Sarcomatoid Carcinoma Of The Urinary Bladder
The sarcomatoid areas may merge with foci of urothelial carcinoma , squamous cell carcinoma, adenocarcinoma or small-cell carcinoma, and most commonly resemble a high-grade sarcoma, not otherwise specified, or have a malignant fibrous histiocytoma histology. Heterologous differentiation may be present but has no definite prognostic significance . In decreasing order of frequency, areas of osteosarcoma, chondrosarcoma, rhabdomyosarcoma, liposarcoma, angiosarcoma or a mixture of sarcoma histologies may be seen. In the absence of an obvious invasive carcinoma , in a primarily malignant spindle cell tumor of the bladder, history of prior urothelial neoplasia, coexistence of in situ disease such as urothelial carcinoma in situ or strong and relatively diffuse cytokeratin immunoreactivity is helpful in making the diagnosis of sarcomatoid carcinoma over a primary sarcoma. Earlier treatment with radiation therapy and intravesical cyclophosphamide chemotherapy has been associated with sarcomatoid carcinoma, as also with external beam radiation for prostate cancer.
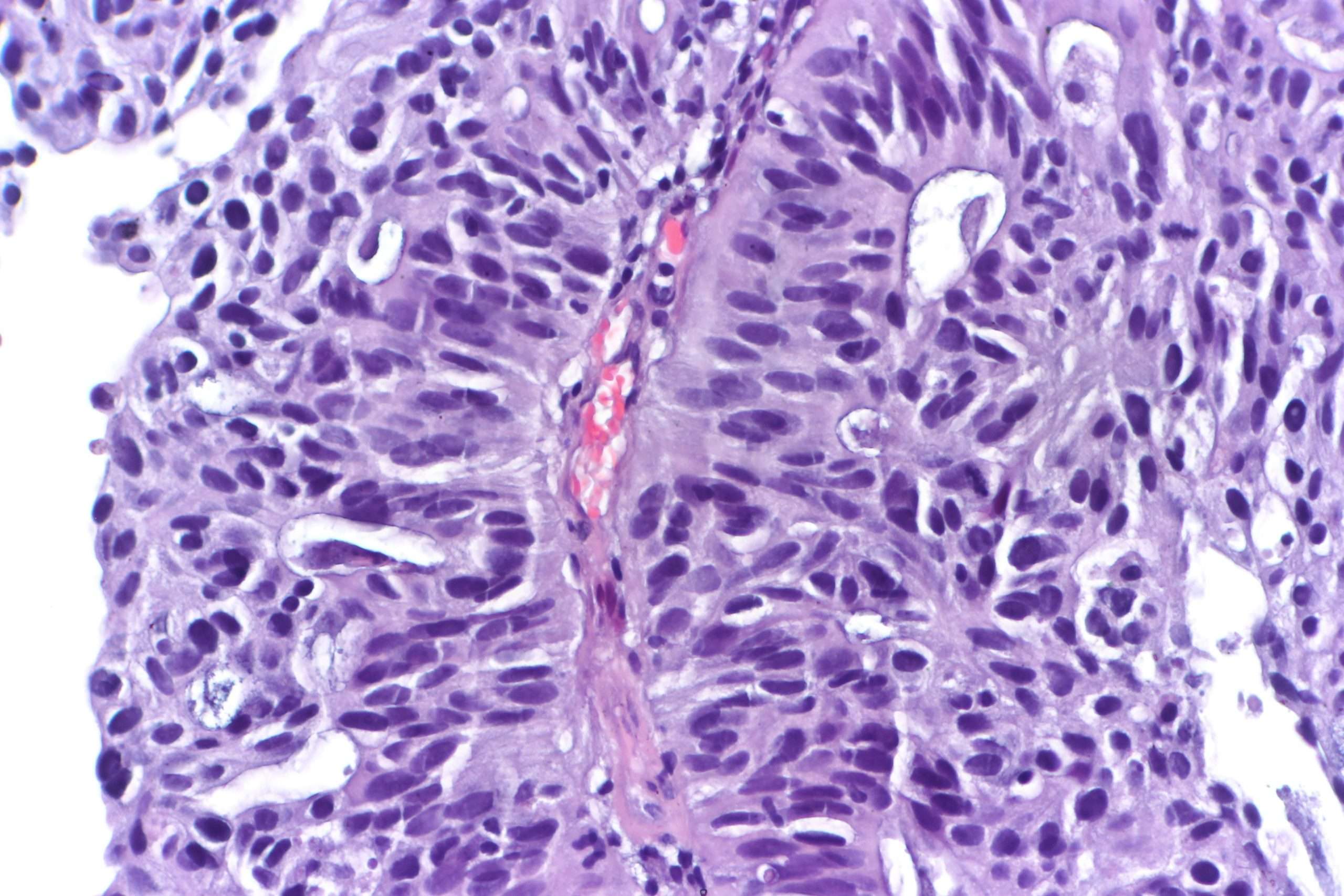
Figure 9
Sarcomatoid carcinoma of the urinary bladder. Urothelial carcinoma and high-grade spindle cell morphology of sarcomatoid component. Heterologous cartilaginous differentiation.
Cellular Classification Of Bladder Cancer
More than 90% of bladder cancers are transitional cell carcinomas derived from the uroepithelium. About 2% to 7% are squamous cell carcinomas, and 2% are adenocarcinomas. Adenocarcinomas may be of urachal origin or nonurachal origin; the latter type is generally thought to arise from metaplasia of chronically irritated transitional epithelium. Small cell carcinomas also may develop in the bladder. Sarcomas of the bladder are very rare.
Pathologic grade of transitional cell carcinomas, which is based on cellular atypia, nuclear abnormalities, and the number of mitotic figures, is of great prognostic importance.
References
Treatment Options Under Clinical Evaluation For Patients With Any T Any N M1 Disease
Prognosis is poor in patients with stage IV disease and consideration of entry into a clinical trial is appropriate.
Other chemotherapy regimens appear to be active in the treatment of metastatic disease. Chemotherapy agents that have shown activity in metastatic bladder cancer include paclitaxel, docetaxel, ifosfamide, gallium nitrate, and pemetrexed.
Also Check: Can Melanoma Be Treated Successfully
What Is The Prognosis For Someone With Prcc
The estimate of how a disease will affect you long-term is called prognosis. Every person is different and prognosis will depend on many factors, such as
- Where the tumor is in your body
- If the cancer has spread to other parts of your body
- How much of the tumor was taken out during surgery
If you want information on your prognosis, it is important to talk to your doctor. NCI also has resources to help you understand cancer prognosis.;
Doctors estimate survival rates by how groups of people with PRCC have done in the past. Because there are so few people with PRCC, these rates may not be very accurate. They also cant consider newer treatments being developed.
In general, type 2 papillary renal cell carcinoma has a poorer prognosis than type 1.;
Related Resources
Micropapillary Variant Of Urothelial Carcinoma
Approximately 120 cases of this variant have been reported since the first description of a series of cases in the urinary bladder in 1994., , , , , , , , , , , This rare histological variant comprises 0.61% of urothelial carcinomas and shows a definite male predominance , which is higher than in conventional urothelial carcinoma . This histological variant of urothelial carcinoma has a micropapillary architecture, which is reminiscent of the papillary configuration seen in ovarian papillary serous tumors . The majority of tumors are muscle invasive at the time of presentation. Histologically, the micropapillary component of these tumors may be encountered in the non-invasive component, invasive component and in metastasis. This pattern may be focal, extensive or exclusive. The percentage of micropapillary component has been shown to be a significant adverse prognostic factor. There is no specified criterion required to designate a case as micropapillary carcinoma, and most series in the literature have included cases with <10% to almost pure micropapillary histology. The author personally diagnoses cases specifying the percentage of micropapillary histology using terminology such as Urothelial carcinoma, high grade, with micropapillary histology and invasion into muscularis propria ; accompanying urothelial carcinoma in situ, non-papillary mucosa.
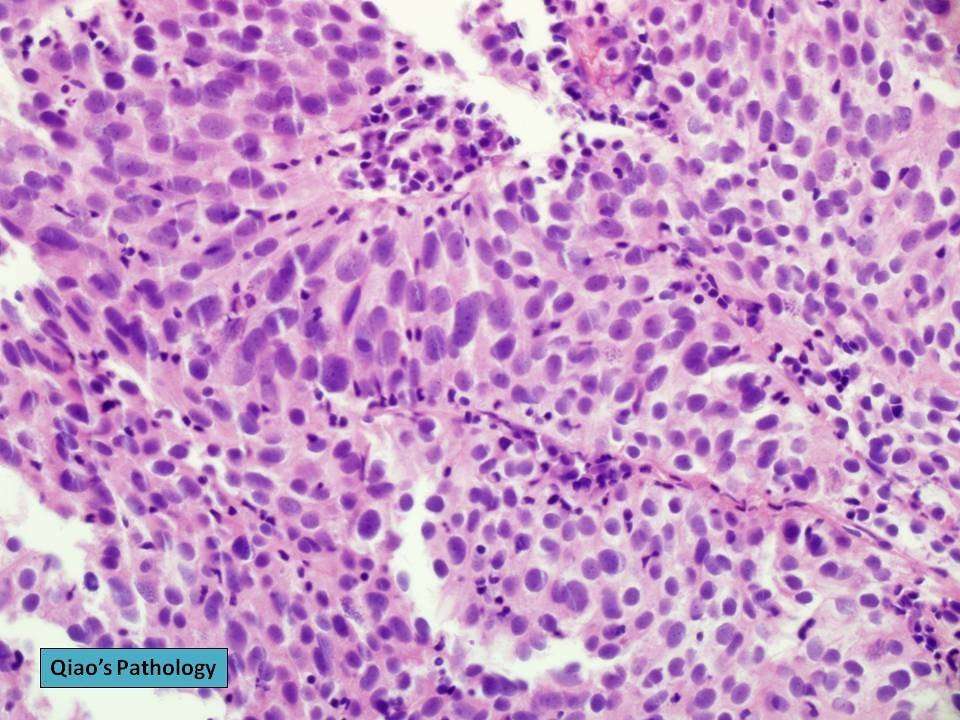
Figure 7
Read Also: How Many Types Of Skin Cancer Exist
Types Of Bladder Cancer
The type of bladder cancer depends on how the tumors cells look under the microscope. The 3 main types of bladder cancer are:
-
Urothelial carcinoma. Urothelial carcinoma accounts for about 90% of all bladder cancers. It also accounts for 10% to 15% of kidney cancers diagnosed in adults. It begins in the urothelial cells found in the urinary tract. Urothelial carcinoma is sometimes also called transitional cell carcinoma or TCC.
-
Squamous cell carcinoma. Squamous cells develop in the bladder lining in response to irritation and inflammation. Over time, these cells may become cancerous. Squamous cell carcinoma accounts for about 4% of all bladder cancers.
-
Adenocarcinoma. This type accounts for about 2% of all bladder cancers and develops from glandular cells.
There are other, less common types of bladder cancer, including sarcoma of the;bladder and small cell bladder cancer, among others. Sarcomas of the bladder often begin in the fat or muscle layers of the bladder. Small cell bladder cancer is a rare type of bladder cancer that is likely to spread to other parts of the body.
Urothelial Carcinoma With Trophoblastic Differentiation
More than 30 cases of urothelial carcinoma with areas of trophoblastic differentiation have been reported and a small subset has had symptoms related to excess human chorionic gonadotropin production including gynecomastia., , , , Although some of the early reports have described tumors that apparently were composed solely of tissue resembling choriocarcinoma, most tumors reported in the last three decades or so have been composed of a mixture of urothelial carcinoma with trophoblastic elements. A single case of micropapillary carcinoma with trophoblastic elements has been reported.
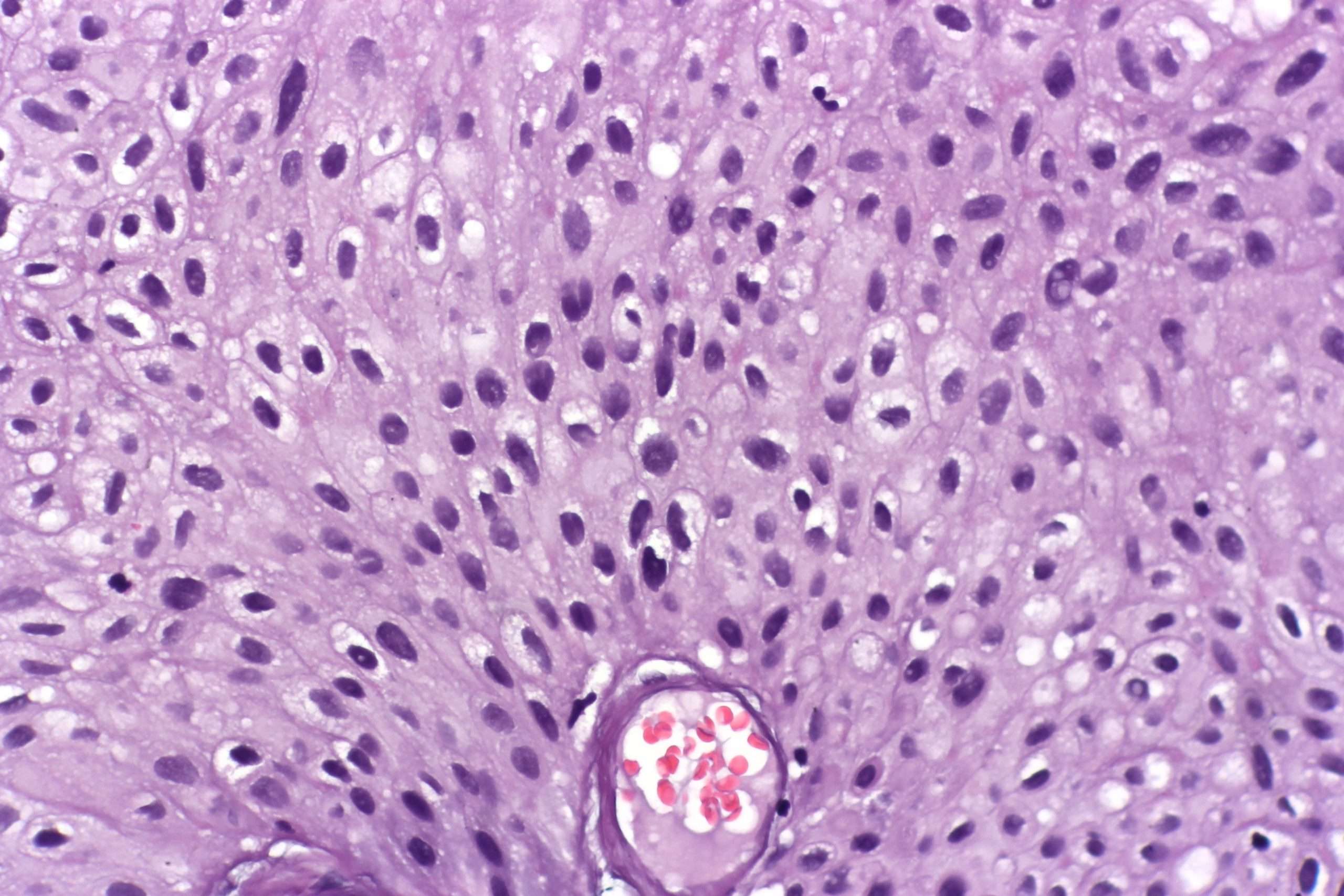
Figure 11
Urothelial carcinoma with trophoblastic differentiation. Choriocarcinoma component with biphasic histology including syncytiotrophoblastic giant cells.
Also Check: Can Merkel Cell Carcinoma Be Cured
Treating Stage I Bladder Cancer
Stage I bladder cancers have grown into the connective tissue layer of the bladder wall , but have not reached the muscle layer.
Transurethral resection with fulguration is usually the first treatment for these cancers. But it’s done to help determine the extent of the cancer rather than to try to cure it. If no other treatment is given, many people will later get a new bladder cancer, which often will be more advanced. This is more likely to happen if the first cancer is high-grade .
Even if the cancer is found to be low grade , a second TURBT is often recommended several weeks later. If the doctor then feels that all of the cancer has been removed, intravesical BCG or intravesical chemo is usually given. If all of the cancer wasn’t removed, options are intravesical BCG or cystectomy .
If the cancer is high grade, if many tumors are present, or if the tumor is very large when it’s first found, radical cystectomy may be recommended.
For people who arent healthy enough for a cystectomy, radiation therapy might be an option, but the chances for cure are not as good.
Irocker Blackfin Paddle Board Xl
Functionality, swiftness, and stableness make this set of our most preferred boards. If you like paddling at speed, with add-ons to entertain, then this board is created you.
For taller riders over 5 8 the Blackfin XL iSUP maneuvers completely through any type of water environment and is great for natural buffs who intend to fish as well as bring camping gear along for the tripexpedition}.
It has an array of attributes, transforming to a dual kayak and integrated fishing installs. Adventure applicants and adventure enthusiasts, its time to enhance the means you paddle.
Don’t Miss: How Do You Know If Squamous Cell Carcinoma Has Spread
Treating Stage 0 Bladder Cancer
Stage 0 bladder cancer includes non-invasive papillary carcinoma and flat non-invasive carcinoma . In either case, the cancer is only in the inner lining layer of the bladder. It has not invaded the bladder wall.
This early stage of bladder cancer is most often treated with transurethral resection with fulguration followed by intravesical therapy within 24 hours.
Prognosis & Survival Rate
The prognosis of the Urothelial Carcinoma depends upon the invasive nature of the malignancy and spreading of metastasizing. In the case of initial stage low-grade cancerous lesion provides a good prognosis, whereas poor prognosis is reported with the high grade cancerous lesion. The local invasion of the carcinoma can provide 5 years survival, whereas involvement of the lymph nodes can cause 0 to 30 percent 5 years survival1.
References
Recommended Reading: What Does Skin Cancer Look Like On Your Head
Read Also: How To Protect Your Self From Skin Cancer
Irocker Cruiser Paddle Board
Newbie boarders with a spot of curiosity and magical journey in their spirit. Outfitted with an extra-wide 33 base, broad tail, as well as balance functions making this board the steadiest iSUP on the marketplace. With a 400lbs weight capability, its developed to manage any kind of rider.
Stand up with convenience and also try some on-board yoga sensation secure above water the perfect novice board to feed that daring side. A smooth introduction to paddleboarding that will certainly make you rely on yourself!
Papillary Vs Flat Cancer
Bladder cancers are also divided into 2 subtypes, papillary and flat, based on how they grow .
- Papillary carcinomas grow in slender, finger-like projections from the inner surface of the bladder toward the hollow center. Papillary tumors often grow toward the center of the bladder without growing into the deeper bladder layers. These tumors are called non-invasive papillary cancers. Very low-grade , non-invasive papillary cancer is sometimes called papillary urothelial neoplasm of low-malignant potential and tends to have a very good outcome.
- Flat carcinomas do not grow toward the hollow part of the bladder at all. If a flat tumor is only in the inner layer of bladder cells, it’s known as a non-invasive flat carcinoma or a flat carcinoma in situ .
If either a papillary or flat tumor grows into deeper layers of the bladder, it’s called an invasive urothelial carcinoma.
Don’t Miss: What Is Papillary Urothelial Carcinoma
Noninvasive Papillary Urothelial Carcinoma High Grade
Editorial Board Members:;Bonnie Choy, M.D.Topic Completed:Minor changes:Copyright: Page views in 2020:Page views in 2021 to date:Cite this page:
- Neoplastic proliferation of the urothelium with a papillary configuration and no invasion beyond the basement membrane
- Moderate to marked architectural and cytologic atypia
- Noninvasive papillary urothelial neoplasm with moderate to marked cytoarchitectural abnormality
- Complex solid to fused papillary architecture, nuclear atypia, pleomorphism , crowded and overlapping cells, brisk mitotic activity
- Immunohistochemistry not required for diagnosis
- Commonly presents with hematuria
Also Check: Is Melanoma Skin Cancer Hereditary
How Will My Doctor Test For It
Youll need a few different tests to see if a nodule is cancer.
Physical exam. Your doctor will feel for unusual growths in your neck and ask about any symptoms you might have.
Blood tests. You may get your thyroid hormone levels checked. This wont tell you if you have cancer, but it gives more information about how your thyroid is working.
Ultrasound. Youll get this test, which uses sound waves to make a picture of things inside your body, to learn more about nodules you have. Your doctor will find out about their shape, size, and other features. That will give important clues to decide how much of a problem they are.
Biopsy. Your doctor will use a very fine needle to take a sample of the nodule to test for cancer. Typically, the most youll feel during it is a small pinch.
Youll likely get this done for any nodule thats bigger than 1 centimeter . Nodules with calcium buildup, lots of blood vessels, or without clear borders raise red flags. So do unusual-looking nearby lymph nodes bean-shaped organs that help fight infections.
Read Also: How To Remove Skin Cancer Yourself
Cystectomy Cystoprostatectomy And Pelvic Exenteration Specimens
Processing of these specimens may be summarized in three steps: orientation of the specimen and identification of relevant anatomic structures , fixation of the specimen and dissection of the specimen. Peritoneum covering the surface of the bladder is a reliable anatomic landmark. In both male and female patients, the peritoneum descends further along the posterior wall of the bladder than it does along the anterior wall. Other pelvic organs, if present, may also be used to orient the specimen. In the male, the bladder adjoins the rectum and seminal vesicles posteriorly, the prostate inferiorly, and the pubis and peritoneum anteriorly. In the female, the vagina is located posteriorly, and the uterus is located superiorly. Once the specimen is oriented, both ureters and, when present, the vasa deferentia should be identified. Location and dissection of the ureters is easier after fixation. The outer dimensions of the urinary bladder, as well as the length and diameter of ureters, should be recorded. The external surface of the bladder should be inked.
The minimum number of sections to be taken are as follows: tumor ; bladder neck , trigone , anterior wall , posterior wall , lateral walls , dome , ureteral orifices , margins , any abnormal appearing bladder mucosa and any perivesical lymph nodes .
Figure 18
Invasion Into The Lamina Propria
Urinary Bladder Tumour, Transurethral Resection: - INVASIVE HIGH-GRADE PAPILLARY UROTHELIAL CARCINOMA with lamina propria invasion.-- Muscularis propria present, NEGATIVE for muscularis propria invasion.-- NEGATIVE for lymphovascular invasion.-- Please see synoptic report.
Block letters
URINARY BLADDER LESION , TRANSURETHRAL RESECTION URINARY BLADDER TUMOUR : - INVASIVE HIGH-GRADE PAPILLARY UROTHELIAL CARCINOMA WITH LAMINA PROPRIA INVASION.- MUSCULARIS PROPRIA NEGATIVE FOR INVASIVE MALIGNANCY.- NEGATIVE FOR LYMPHOVASCULAR INVASION.
Recommended Reading: What Is Stage 4 Melanoma Cancer
Cancerous Tumours Of The Bladder
A cancerous tumour of the bladder can grow into nearby tissue and destroy it. It can also spread to other parts of the body. Cancerous tumours are also called malignant tumours.
Bladder cancer is often divided into 3 groups based on how much it has grown into the bladder wall.
- Non-invasive bladder cancer is only in the inner lining of the bladder .
- Non–muscle-invasive bladder cancer has only grown into the connective tissue layer .
- Muscle-invasive bladder cancer has grown into the muscles deep within the bladder wall and sometimes into the fat that surrounds the bladder.
Standard Treatment Options For Stage Iv Bladder Cancer
Standard treatment options for patients with T4b, N0, M0 disease
Treatment options for patients with T4b, N0, M0 disease include the following:
Chemotherapy alone or as an adjunct to local treatment
Cisplatin-based combination chemotherapy regimens are the standard of care for first-line therapy for stage IV bladder cancer in patients who can tolerate it. The only chemotherapy regimens that have been shown to result in longer survival in randomized controlled trials are MVAC, dose-dense MVAC, and CMV. GC was compared with MVAC in a randomized controlled trial and neither regimen was associated with a statistically significant difference in response rate or survival. The two regimens are generally considered equivalent, but they have never been compared in a noninferiority trial. Of note, patients with good performance status and lymph node-only disease have a low but significant rate of achieving a durable complete remission with MVAC or GC. In the large, randomized, controlled trial comparing MVAC with GC, for example, 5-year OS in patients with lymph node-only disease was 20.9%. Dose-dense MVAC and standard-dose MVAC were compared in a randomized controlled trial, and dose-dense MVAC was associated with longer survival.
Ongoing studies are evaluating new chemotherapy combinations.
Evidence :
Ongoing studies are evaluating new chemotherapy combinations.
Immunotherapy
Pembrolizumab
Evidence :
Don’t Miss: Can You Die From Basal Cell Skin Cancer
What Is Papillary Renal Cell Carcinoma
Papillary renal cell carcinoma, or PRCC, is a type of kidney cancer. The kidneys work by removing waste products from the blood. Papillary renal cell carcinoma is a cancer of the tubes that filter those waste products from the blood. There are two types of papillary renal cell carcinoma. Type 1 is more common and grows slowly. Type 2 is more aggressive and grows more quickly.;
Low Grade And High Grade
Bladder cancer can also be described as either low grade or high grade.
Low grade bladder cancer means that your cancer is less likely to grow, spread and come back after treatment. High grade means your cancer is more likely to grow spread and come back after treatment.;
For example, if you have early; bladder cancer but the cells are high grade, you’re more likely to need further treatment after surgery. This is to reduce the risk of your cancer coming back.;
Low grade is the same as;grade 1. High grade;is the same as grade 3.;Grade 2 can be split into either low or high grade. Carcinoma in situ tumours are high grade.
You May Like: How Deadly Is Squamous Cell Carcinoma
Treatment Of Bladder Cancer By Stage
Most of the time, treatment of bladder cancer is based on the tumors clinical stage when it’s first diagnosed. This includes how deep it’s thought to have grown into the bladder wall and whether it has spread beyond the bladder. Other factors, such as the size of the tumor, how fast the cancer cells are growing , and a persons overall health and preferences, also affect treatment options.