of the bladder and in UTUCs, CT urography provides more information .
The necessity to perform a baseline CT urography once abladder tumour has been detected is questionable due to the low incidence of significantfindings obtained . The incidence of UTUCs is low, but increases to 7.5% in tumours located in the trigone . The risk of UTUC during follow-up increases in patients with multiple- andhigh-risk tumours .
Read Also: Stage 3b Melanoma Survival Rate
What Is Bladder Cancer
Bladder cancer starts when cells that make up the urinary bladder start to grow out of control. As more cancer cells develop, they can form a tumor and, with time, spread to other parts of the body.
The bladder is a hollow organ in the lower pelvis. It has flexible, muscular walls that can stretch to hold urine and squeeze to send it out of the body. The bladders main job is to store urine. Urine is liquid waste made by the 2 kidneys and then carried to the bladder through 2 tubes called ureters. When you urinate, the muscles in the bladder contract, and urine is forced out of the bladder through a tube called the urethra.
Urothelial Cis Without Ihc
All cases of urothelial CIS without IHC were positive for AMACR with a mean intensity of 2.1. The percentage of cases with positive or partially positive AMACR expression was significantly greater for urothelial CIS without IHC compared to urothelial CIS with IHC . The mean intensity was greater in the group urothelial CIS with IHC compared to without IHC, but the difference was not significant . The rate of positivity of AMACR was significantly lower for non-neoplastic urothelium with IHC compared to urothelial CIS without IHC and urothelial CIS with IHC .
You May Like: What Is The Main Cause Of Skin Cancer
Don’t Miss: What Is The Prognosis For Skin Cancer
Stage Information For Bladder Cancer
The clinical staging of carcinoma of the bladder is determined by the depth of invasion of the bladder wall by the tumor. This determination requires a cystoscopic examination that includes a biopsy and examination under anesthesia to assess the following:
- Size and mobility of palpable masses.
- Degree of induration of the bladder wall.
- Presence of extravesical extension or invasion of adjacent organs.
Clinical staging, even when computed tomographic and/or magnetic resonance imaging scans and other imaging modalities are used, often underestimates the extent of tumor, particularly in cancers that are less differentiated and more deeply invasive. CT imaging is the standard staging modality. A clinical benefit from obtaining MRI or positron emission tomography scans instead of CT imaging has not been demonstrated.
Also Check: Is Basal Cell Carcinoma Slow Growing
Standardization Of The Reporting System
Anatomic pathologists serve as consultants to their clinical colleagues and patients, and pathology reports officially document this communication. To help clinicians choose the optimal management options for the patient, reports must accurately and clearly communicate the cytopathologic findings and outcome probability.
Pathologists actively use the terms suspiciousâ, indeterminateâ, or atypicalââ all too often with resultant failure to provide a clear diagnostic and therapeutic path for clinicians. A survey of pathologists and clinicians performed by Redman et al. documented the need for a more standardized terminology for reporting cytopathology results and for the education of clinicians on that terminology. Although pathologists have paid attention to all elements of the pathology report , they have not focused on the issue of report comprehension. In a study looking at surgical pathology reports, surgeons misunderstood pathologistsâ reports 30% of the time . One of the issues shared by patients and their advocates on Web sites dedicated to cancer advocacy is that different pathologists and/or different institutions use different highly technical terms to describe the same entities, predictably confusing to both patients and their clinicians.
Don’t Miss: Well Differentiated Carcinoma
What Is An Urothelial Neoplasm
Urothelial neoplasia is a unique cancer in that is consists of a spectrum of tumors with different biologic behaviors. The most common urothelial neoplasm is the low grade superficial papillary carcinoma or papilloma which may recur numerous times but does not result in significant morbidity or mortality.
Risk Adjusted Surveillance And Follow
Guideline Statement 32
32. After completion of the initial evaluation and treatment of a patient with NMIBC, a clinician should perform the first surveillance cystoscopy within three to four months.
Discussion
The natural history of NMIBC is often characterized by recurrence, even for solitary, small, low-grade papillary tumors. At the time of first evaluation and treatment, none of the existent risk stratification tools or urinary biomarkers is sufficiently sensitive and specific to predict which patient will have an early tumor recurrence. Therefore, the only reliable way to know in a particular patient whether they are at risk for early recurrence is by cystoscopic visualization of the urothelium at a relatively early interval after the first treatment/resection. In addition, visualization at a relatively early interval allows the treating urologist to verify that the initial resection was complete. The Panel, therefore, felt that the first repeat cystoscopic evaluation should occur three to four months after the initial treatment and evaluation, regardless of the patient’s overall risk.
Guideline Statement 33
33. For a low-risk patient whose first surveillance cystoscopy is negative for tumor, a clinician should perform subsequent surveillance cystoscopy six to nine months later, and then annually thereafter surveillance after five years in the absence of recurrence should be based on shared-decision making between the patient and clinician.
Discussion
Discussion
You May Like: Cancer All Over Body Symptoms
Bcg Relapse And Salvage Regimens
Guideline Statement 22
22. In an intermediate- or high-risk patient with persistent or recurrent disease or positive cytology following intravesical therapy, a clinician should consider performing prostatic urethral biopsy and an upper tract evaluation prior to administration of additional intravesical therapy.
Discussion
Urothelial carcinoma, particularly CIS, is considered a field-change disease with the entire urothelium at risk in affected individuals. Clinicians should remain aware of sites outside the bladder as potential sources for metachronous tumors. While the initial diagnostic evaluation includes radiographic/endoscopic visualization of the entire urinary tract, the extra-vesical urothelium remains at long-term risk for subsequent tumor development. Moreover, these sites may harbor disease and contribute to cancer recurrence within the bladder.
Of note, the Panel recognizes that evaluation of the upper urinary tract and urethra may be withheld in select patients who have received a single induction course of intravesical BCG and subsequently have persistent evidence of disease and are to undergo a second course of BCG.
Guideline Statement 23
23. In an intermediate- or high-risk patient with persistent or recurrent Ta or CIS disease after a single course of induction intravesical BCG, a clinician should offer a second course of BCG.
Discussion
Guideline Statement 24
Discussion
Guideline Statement 25
Discussion
Guideline Statement 26
Counselling Of Smoking Cessation
It has been confirmed that smoking increases the risk of tumour recurrenceand progression . Whileit is still controversial whether smoking cessation in BC will favourably influence theoutcome of BC treatment, patients should be counselled to stop smoking due to the generalrisks connected with tobacco smoking .
Read Also: What Is The Survival Rate For Invasive Ductal Carcinoma
Bladder Cancer Clinical Trials
What about Clinical Trials?
You may hear about clinical trials for your bladder cancer. Clinical trials are research studies that test if a new treatment or procedure is safe and effective.
Through clinical trials, doctors find new ways to improve treatments and the quality of life for people with disease. Trials are available for all stages of cancer. The results of a clinical trial can make a major difference to patients and their families. Please visit our clinical trials research webpage to learn more.
Grade And Risk Category
The biopsy results will show the grade of the cancer. This is a score that describes how quickly a cancer might grow. Knowing the grade helps your urologist predict how likely the cancer is to come back and if you will need further treatment after surgery.
| Low grade | The cancer cells look similar to normal bladder cells, are usually slow-growing and are less likely to invade and spread. Most bladder tumours are low grade. |
| High grade | The cancer cells look very abnormal and grow quickly. They are more likely to spread both into the bladder muscle and outside the bladder.
In non-muscle-invasive tumours, the grade may be low or high, while almost all muscle-invasive cancers are high grade. Carcinoma in situ is a high-grade tumour that needs prompt treatment to prevent it invading the muscle layer. |
| Risk category | Based on the stage, grade and other features, a non-muscle-invasive bladder cancer will also be classified as having a low, medium or high risk of returning after treatment. This will help your doctors work out which treatments to recommend. |
You May Like: Skin Cancer 1st Stage
Urine Cytology Collection Report:
A report consisting of values of carcinoma-in-situ , low-grade urothelial neoplasm , high-grade urothelial neoplasm , positive predictive value . Also, the number of atypical urothelial cells and suspicious for high-grade urothelial carcinoma is called a urine cytology report.
High-grade cancer cells that become tumor after growing at a particular extent is called high-grade urothelial neoplasm . These cells multiply and are predicted to have a worse condition.
Low-grade urothelial neoplasm is linked to atypical urothelial cells. Low-grade urothelial carcinoma is also reported where the cells grow very slowly as a result of low malignant potential of the tumor.
Sometimes there may be cancer cells detected in high-grade urothelial neoplasm, but the number of cancer cells may be not as much as required for a malignancy. Therefore, the report indicates suspicion for high-grade urothelial neoplasm.
Types Of Bladder Cancer
The type of bladder cancer depends on how the tumors cells look under the microscope. The 3 main types of bladder cancer are:
-
Urothelial carcinoma. Urothelial carcinoma accounts for about 90% of all bladder cancers. It also accounts for 10% to 15% of kidney cancers diagnosed in adults. It begins in the urothelial cells found in the urinary tract. Urothelial carcinoma is sometimes also called transitional cell carcinoma or TCC.
-
Squamous cell carcinoma. Squamous cells develop in the bladder lining in response to irritation and inflammation. Over time, these cells may become cancerous. Squamous cell carcinoma accounts for about 4% of all bladder cancers.
-
Adenocarcinoma. This type accounts for about 2% of all bladder cancers and develops from glandular cells.
There are other, less common types of bladder cancer, including sarcoma of the bladder and small cell bladder cancer, among others. Sarcomas of the bladder often begin in the fat or muscle layers of the bladder. Small cell bladder cancer is a rare type of bladder cancer that is likely to spread to other parts of the body.
Recommended Reading: Can You Get Skin Cancer On Your Scalp
Also Check: Non Invasive Breast Cancer Survival Rate