What Are The Signs Of Metastatic Squamous Cell Carcinoma
Squamous cell carcinoma at any stage can appear as a scaly red patch, a firm nodule or a flat or raised sore that may crust over. Because the appearance of this cancer can vary considerably, its a good idea to consult with a physician if any skin abnormalities develop. Squamous cell carcinoma is more likely to appear on skin that is exposed to sunlight, such as on the face or neck, although it sometimes occurs on the bottom of feet, inside the mouth or around the genitals.
Metastatic squamous cell carcinoma is often referred to as a neck cancer because it tends to travel to the lymph nodes in the neck and around the collarbone. Because of this, signs of metastasis may include a painful or tender lump in the neck or a sore throat that doesnt improve or go away.
What Is A Squamous Cell Carcinoma Of The Skin
Squamous cell carcinoma is a tumor of skin cells. As shown in the illustration, the skin is made up of several layers of cells with the squamous layer at the top. Given that this type of cancer arises from squamous cells, tumors can develop anywhere that these cells are present. This can include the nail bed, ear tips , nose, and corner of the eyes.
Squamous cell carcinomas usually present as a single, solitary lesion in one location, but there is a kind of SCC called multicentric squamous cell carcinoma that presents as many lesions in multiple locations on the body, including the mouth. Multicentric SCC is rare in cats.
The Role Of Fine Needle Aspiration Biopsy Core Biopsy And Open Biopsy
If a primary site is not identified on clinical examination, the next step will be FNA of the neck mass for cytological examination, preferably under ultrasound guidance . For patients with solid masses that harbor squamous cell carcinoma, FNA will be positive in 80% or more and repeated FNA can yield an additional increment. With cystic neck masses the percentage is lower, but still, if ultrasound assisted and directed toward the most solid parts of the lesion, in the majority of patients with a suspicious neck mass, the FNA will correctly diagnose malignancy if present.
In those cases which are not squamous cell carcinomas, and in particular when a primary below the clavicles is suspected, sophisticated diagnostic approaches, including immunocytochemistry or immunohistochemistry and molecular techniques are available to help direct a search for a primary site, based on the biopsy, and this is covered in more detail later.
The possibility of applying additional cytopathological and molecular techniques to the cytologic aspirate, to provide an estimate regarding the risk of malignancy relative to a benign branchial cleft cyst, is an area that is open for further study. If a few non-diagnostic cells are encountered, IHC or in-situ hybridization Epstein Barr Virus , P53 mutations , cytokeratin and other markers can be performed, depending on the viral prevalence in the region and level of suspicion.
Don’t Miss: Cancer Spread All Over Body
Definition Of Metastatic Neck Carcinoma In The Neck With Unknown Primary
Many patients with cervical lymphatic metastases start out as unknown primaries, but most have primaries identified on careful physical examination, office endoscopy, and imaging . Only after such an evaluation can patients be categorized as neck cancer with an unknown primary . We introduce more specific abbreviation NCUP rather than CUP, which is also commonly used for widespread systemic cancer metastases below the clavicles with unknown primary.
NCUP occurs in 1 to 7% of new head and neck cancer cases, and that percentage declines with the extensiveness of the search for a primary . After extensive endoscopic evaluation under general anesthesia, the percentage of unknown primary tumors decreases to less than 3%, . Some have suggested that the incidence of patients with NCUP is increasing with the increasing numbers of HPV-related oropharyngeal cancers .
Isolated supraclavicular nodes , on the other hand, are either of thyroid origin or metastatic from primary sites below the clavicles, the classic Virchows node, which include gastrointestinal tract, urogenital tract, esophagus, biliary, liver, pancreas, lung, breast, and gynecological cancers . Even rarer malignant neck masses include soft tissue sarcomas and cervical metastases from central nervous system tumors .
Squamous Cell Carcinoma Causes
Exposure to ultraviolet rays, like the ones from the sun or a tanning bed, affects the cells in the middle and outer layers of your skin and can cause them to make too many cells and not die off as they should. This can lead to out-of-control growth of these cells, which can lead to squamous cell carcinoma.
Other things can contribute to this kind of overgrowth, too, like conditions that affect your immune system.
Also Check: Does Skin Cancer Burn And Itch
Citation Doi And Article Data
Citation:DOI:Dr Divya SaanjRevisions:see full revision historySystem:
- Squamous cell carcinoma in mature cystic teratoma
- Squamous cell carcinoma arising from mature cystic teratoma
- SCC ovary
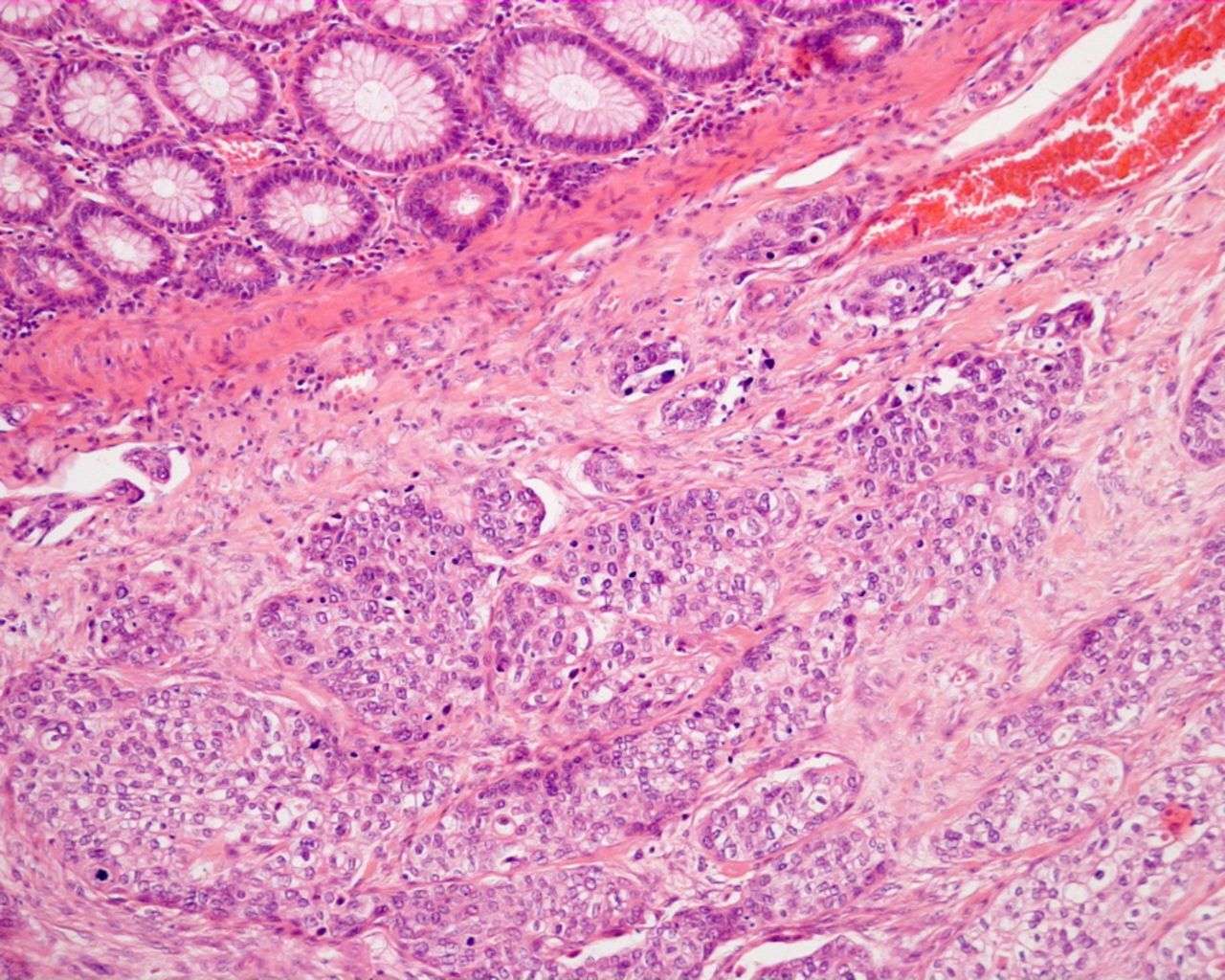
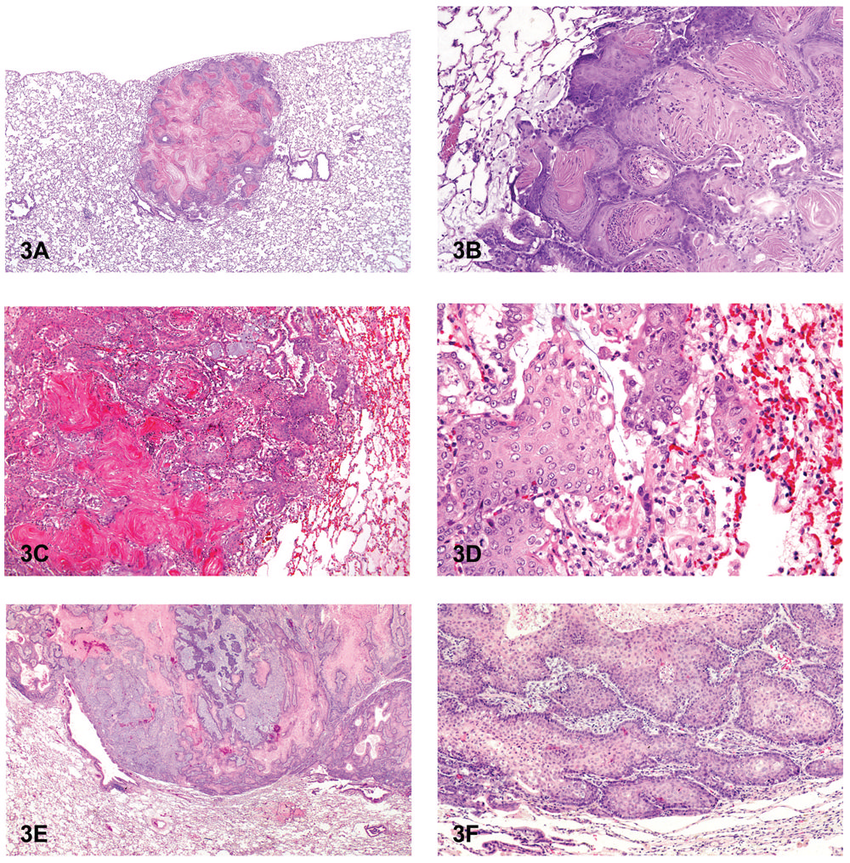
Squamous cell carcinoma of the ovary is extremely rare and usually arises in a mature cystic ovarian teratoma2. As only parts of the lesion are composed of malignant tissue, it is difficult to diagnose malignant transformation of a teratoma preoperatively, unless invasion into adjacent structures is present.
How Is This Cancer Diagnosed
Depending on where the tumor develops , a diagnosis may be achieved with a fine needle aspiration . FNA involves taking a small needle with a syringe and suctioning a sample of cells directly from the tumor and placing them on a microscope slide. A veterinary pathologist then examines the slide under a microscope.
In some cases, results from FNA may not be entirely clear and biopsy may be necessary. A biopsy is a surgical excision of a piece of the tumor. Pieces of the tumor are then examined by a veterinary pathologist under the microscope. This is called histopathology. Histopathology is not only helpful to make a diagnosis but can indicate how the tumor is likely to behave.
In cases of tumors of the toe, X-rays may be especially helpful with making a diagnosis. In cats, about 90% of carcinomas of the toes are actually cancer that had spread to the toe from the lungs. Lung cancer in cats tends to selectively spread to the nailbeds and toes. This is called lung-digit syndrome. X-rays of the chest, therefore, are necessary to determine if the tumor in the toe area is truly SCC of the toe or if it is secondary to a lung cancer.
Also Check: How To Identify Basal Cell Carcinoma
Stages Of Squamous Cell Carcinoma
- print page
- Bookmark for later
Cancer staging is a way of describing how extensive a cancer is. The stage is related to tumor size. It also relates to whether the cancer has spread from the original tumor to other parts of the body. The cancer stage helps you and your doctor to develop a treatment plan. It also provides information about survival. Squamous cell carcinoma stages use a system called TNM.1,2 This cancer staging system is used by most hospitals and medical systems.3 Once your doctor has categorized the T, N, and M, these values are combined to assign a cancer stage.2
Squamous Cell Carcinoma Pathology
open
App to facilitate skin self-examination and early detection. Read more.
Squamous cell carcinoma is common form of keratinocytic skin cancer, usually related to exposure to ultraviolet radiation from sunlight. It often arises within solar/actinickeratosis or within squamous cell carcinoma in situ.
Don’t Miss: What Is The Prognosis For Skin Cancer
Treating Squamous Cell Carcinoma Of The Skin
Treatment options for squamous cell skin cancer depend on the risk of the cancer coming back, which is based on factors like the size and location of the tumor and how the cancer cells look under a microscope, as well as if a person has a weakened immune system.
Most squamous cell skin cancers are found and treated at an early stage, when they can be removed or destroyed with local treatment methods. Small squamous cell cancers can usually be cured with these treatments. Larger squamous cell cancers are harder to treat, and fast-growing cancers have a higher risk of coming back.
In rare cases, squamous cell cancers can spread to lymph nodes or distant parts of the body. If this happens, treatments such as radiation therapy, immunotherapy, and/or chemotherapy may be needed.
Primary Intraosseous Squamous Cell Carcinoma Of The Maxilla Possibly Arising From An Infected Residual Cyst: A Case Report
This article is mentioned in:
Abstract
Introduction
A primary intraosseous odontogenic carcinoma, whichis a term that was recommended by the World Health Organization in 1972 is a type ofsquamous cell carcinoma arising within the jawbone thatpurportedly develops from remnants of odontogenic epithelium. In2005, the WHO classified these lesions as odontogenic carcinomas,termed primary intraosseous SCC , and divided them intothree types: solid type keratocystic odontogenic cyst-derived andodontogenic cyst-derived . Adefinitive diagnosis of PIOSCC is difficult as the lesion must bedistinguished from tumors that have metastasized to the jawbonefrom distant sites, from alveolar carcinomas that have invaded thebone from the surface and from tumors of maxillary origin .
Odontogenic cysts are true cysts that arise from thedental epithelium, which is associated with tooth formation. Theepithelial lining of odontogenic cysts has the potential totransform into various types of odontogenic tumor .However, transformation from an odontogenic cyst to a malignanttumor is rare .
Case report
Discussion
Also Check: Melanoma Braf Positive
What Causes This Cancer
The reason why a particular cat may develop this, or any cancer, is not straightforward. Very few cancers have a single known cause. Most seem to be caused by a complex mix of risk factors, some environmental and some genetic or hereditary. Exposure to ultraviolet rays/sunlight has been attributed to the development of SCC in cats. Exposure to papilloma-like viruses also appears to contribute to multicentric SCC in the mouth and other areas of the skin where squamous cells are present.
White and light-colored cats are more likely to get these tumors. A risk has been reported in Siamese, Himalayan, and Persian breeds, likely related to their protective pigment.
How Can I Prevent Scc
Reducing ultraviolet exposure will reduce the risk of getting an SCC.
Top sun safety tips
- Protect your skin with clothing, and dont forget to wear a hat that protects your face, neck and ears, and a pair of UV protective sunglasses.
- Spend time in the shade between 11am and 3pm when its sunny. Step out of the sun before your skin has a chance to redden or burn. Keep babies and young children out of direct sunlight.
- When choosing a sunscreen look for a high protection SPF to protect against UVB, and the UVA circle logo and/or 4 or 5 UVA stars to protect against UVA. Apply plenty of sunscreen 15 to 30 minutes before going out in the sun, and reapply every two hours and straight after swimming and towel-drying.
- Sunscreens should not be used as an alternative to clothing and shade, rather they offer additional protection. No sunscreen will provide 100% protection.
- It may be worth taking Vitamin D supplement tablets as strictly avoiding sunlight can reduce Vitamin D levels. You should consult your doctor about this.
Treatment of areas of scaly sun damage may reduce your risk of an SCC.
Recommended Reading: What Is The Most Aggressive Skin Cancer
Features Of T Categories
The T categories describe the main tumor based on its thickness, the presence of high-risk features, and invasion.2 Your doctor begins to gather this information by doing a skin biopsy. If the tumor is invasive, you will need imaging tests.
- Size. The longest dimension of the tumor is measured in centimeters.
- Invasion. The tumor is categorized by how far it has invaded the body. Invasion of the facial bones is categorized as T3. Invasion of bones in the rest of the body or the base of the skull is T4. Your doctor determines this using magnetic resonance imaging or computed tomography scan.
- High-risk features. High-risk features refer to the risk that the cancer returns or spreads . High-risk features of SCC are:2
- > 2 mm thick or Clark level IV
- Growing around a nerve
- Located on the ear or lip
- Poorly differentiated or undifferentiated cells. Differentiation means how much the cancer cells look like the normal tissue that it came from. Poorly differentiated cells grow and spread more quickly.
How Is Metastatic Squamous Cell Carcinoma Treated
Each patients ideal course of metastatic squamous cell carcinoma treatment will vary according to the location of the primary cancer, how far it has spread, the overall health of the patient and several other factors. Many treatment plans include a combination of surgery to remove skin lesions and affected lymph nodes, as well as chemotherapy and radiation therapy to help shrink or destroy cancer cells that have traveled to other parts of the body.
Moffitt Cancer Centers Cutaneous Oncology Program offers a full spectrum of diagnostics and leading-edge treatment options to patients with squamous cell carcinoma of any stage. To speak with a Moffitt oncologist specializing in skin cancer, submit a new patient registration form online or call .
- BROWSE
You May Like: What Is The Survival Rate For Invasive Ductal Carcinoma
Evaluation By The General Practitioner
Hayes Martin stated that an adult patient who presents with a palpable lateral neck mass, whether solid or cystic, should be considered to have a metastatic lymph node until proven otherwise .
In the typical patient with NCUP, the lymph nodes, located in the upper part of the neck, are clearly abnormal in size, shape or consistency. The palpable mass may be firm or, if cystic, may have a tense or soft consistency. On careful questioning, the patient may have symptoms referable to a head and neck primary tumor, such as a sore throat when swallowing, ear pain, new nasal obstruction, voice change, etc. They also may have a history of tobacco and alcohol abuse or 10 or more lifetime sexual partners. The absence of suspicious history or symptoms does not, however, rule out cancer.
If a patient has a clinical presentation and imaging typical of lymphoma, with widespread adenopathy, sometimes exhibiting splenic, liver, bone marrow or lung involvement, and sometimes with type B constitutional symptoms , this represents an appropriate clinical scenario for open cervical lymph node biopsy . If not, it would be preferable to presume carcinoma initially and avoid open or even core biopsy as an initial test.
Ultrasound-guided FNA of the neck mass for cytology is also appropriate prior to referral, but core needle biopsy should be deferred until after evaluation by the specialist and complete head and neck physical examination including fiberoptic nasopharyngo-laryngoscopy .
Health Literacy To Empower Patients
With the right information, patients can make the best decisions about their care. By partnering with patients, healthcare providers, and hospitals, we hope to provide all patients with the tools and knowledge to understand their pathology report.
For more information about this site, contact us at .
Disclaimer: The articles on MyPathologyReport are intended for general informational purposes only and they do not address individual circumstances. The articles on this site are not a substitute for professional medical advice, diagnosis or treatment and should not be relied on to make decisions about your health. Never ignore professional medical advice in seeking treatment because of something you have read on the MyPathologyReport site. MyPathologyReport is independently owned and operated and is not affiliated with any hospital or patient portal. The articles on MyPathologyReport.ca are intended for use within Canada by residents of Canada only.
Copyright © 2020. All rights reserved. Privacy Policy
Our work is generously supported by:
Don’t Miss: What Is The Survival Rate For Invasive Ductal Carcinoma
Incidence And Clinical Predictors Of Cystic Squamous Cell Carcinoma Metastases In Lateral Cervical Cysts
Published online by Cambridge University Press: 22 April 2019
- Department of Otorhinolaryngology Head and Neck Surgery, Medical Faculty, Comenius University in Bratislava, Slovakia
- N Gnojcakova
- Department of Otorhinolaryngology, University Hospital, Nové Zámky, Slovakia
- F Kurinec
- Department of Otorhinolaryngology, University Hospital, Nové Zámky, Slovakia
- M Profant
- Department of Otorhinolaryngology Head and Neck Surgery, Medical Faculty, Comenius University in Bratislava, Slovakia
- *
What Is Metastatic Squamous Neck Cancer
Metastatic squamous neck cancer develops in squamous cells and eventually spreads to lymph nodes in the neck. Squamous cells are present in many different organs throughout the body, including the lungs, kidneys, skin, cervix and esophagus. When squamous cell cancer develops in any of these organs, the cancerous cells can potentially spread to nearby lymph nodes, enter the lymphatic system and travel to distant areas of the body. If cancerous squamous cells settle in the tonsils, nasopharynx, base of the tongue or lymph nodes in the neck, the condition is known as metastatic squamous neck cancer.
Don’t Miss: Invasive Ductal Carcinoma Survival
What Causes A Squamous Cell Carcinoma
The most important cause is too much exposure to ultraviolet light from the sun or other sources. This can cause the DNA of skin cells in the outer layer of the skin to change. Sometimes this alteration in DNA allows the skin cells to grow out of control and develop into an SCC. Ultraviolet light damage can cause SCC directly, or sometimes it can induce a scaly area called an actinic keratosis or Bowens disease. These can change into SCC if they are not treated.
Squamous cell carcinomas can also develop in skin damaged by other forms of radiation, in burns and persistent chronic ulcers and wounds and in old scars. Certain human viral wart viruses can also be a factor. However, SCC itself is not contagious.