What Is Clear Cell Carcinoma Of Endometrium
- Clear Cell Carcinoma of Endometrium is a rare subtype of endometrial cancer, which begins in the lining of the uterus . The majority of these cancer cases are detected and diagnosed in women aged 50 years and older
- Based on the grade and degree of aggressiveness, Clear Cell Carcinoma of Endometrium is mostly categorized as a high-grade tumor that is typically aggressive in nature. In many cases, these tumors are diagnosed in their later stages
- A variety of factors are known to influence the development of Clear Cell Carcinoma of Endometrium including smoking, positive family history of endometrial cancer, and polycystic ovarian syndrome. The exact cause of the cancer is unknown, but it may be due to certain genetic abnormalities
- The majority of Clear Cell Carcinoma of Endometrium cases are detected and diagnosed at an early stage due to frequent abnormal vaginal bleeding, which is a major indicative sign. Additional signs and symptoms may include pelvic pain, pain during sex, and urination difficulties
- If Clear Cell Carcinoma of Endometrium is diagnosed early, then a surgical removal of the uterus may help eliminate the cancer. The prognosis depends on the stage of the tumor. However, in general, Clear Cell Carcinoma of Endometrium has a poorer prognosis compared to endometrioid adenocarcinomas
How Is Clear Cell Carcinoma Of Endometrium Diagnosed
There is a variety of tests healthcare providers may use to detect, locate, and diagnose Clear Cell Carcinoma of Endometrium, and assess if it has potentially spread to other regions. A surgical procedure called a biopsy is the main test a healthcare provider relies on to make a definitive diagnosis of Clear Cell Carcinoma of Endometrium.
The diagnostic tools may include:
- A thorough physical examination and a complete medical history evaluation is very vital to the diagnosis
- Pelvic examination: During a pelvic examination, a physician exams the uterus, vagina, ovaries, fallopian tubes, bladder, and rectum to check for any abnormal changes in these organs
- Complete blood count with differential of white blood cells
- Liver function test
- Inhibin
- Estrogen and testosterone levels
Note:
What Is Clear Cell Carcinoma
Clear cell carcinoma , also sometimes called clear cell cancer, is a rare type of tumor characterized by cells that are clear or pale in color. These cells have a solid boundary and tend to be either filled with fluid or glycogen, a form of glucose. This type of cell can be found in many different types of tumors, but they are often found in the female reproductive system and lower urinary tract.
Areas of the Body Affected by CCC
Carcinoma tumors arise from epithelial cells, which are cells that make up the surface of body tissue and cavities. Clear cell carcinoma, therefore, can be found throughout the body in both men and women in the breasts on the skin in the lower urinary tract, particularly the kidney or the organs of the female reproductive system, including the ovaries, vaginal tract, and uterus.
Clear cell renal carcinoma, also known as renal cell carcinoma , originates in the renal tubules of the kidney. These are the small tubes that remove waste products from the blood. RCC is a very common type of kidney tumor nine out of ten kidney tumors are of this type, and seven out of ten of RCC tumors are clear cell tumors.
Don’t Miss: Invasive Ductal Breast Cancer Prognosis
Talk With Others Who Understand
MyOvarianCancerTeam is the social network for people with ovarian cancer. On MyOvarianCancerTeam, more than 8,900 members come together to ask questions, give advice, and share their stories with others who understand life with ovarian cancer.
Have you been diagnosed with ovarian clear cell carcinoma? Share your experiences in the comments below, or start a conversation by posting on your Activities page.
Clinical Characteristics Of Patients With Occc
Patients with OCCC usually examined with a huge unilateral pelvic mass confined to the ovary, accompanied by abdominal pain and swelling symptoms with a mild-to-moderate elevation of serum CA125 . Particularly, they are likely to develop hypercalcemia , resulted from the elevated expression of the parathyroid-hormone-related protein and the activation of stanniocalcin-1 signaling mediated by IL-6 .
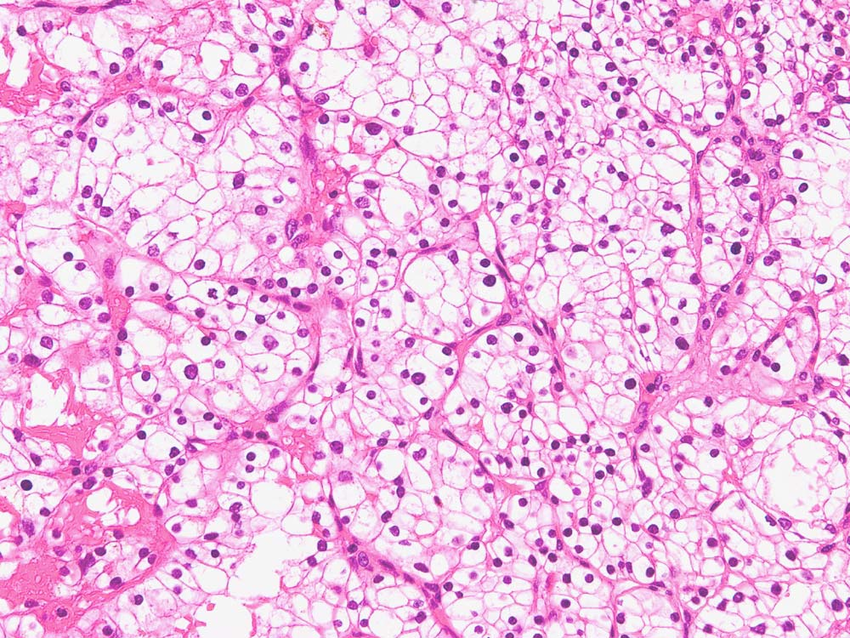
Pathologically the OCCC lesions are usually present as huge masses consist of solid tissue that protrudes into the cyst cavity and commonly displays a combination of papillary, tubulocystic, and solid microscopic patterns. The tumor invades the ovarian interstitium, causing desmoplasia, stromal destruction, hyalinization, desmoplasia and confluence of the epithelial elements. . The presence of clear cells alone could not directly confirm OCCC because clear cytoplasm could also be found in cells of ovarian endometrioid carcinoma and HGSC. OCCC characteristically contains clear or hobnail cells with eccentric, rounded, and bulbous nuclei, multiple complex papillae, densely hyaline basement membrane material, and hyaline bodies. Compared with other types of EOC, the frequency of mitoses is lower .
Read Also: What Does Cancer Look Like Outside The Body
B What Complications Could Arise As A Consequence Of Management Of Chemotherapy Radiation And/or Surgery
Surgery
Complications of surgery for UPSC and CC carcinoma depend in part on whether the surgery is performed at the time of initial diagnosis or for recurrent disease. Staging procedures for endometrial cancer are associated with both short-term and longer term sequelae. The GOG LAP-2 trial does provide us with some of the best prospective data regarding operative complications. While one cannot extrapolate from the laparoscopic results to robotic assisted laparoscopy, they should not be expected to be significantly different. Table 3 lists a select representation of the most usual complications:
Table 3.
Immunohistochemical Staining And Scoring
Tumors were scored positive for LDHA if tumor cells showed definite nuclear and/or membranous staining and negative if tumor nuclei and cell membrane had no immunoreactivity. A combination of a proportion score and an intensity score was used to assess LDHA immunostaining: the proportion score was: 0: none, 1: 1-24%, 2: 25-49%, 3: 5074, 4: 75%. The intensity score was: 0: none, 1: weak, 2: moderate, 3: strong. Three cases were used as calibrators to define intensity. A total score was obtained by the combining both scores. Cores were evaluated independently by two pathologists and controversial cases were assigned a consensus score after discussion. Representative micrographs of immunostaining are shown in Figure 1.
Representative photomicrographs showing the expression of LDHA protein by immunohistochemistry. Normal kidney proximal tubular epithelium, weak, moderate, and strong staining Clear Cell Renal Cell Carcinoma .
Read Also: What Is The Survival Rate For Invasive Lobular Carcinoma
What Are The Causes Of Clear Cell Carcinoma Of Endometrium
The exact cause and mechanism of formation of Clear Cell Carcinoma of Endometrium is unknown. Some researchers believe that the tumor occurs due to genetic mutations within the cells in the endometrium .
- In general, it is known that cancers form when normal, healthy cells begin transforming into abnormal cells – these cancer cells grow and divide uncontrollably , resulting in the formation of a mass or a tumor
- The transformation of normally healthy cells into cancerous cells may be the result of genetic mutations. Mutations allow the cancer cells to grow and multiply uncontrollably to form new cancer cells
- These tumors can invade nearby tissues and adjoining body organs, and even metastasize and spread to other regions of the body
Currently, medical research is being conducted to determine the exact cause of Clear Cell Carcinoma of Endometrium.
How Can Clear Cell Carcinoma Of Cervix Be Prevented
Some steps for the prevention of Clear Cell Carcinoma of Cervix include:
- Even though DES-exposure was responsible for many cases of Cervical Clear Cell Carcinoma earlier, the use of DES is decreasing steeply and the incidence of cancer caused by DES-exposure is on the decline worldwide
- Avoidance of smoking
- Regular screening to detect precancers:
- The American Cancer Society recommends screening of women from age 21 years
- A Pap smear is recommended every 3 years, from ages 21-29 years
- From age 30-65 years, a Pap smear and HPV testing is recommended, once every 5 years
- More frequent screenings are advised for women having a high-risk for cervical cancer
Read Also: Well Differentiated
What Is The Prognosis For People With Ccrcc
The estimate of how a disease will affect you long-term is called prognosis. Every person is different and prognosis will depend on many factors, such as
- Where the tumor is in your body
- If the cancer has spread to other parts of your body
- How much of the tumor was taken out during surgery
If you want information on your prognosis, it is important to talk to your doctor. NCI also has resources to help you understand cancer prognosis.
Doctors estimate ccRCC survival rates by how groups of people with ccRCC have done in the past. Because there are so few pediatric ccRCC patients, these rates may not be very accurate. They also dont take into account newer treatments being developed.
With this in mind, ccRCC patients with smaller tumors have a better chance of survival than patients with larger tumors. The 5-year survival rate for patients with ccRCC is 50-69%. When ccRCC is already large or has spread to other parts of the body, treatment is more difficult and the 5-year survival rate is about 10%.
Related Resources
What Is The Survival Rate For Clear Cell Renal Cell Carcinoma
As many as 7 in 10 people with small ccRCC tumors are alive five years after the initial diagnosis. Treatment is less effective on large tumors or metastatic cancer. In those cases, five-year survival rates may drop to about 1 in 10. A cancer prognosis depends on many factors, including:
- Cancer spread.
- Location, size and number of tumors .
Read Also: Invasive Ductal Carcinoma Survival Rate Stage 3
Clear Cell Carcinoma Treatment: The Water Cures
On getting in touch with the Water Cures staff and getting a hydration coach, the family was instructed on what to do. They were scared, and not fully on-board yet.
She started to change what she ate, what and how she drank, and putting salt on her tongue. She took two 45 minute baths a day adding unprocessed sea salt to the bath.
She was following the Water Cures protocol in addition to chemo therapy. On the check up after the third chemo treatment….her cancer was reduced over 50%. The Doctor, very surprised, thought the test may have been inaccurate. Asking for the original scan and viewing the original side by side with the latest, he confirmed the 50% reduction. It should also be noted that mom never had to be hospitalized, never got an infection, and only experienced minimal side effects. For the most part, aside from typical discomforts, she went through all treatments pretty smoothly.
Betty completed the 6th and last chemo treatment and looks wonderful. She never had to be admitted into the hospital, was never given blood of any form, and never got an infection. She did not even experience the mouth sores that most get. The side effects she experienced were being very tired, nausea at times, lack of appetite on occasion, hair loss. According to Betty, there were times when it was painful, even her eyelids hurt.
One of her grandsons offered to give her his hair from a visit to the barber shoppe since she lost hers, including her eyelashes.
Molecular And Genetic Aspects Of Ccrcc
Studies in patients with VHL disease established the importance of genetic alterations involving chromosome 3p in the development of CCRCC, while subsequent research has shown that chromosome 3 or 3p is lost in 80-98% of sporadic CCRCCs.
Inactivation or loss of the VHL gene results in the absence of a functional VHL protein, which under normoxic conditions usually targets the alpha subunit of the transcription factor hypoxia-inducible factor for degradation. Loss of functional VHL protein therefore leads to accumulation of HIF and activation of its hypoxia-inducible target genes under normoxic rather than hypoxic conditions. HIF target genes include the vascular endothelial growth factor gene VEGF, which may explain the prolific angiogenesis associated with CCRCC.
A less common pathway followed in 18% of CCRCCs mainly involves gains of entire chromosomes resulting in a hyperdiploid karyotype. Common gains involve chromosomes 7 , 16 , 20 , 12 , and 2 . This second pathway is similar to the genetic events seen in papillary RCC, except that most papillary RCCs also show gain of chromosome 17.
Progression of CCRCC can eventually involve reduplication of the entire genome to give a polyploid karyotype, followed by further losses or gains of genetic material. Complex polyploid karyotypes are particularly common in tumors with sarcomatoid differentiation.
Don’t Miss: Invasive Ductal Carcinoma Survival Rate Stage 4
Clear Cell Carcinoma Stages
Your doctor can also determine the cancer stage during surgery. The stage describes whether cancer has begun to spread. Doctors use a system called FIGO to classify ovarian cancer into four stages. Cancer stages are sometimes represented with Roman numerals, as stages I through IV. FIGO stage 1 is the least advanced and stage 4 is the most advanced:
- Stage 1 Cancer cells are located in one or both ovaries or fallopian tubes.
- Stage 2 Cancer cells have spread to nearby tissues in the pelvis such as the uterus.
- Stage 3 Cancer cells are found in the lymph nodes or tissues in the abdomen.
- Stage 4 Cancer cells have spread outside of the pelvis and abdomen.
OCCC is more likely to be diagnosed at an early stage compared with other types of ovarian cancer. Between 57 percent and 81 percent of OCCC cases are discovered when they are stage 1 or stage 2.
Prognosis And Predictive Factors
Patients with clear cell renal cell carcinoma tend to have a worse prognosis than patients with other histologic subtypes of RCC, with 5-year disease-specific survival rates of 50-69%, compared with 67-87% for papillary RCC and 78-87% for chRCC. However, analysis of 1000 patients showed very similar 5-year disease-specific survival rates for CCRCC and papillary RCC once metastatic disease was present.
Multivariate analyses indicate that histologic RCC subtype has no significant independent value for predicting cancer-specific survival because prognosis is primarily dependent upon TNM stage and Fuhrman nuclear grade. Multivariate analysis specifically of CCRCC cases shows that in addition to the 3 separate components of tumor staging , other significant independent predictors of poor prognosis are nuclear grade, tumor size, and the presence of histologic necrosis or sarcomatoid differentiation.
Rhabdoid differentiation is also observed in CCRCC and seems to impart a poor outcome similar to sarcomatoid change however, this factor has not yet been tested in predictive models. Interestingly, histological necrosis is seen more commonly in papillary RCC but is not a significant predictor of poor prognosis for papillary RCC, even in univariate analyses.
References
Delahunt B, Eble JN. History of the development of the classification of renal cell neoplasia. Clin Lab Med. 2005 Jun. 25:231-46, v. .
Pascual D, Borque A. Epidemiology of kidney cancer. Adv Urol. 2008. 782381. .
Don’t Miss: How Do Carcinomas Spread
Health Literacy To Empower Patients
With the right information, patients can make the best decisions about their care. By partnering with patients, healthcare providers, and hospitals, we hope to provide all patients with the tools and knowledge to understand their pathology report.
For more information about this site, contact us at .
Disclaimer: MyPathologyReport.ca is a registered not-for-profit charity . The articles on MyPathologyReport are intended for general informational purposes only and they do not address individual circumstances. The articles on this site are not a substitute for professional medical advice, diagnosis, or treatment and should not be relied on to make decisions about your health. Never ignore professional medical advice in seeking treatment because of something you have read on the MyPathologyReport site. MyPathologyReport is independently owned and operated and is not affiliated with any hospital or patient portal.
Copyright © 2021. All rights reserved. Privacy Policy
Our work is generously supported by:
Serum Cancer Antigen 125
The conventional tumor marker CA125 has long been used in the diagnosis of HGSC. It is elevated in 75.6% of serous carcinoma cases but in only 57.6% of OCCC cases . Thus, CA125 is a poor marker for OCCC, with only a mildly elevated baseline value and a frequent incidence of false-negative results . However, CA-125 levels can be used for predicting advanced stage disease, suboptimal debulking and platinum-resistance with cut-off values of 46.5 U/mL, 11.45 U/mL, and 66.4 U/mL . Increased CA125 levels after the end of chemotherapy is significantly associated with shorter PFS and OS, so it also can be used as a valid indicator of the prognosis and efficacy of chemotherapy in patients with OCCC . Because there is currently no appropriate biomarker for OCCC, novel diagnostic markers are urgently required to improve early diagnosis and therapeutic stratification of the disease to provide more favorable prognoses and survivability.
Recommended Reading: How Long Until Melanoma Spreads