Treatment Of Ductal Carcinoma In Situ
Ductal carcinoma in situ means the cells that line the milk ducts of the breast have become cancer, but they have not spread into surrounding breast tissue.
DCIS is considered non-invasive or pre-invasive breast cancer. DCIS cant spread outside the breast, but it is often treated because if left alone, some DCIS cells can continue to undergo abnormal changes that cause it to become invasive breast cancer .
In most cases, a woman with DCIS can choose between breast-conserving surgery and simple mastectomy. But sometimes, if DCIS is throughout the breast, a mastectomy might be a better option. There are clinical studies being done to see if observation instead of surgery might be an option for some women.
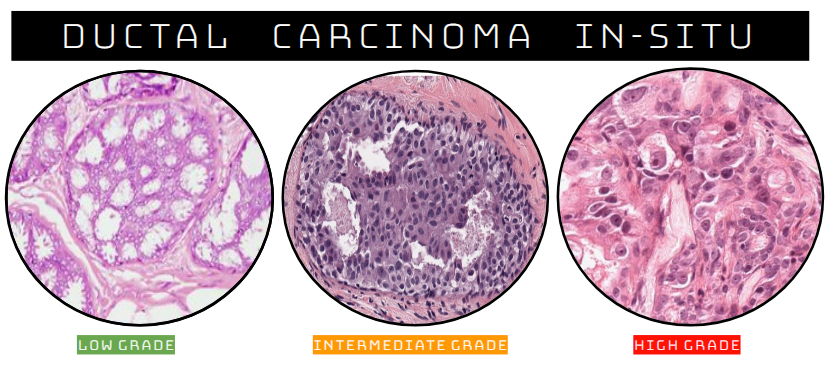
What Does It Mean If My Ductal Carcinoma In Situ Is Described As Being Low Grade Intermediate Grade Or High Grade Or Nuclear Grade 1 Nuclear Grade 2 Or Nuclear Grade 3 Or Low Mitotic Rate Intermediate Mitotic Rate Or High Mitotic Rate
These are all different ways of describing how the DCIS looks under the microscope:
- DCIS that is high grade, is nuclear grade 3, or has a high mitotic rate is more likely to come back after it is removed with surgery.
- DCIS that is low grade, is nuclear grade 1, or has a low mitotic rate is less likely to come back after surgery.
- DCIS that is intermediate grade, is nuclear grade 2, or has an intermediate mitotic rate falls in between these two.
Patients with higher grade DCIS may need additional treatment.
Patient Discussion About Ductal Carcinoma In Situ
Q. Hi all. I was diagnosed with DCIS in April. Had a lumpectomy about 3 cm and it was removed. Am I cured fully? Hi all. I was diagnosed with DCIS in April. Had a lumpectomy about 3 cm and it was removed. I then had 28 radiation and 4 boosters. I went to the cancer center for my checkup and the doctor said nothing to worry. They didnt advice me further follow up and I am normal for the past 6 months and not even taking tamoxifen. I am quite normal like others. Am I cured fully?
A.
Q. My wife is diagnosed with DCIS type of breast cancer. My wife is diagnosed with DCIS type of breast cancer. Doctors had staged my wife`s cancer as low. She is still due for some tests which she will soon have. Doctor have told that there is nothing much to worry so why are they taking so many tests?
A.
Don’t Miss: Melanoma 3c
Why Is Dcis Treated
DCIS is non-invasive, but without treatment, the abnormal cells could progress to invasive cancer over time.
Health care providers cannot predict which cases of DCIS will progress to invasive breast cancer and which will not. Because DCIS might progress to invasive breast cancer, almost all cases of DCIS are treated.
Komen Perspectives
How Common Is Ductal Carcinoma In Situ
The American Cancer Society expects that 63,960 new cases of DCIS will be found in 2018. Today more and more women are aware of the importance of early detection and are getting mammograms each year. Because of this, the number of cases of DCIS has increased. In addition, mammography technology has greatly improved as well and is better able to detect problems at an earlier stage. An estimated 12.4% of women in the U.S. will develop invasive breast cancer at some time in their lives.
Read Also: Well Differentiated Squamous Cell Carcinoma Stages
Carcinoma In Situ Vs Cancer
A million-dollar question lately, especially with controversy over the treatment of ductal carcinoma in situ or in situ breast cancer, is whether or not carcinoma in situ is really cancer. The answer is that it depends on who you talk to. Some physicians classify carcinoma in situ as non-invasive cancer and others may prefer calling it pre-cancer. The distinction would lie in knowing whether or not the CIS would progress to invasive cancer, and that, by definition, is not known. Nor are we apt to get answers soon, as it wouldn’t be ethical to simply watch large numbers of carcinoma in situ’s to see if they became invasive cancer and spread.
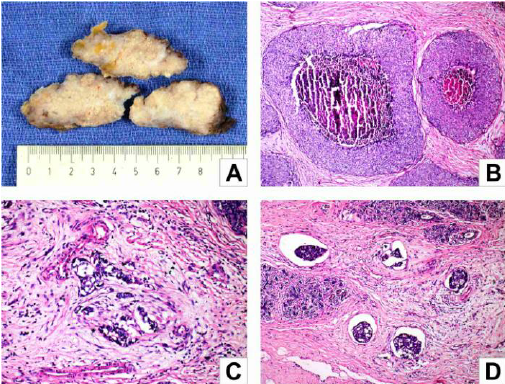
Necrosis And Calcification Are Common
When a sample of the comedo carcinoma lesion is removed for biopsy study, one will find it has a characteristic necrotic tissue with calcification, that almost feels cord-like. If the breast duct is physically squeezed, a material will be expressed which might be described as cheesy-like, almost like toothpaste. That paste is caused by the degeneration of the central cells of the early-stage tumor, and it is quite easily expressed from the rest of the tumor.
Recommended Reading: What Is The Survival Rate For Invasive Ductal Carcinoma
Hormone Therapy After Breast Surgery
If the DCIS is hormone receptor-positive , treatment with tamoxifen or an aromatase inhibitor, such as exemestane or anastrozole, for 5 years after surgery can lower the risk of another DCIS or invasive cancer developing in either breast. If you have hormone receptor-positive DCIS, discuss the reasons for and against hormone therapy with your doctor.
What Type Of Follow
Each patient is different, and the doctor will work with each individual on a follow-up plan after surgery and radiation therapy. Typically, a patient can expect to see the doctor for a physical exam every six to 12 months for five years after treatment, then annually after that. An annual mammogram will also be recommended.
Don’t Miss: Chances Of Squamous Cell Carcinoma Spreading
Meaning Of Carcinoma In Situ
In many ways, the term “carcinoma” is simply equated with cancer. Roughly 85 percent of cancers are carcinomas. Carcinomas are composed of epithelial cells the type of cells that line the skin, breast ducts, and other surfaces of organs in the body.
The subtypes of carcinomas include adenocarcinoma, squamous cell carcinoma, transitional cell carcinoma , and basal cell carcinoma.
Carcinoma in situ can be further defined by the tissue type in which cancer is beginning. For example, squamous cell carcinoma in situ of the cervix would represent a cancer that had started in squamous cells which line the cervix and has not yet become invasive.
Tumors such as sarcomas arise in tissues which do not have a basement membrane so that for these types of cancer there is not a stage of carcinoma in situ. In other words, tumors such as bone cancer do not have a pre-invasive stage and the cells would either be considered normal or cancer. Likewise, blood-related cancers, such as leukemias and lymphomas, do not have a preinvasive but cancerous stage for which people can be screened. For cancers that don’t have a CIS stage, screening tests are not as effective in early detection, because once the abnormal cells are detected, it would already be considered invasive with the potential to spread .
How Is Ductal Carcinoma In Situ Diagnosed
About 80% of cases are found by mammograms. On the mammogram, it appears as a shadowy area.
If your mammogram suggests that you may have DCIS, your doctor should order a biopsy to analyze the cells and confirm the diagnosis. Biopsies for DCIS are typically done using needles to remove tissue samples from the breast.
If you have DCIS, your doctor may do more tests to gather information about your cancer. These tests may include an ultrasound or MRI. Based on the results of various tests, your doctor will be able to tell the size of your tumor and how much of your breast is affected by the cancer.
You May Like: Skin Cancer Mayo
Are There Any Adjuvant Treatments
After surgery, you may need other treatments. These are called adjuvant treatments and can include radiotherapy and, in some cases, hormone therapy.
The aim of these treatments is to reduce the risk of DCIS coming back or an invasive cancer developing.
Chemotherapy and targeted therapy are not used as treatment for DCIS.
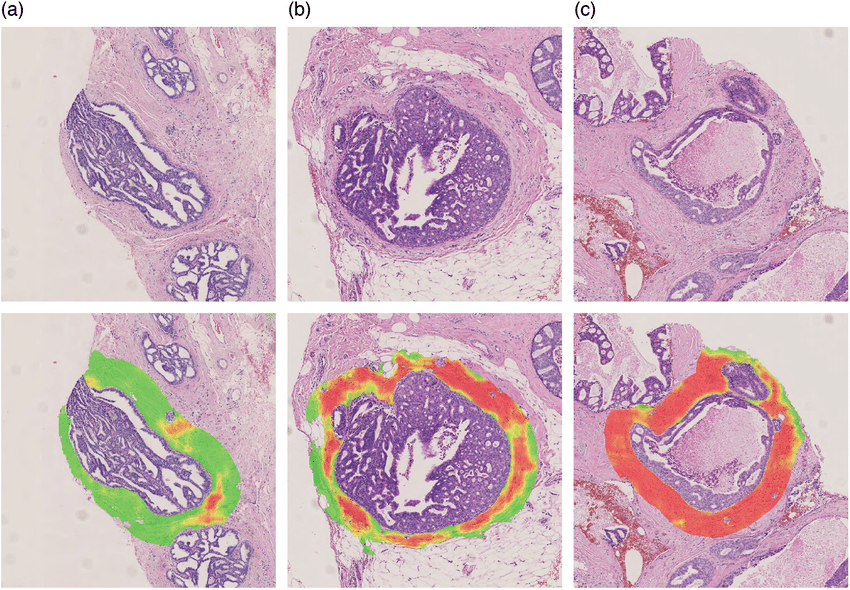
The Relationship Of Primary Dcis To Recurrences
Assessment of the clonal relationship between primary DCIS and later recurrent disease has been attempted in a number of different ways. Nuclear grade evaluation shows varying levels of concordance, with the same grade seen in 7085% of recurrences when returning as DCIS and 4953% when invasive , although better concordance with invasive grade is seen when the nuclear pleomorphism component only is considered . Immunophenotypic analyses of DCIS and recurrences have shown that recurrence as DCIS and invasive carcinoma both have high ER status concordance as well as high HER2 concordance . Immunostaining of p53 was also highly consistent .
Using such immunohistochemical and pathological features, clonality could be estimated as anywhere between 50 and 95%. However, the levels of concordance observed by these parameters do not accurately represent the clonality rate as: the assays can have poor reproducibility across time, with differing laboratory procedures and pathologist scoring leading to false non-clonality calls, caveats to using grade include that intermediate grade has low inter-observer reproducibility and that overall invasive grade is measured differently to DCIS grade, and most critically, measuring these common, low variability features is a blunt tool for positively assessing clonality: many tumors will share grade and ER status and be entirely independent tumors.
Don’t Miss: Invasive Ductal Carcinoma Breast Cancer Survival Rates
Can Dcis Be Left And Not Treated
Because theres no way of knowing when or if DCIS will become invasive, treatment is usually recommended. Its possible this may lead to unnecessary treatment for some people.
The aim of treatment is to remove all the DCIS from within the breast to reduce the chance of it becoming an invasive cancer.
Research is looking at which cases of DCIS are more likely to develop into invasive breast cancer and which could be closely monitored instead of being treated. If you are diagnosed with low-grade DCIS, you may be invited to join a clinical trial.
If you have any questions or concerns about your diagnosis and treatment, talk to your treatment team.
What Does It Mean To Have Stage 1 Breast Cancer
In Stage 1 breast cancer, cancer is evident, but it is contained to only the area where the first abnormal cells began to develop. The breast cancer has been detected in the early stages and can be very effectively treated.
Stage 1 can be divided into Stage 1A and Stage 1B. The difference is determined by the size of the tumor and the lymph nodes with evidence of cancer.
Also Check: Invasive Ductal Breast Cancer Prognosis
How Is Dcis Classified
Grade
DCIS can be classified by grade. The lower the grade, the more the cancer cells look like normal breast cells. Lower grades also tend to grow more slowly. Sometimes the cells might be a mix of grades, which may be called borderline cells. The grades of DCIS are:
- Grade I – The cancer cells look a lot like normal breast cells under a microscope.
- Grade II – These cells grow faster than normal breast cells and look a little less like the normal cells.
- Grade III – These cells grow faster and look much different than normal breast cells. People with high-grade cancers have a higher chance of developing invasive breast cancer in the future or having the current cancer come back after treatment.
Appearance
DCIS cells are further identified by their pattern or shape when looked at under the microscope, classifying them into subtypes. Many tumors will be a mix of two or more subtypes. These subtypes are:
Low or Moderate Grade:
- Papillary- The cancer cells in the duct look finger-like.
- Micropapillary- A type of papillary where the cells are very small.
- Cribiform- Spaces or gaps are seen between the cancer cells in the duct.
- Solid- There is a solid collection of cancer cells without spaces between them.
High Grade:
- Comedo- There is a solid collection of cancer cells, with an area in the middle that is made up of dead cells . The cancer cells build up quickly within the duct and some cells inside the tumor lose their blood supply, causing necrosis.
Hormone Status
Additional Types Of Invasive Ductal Carcinoma:
There are four types of invasive ductal carcinoma that are less common:
- Medullary Ductal Carcinoma This type of cancer is rare and only three to five percent of breast cancers are diagnosed as medullary ductal carcinoma. The tumor usually shows up on a mammogram and it does not always feel like a lump rather it can feel like a spongy change of breast tissue.
- Mucinous Ductal Carcinoma This occurs when cancer cells within the breast produce mucous, which also contains breast cancer cells. The cells and mucous combine to form a tumor. Pure mucinous ductal carcinoma carries a better prognosis than more common types of IDCs.
- Papillary Carcinoma This is a very good prognosis breast cancer that primarily occur in women over the age of 60.
- Tubular Ductal Carcinoma This is a rare diagnosis of IDC, making up only two percent of diagnoses of breast cancer. The name comes from how the cancer looks under the microscope like hundreds of tiny tubes. Tubular breast cancer has an excellent prognosis.
Show me moreâ¦
Read Also: What Is Merkel Cell Skin Cancer
You May Like: Invasive Ductal Carcinoma Grade 1 Survival Rate
Diagnosis And Pathology Of Dcis
Ductal carcinoma in situ is a proliferation of atypical epithelial cells that is contained within the lumen of the breast ductal system. Nowadays, it is usually detected in the context of a mammographic screening program, but can occasionally present as a palpable lump or with other physical symptoms like nipple discharge . Approximately 8% of core needle biopsies are initially diagnosed as DCIS , and this diagnosis is confirmed in ~74% of cases after excision. A recent meta-analysis found that under-diagnosis on core biopsy was associated with large tumor size, palpable mass, a mammographic mass lesion, use of image guidance other than stereotactic, and high mammographic density .
In addition to nuclear atypia, a range of different architectural patterns are observed, including cribriform, solid, comedo , micropapillary, and papillary . Multiple patterns are often observed within the same tumor , which may explain the low level of concordance of studies using these categories as prognostic markers. The prognostic value of these architectural features has been found to be limited comedo necrosis is associated with high grade and worse breast cancer-specific survival but only inconsistently with recurrence . The increase in incidence of DCIS after the introduction of mammographic screening has been more strongly associated with an increase in the non-comedo subtypes .
Understanding Ductal Carcinoma In Situ
Most women diagnosed with this noninvasive breast cancer are alive 10 years later, and better treatments are emerging.
For the 62,000 women who will be diagnosed with ductal carcinoma in situ this year, the good news is far more important than the bad. While cancer is never a picnic, DCIS is the earliest detectable form of the disease. Some news that sounds “bad” for instance, that the incidence of DCIS is increasing faster than that of any other type of breast cancer is encouraging news. It means that more breast cancers are being detected early, while they can be nipped in the bud. Today, with standard treatment, 10-year survival rates for DCIS are approaching 100%, and the treatment is usually not too difficult to tolerate.
Read Also: Ductal Breast Cancer Survival Rates
Comedo Carcinoma Of The Breast
Comedo carcinoma of the breast is actually a type of ductal carcinoma in situ. It is considered to be an early stage of breast cancer, and it is characterized by the presence of central necrosis, or evidence of cell death and decay. A diagnosis of this particular kind of breast cancer is somewhat fortuitous as it is confined to the breast ducts and usually does not spread beyond. However, in terms of the various kinds of DCIS, comedo carcinoma is considered to be of a higher grade and a little more aggressive than the others, and may be treated a little more aggressively.
This page is still has some very helpful information, but check out our new and improved up-to-date page on Comedo Carcinoma.
Future Directions In Dcis
DCIS research is directed mainly at improving treatment and, above all, at preventing progression to invasive disease. As researchers continue to study the pathology of DCIS, they are finding that certain tumor characteristics help predict the treatment most likely to reduce the chance of recurrence. For example, some forms of breast cancer require estrogen in order to grow tumors that do are termed estrogen receptorpositive . Tamoxifen belongs to a class of drugs called selective estrogen-receptor modulators , which act by blocking estrogen receptors. Tamoxifen is more likely to prevent a recurrence in women with ER-positive DCIS than in women with ER-negative disease.
The use of aromatase inhibitors, which block estrogen production in the peripheral tissues and breast tissue, is being investigated in a trial of postmenopausal women with ER-positive DCIS. For women whose DCIS is ER-negative but who have the HER-2/neu gene, researchers are exploring the use of trastuzumab and lapatinib , which block the tumor growth factors produced by that gene.
A new way to administer radiation that is showing some promise in clinical trials is accelerated partial breast irradiation, in which the tumor site alone is treated for five days with a lighter dose of radiation. In another approach, intraoperative radiation therapy, a one-time dose of radiation is delivered to the involved area of the breast after the tumor has been removed but before the incision is closed.
Read Also: Stage 2 Invasive Ductal Carcinoma Survival Rate
After Surgery What Other Treatments Might Be Needed
For those who have a mastectomy for DCIS, there is usually no need for additional treatment because the risk of the cancer coming back is very low. After a lumpectomy, there is still a risk that the DCIS may come back or become invasive cancer. To reduce this risk, the two main treatments are radiation therapy and, if the DCIS cells have the estrogen receptor, hormone therapy. These hormone-blocking drugs include tamoxifen, which blocks the estrogen receptor, and aromatase inhibitors, which block estrogen production.
Probably the hardest decision faced by people with DCIS is whether to have one of these additional treatments after a lumpectomy. A lot of factors must be considered, including the size and grade of the DCIS, how close the DCIS cells were to the final margin, and the age of the person at diagnosis. Younger patients tend to have a higher risk of recurrence compared to older individuals. And then as a doctor, I need to consider how each of my patients thinks about risk. For example, a 10% risk of recurrence in the next ten years can mean completely different things to two different people. Some patients want to do everything to lower their risk, while others are happy to just have it watched closely.