What Are The Clinical Features Of Intraepidermal Scc
Intraepidermal SCC presents as one or more irregular scalyplaques of up to several centimetres in diameter. They are often an orange-red colour but may also be brown.
Although intraepidermal SCC may arise on any area of skin, it is most often diagnosed on sun-exposed sites of the ears, face, hands and lower legs. When there are many plaques, distribution is not symmetrical .
Intraepidermal squamous cell carcinoma
Intraepidermal SCC may start to grow under a nail when it results in a red streak that later may destroy the nail plate.
Intraepidermal squamous cell carcinoma of the nail
What Is Intraepidermalsquamous Cell Carcinoma
Intraepidermal squamous cell carcinoma is a common superficial form of keratinocytecancer. It is also known as Bowen disease, intraepidermal carcinoma and carcinoma in situ .
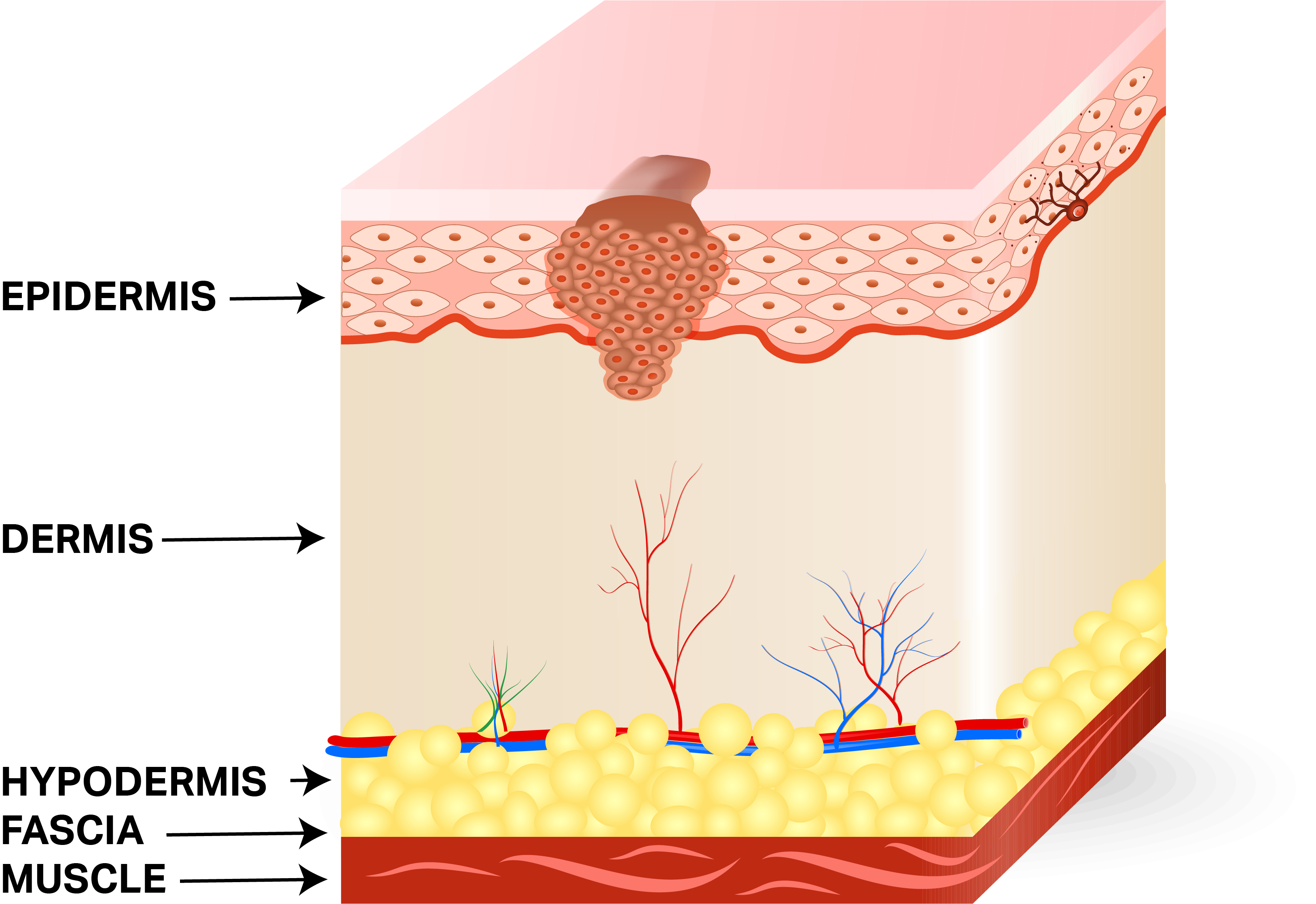
Intraepidermal SCC is derived from squamous cells, the flat epidermal cells that make keratin, the horny protein that makes up skin, hair and nails. Intraepidermal and in situ mean the malignant cells are confined to the tissue of origin, in this case, the epidermis.
Causes And Risk Factors
The causes of Bowens Disease are different among patients, but I listed some of the factors that are associated with the skin condition. Please note that if you have or experienced the things that I have listed doesnt mean that you will have the condition. The list that I will provide is the risk factors that are linked to Bowens Disease.
- Positive Family History Family History has a strong relationship with diseases that we had, we are having, and we will have in the future. Although not definite, somehow researchers are able to find certain connections between our genes and our overall health.
- Excessive Sun Exposure Sun exposure is not bad, in fact, it is good for everyone to go out in the sun once in a while. But if there is an excessive exposure to sunlight, there can be consequences, skin diseases are often related to sunlight exposure.
- HPV Infection According to a research study about Bowens Disease, HPV or Human Papilloma Virus infection can predispose a person to Bowens Disease.
- Long-term Skin Condition/Injury Chronic skin diseases can cause destruction and harm to our healthy cells, this may cause our cells to mutate and produce cancer cells that can lead to various skin cancers.
- This one is self explanatory, a person with decreased immune system will increase the chance to catch an infection then it will proceed to a long-term health condition, in the worst case scenario, it can develop into a terminal illness.
Read Also: Can You Die From Basal Cell Skin Cancer
What Does It Mean If The Following Terms Are Used To Describe The Adenocarcinoma: Papillary Micropapillary Acinar Mucinous Or Solid
These terms describe different types of lung adenocarcinoma, which are based on how the cells look and are arranged under the microscope . Some tumors look basically the same throughout the tumor, and some can look different in different areas of the tumor. Some growth patterns have a better prognosis than others. Since some tumors can have a mixture of patterns, the pathologist canât always tell all the types contained in a tumor just based on a biopsy that samples only a small part of the tumor. To know what types a tumor contains, the entire tumor must be removed.
What Are The Risk Factors For Invasive Squamous Cell Carcinoma Of Anus
Invasive Squamous Cell Carcinoma of Anus develops from squamous cell carcinoma in situ. The risk factors that contribute to squamous cell carcinoma in situ formation include:
- Human papilloma virus infection the subtypes responsible include 16, 18, 31, 33, and 45,
- High-risk sexual behavior, such as multiple partners and unprotected sex
- Weakened immune system due to many reasons, such as organ transplant, old age, HIV/AIDS infection, or due to administration of immune suppressing drugs
- Smoking of tobacco
- Poor personal hygiene
- Ulcerative lichen planus
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases ones chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
Also Check: Can You Die From Basal Cell Skin Cancer
What Does Squamous Cell Carcinoma Look Like
Squamous cell carcinoma , also known as squamous cell cancer, is the second most common type of skin cancer following basal cell carcinoma. About 1 million cases are diagnosed each year in the United States. It begins in the squamous skin cells located in the top layer of skin called the epidermis. The DNA in squamous cells can become damaged from ultraviolet rays from the sun or tanning beds. When this occurs, they begin to grow at an out-of-control rate, leading to skin cancer.
Fortunately, when caught early, most cases of squamous cell carcinoma are curable. Knowing the early warning signs is critical to receiving an early diagnosis and treatment.
Unprotected exposure to UV rays is a major risk factor for squamous cell carcinoma. The more time you spend in the sun , the more likely you are to develop SCC. About 90% of non-melanoma skin cancers are related to exposure to UV rays. Other risk factors of SCC include light skin, age , male sex, immunosuppression, human papillomavirus, chronic scarring conditions, family history, and toxic exposures.
What Are Basal And Squamous Cell Skin Cancers
Basal and squamous cell skin cancers are the most common types of skin cancer. They start in the top layer of skin , and are often related to sun exposure.
Cancer starts when cells in the body begin to grow out of control. Cells in nearly any part of the body can become cancer cells. To learn more about cancer and how it starts and spreads, see What Is Cancer?
Read Also: Stage 2 Cancer Symptoms
What Are The Causes Of Invasive Squamous Cell Carcinoma Of Anus
Untreated squamous cell carcinoma in situ can result in invasive squamous cell carcinoma.
- The exact cause of development of squamous cell carcinoma in situ of anus is not completely known in a majority of cases
- In case HPV infection is associated with SCC in situ of anus, it is caused by alteration in the DNA by the human papilloma virus that results in uncontrolled cell proliferation
- Other factors that may contribute to the condition include compromised immune system, sexual promiscuity, smoking, and even poor hygiene
What If My Report Mentions Margins
The margin is the edge or the boundary of the specimen that was removed by the surgeon. It is where the surgeon has sectioned across the lung to remove the tumor.
The margin may be free of the tumor that is, a rim of uninvolved tissues may surround the tumor, indicating that the tumor has been removed completely. This is sometimes referred to as a negative margin.
Alternatively, the tumor could extend to the edge of the specimen , implying that the tumor has not been completely removed. This is sometimes referred to as a positive margin.
The status of the margin is an important indicator of the potential for the tumor to recur and of the need for further treatment. Talk with your doctor about the best approach for you if cancer is found at the margins.
Also Check: How Fast Does Cancer Kill
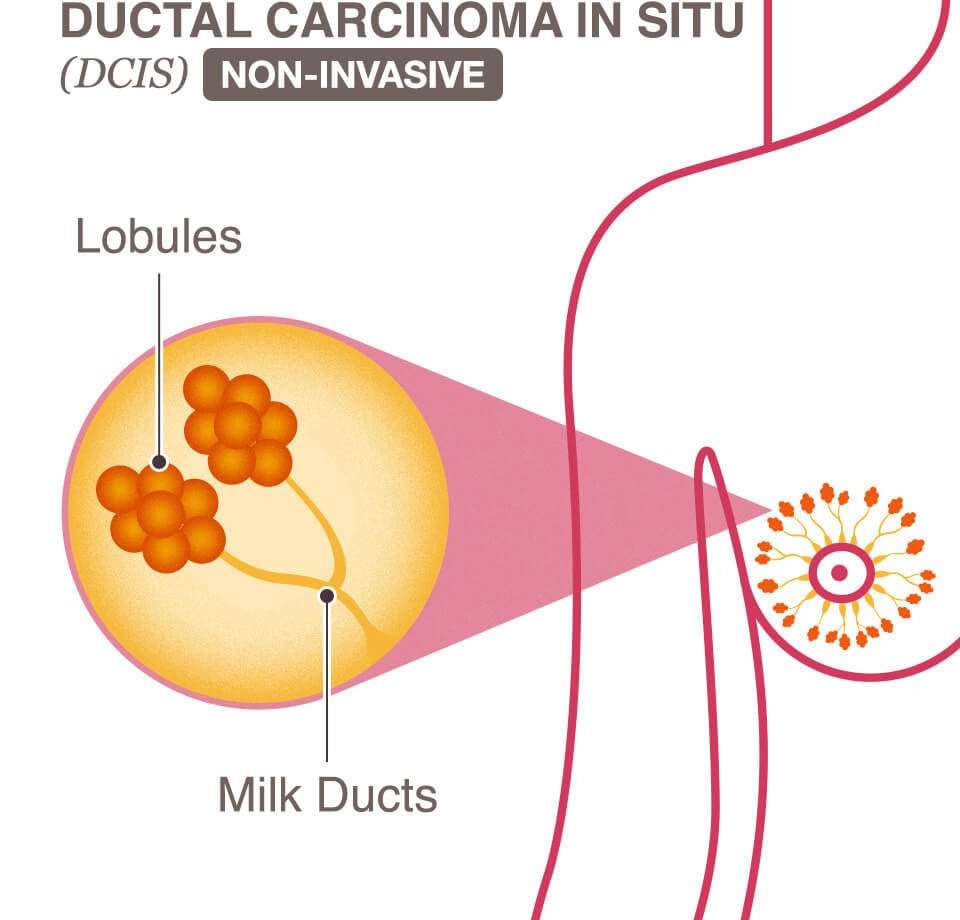
Carcinoma In Situ Vs Precancerous Cells Vs Dysplasia
There are many terms describing the spectrum of normal cells and invasive cancer cells. One of these is dysplasia. Dysplasia can run the spectrum from mild dysplasia in which the cells are barely abnormal appearing, to carcinoma in situ, which some pathologists describe as severe dysplasia involving the full thickness of the epithelium. The term precancerous cells may also be used to describe cells on this continuum between normal and cancer cells.
These terms are also used in different ways depending on the sample analyzed. For example, cells visualized on a pap smear may show dysplasia , but since the cells are “loose,” nothing can be said about whether carcinoma in situ is present or not. With cervical dysplasia, a biopsy is required before the diagnosis of CIS is made. A biopsy sample provides a view of the cells as they occur in relation to the basement membrane and other cells, and is needed to understand if abnormal cells seen on a pap smear are concerning.
What Is The Significance Of The Reported Size Of The Tumor
If the entire tumor is removed, the pathologist will measure its size by looking at it , or, if it is very small, measure it under the microscope. Often, what is reported is how big across it is in the area where the tumor is the largest. This is called the greatest dimension of the tumor, as in âthe tumor measured 2 centimeters in greatest dimension.â In general, smaller tumors have a better prognosis .
A biopsy of a tumor only samples a part of the tumor, so measurements of its overall size cannot be reported.
Read Also: What Is The Life Expectancy Of Someone With Metastatic Melanoma
In Situ Hybridization For Hpv
In Situ hybridization was carried out on formalin fixed, paraffin embedded, 4-µm tissue sections on a Ventana Benchmark LT-automated immunostainer according to the manufacturers instructions. This uses the ISH I View Blue Plus Detection Kit that is a biotin-streptavidin-based detection system. The Ventana HPV III Family 16, probe B, a cocktail recognizing the high risk HPV types 16, 18, 31, 33, 35, 45, 51, 52, 56, 58, 59, 68, and 70 was used along with endogenous biotin blocking and counter staining with Ventana Red Counterstain II . A known HPV-positive head and neck SCC case was used as a positive control and normal tonsil sections as the negative control with each run. Staining was read by a single study researcher . Positive staining was identified as blue nuclear dots and ranged widely, from strongly and diffusely positive across the entire tumor to extremely focal, with only rare positive cells. The individual nuclear pattern ranged from granular staining across the whole nucleus to single, punctate, single focus staining. These 2 patterns would seem to correspond to episomal versus integrated virus, but as earlier studies have shown, this does not necessarily correlate for this particular assay. Any definitive nuclear staining in the tumor cells was considered positive. Cases were classified in a binary manner as either positive or negative.
What Is Squamous Cell Carcinoma Of Tongue
- Squamous Cell Carcinoma of Tongue is a common malignant tumor that typically affects elderly men and women. It is more aggressive than conventional squamous cell carcinoma affecting other body regions
- The cause of the condition is unknown, but genetic mutations may be involved. Factors that may influence its development include smoking and chewing of tobacco, radiation treatment for other reasons, and exposure to coal tar and arsenic
- The squamous cell carcinoma may appear as slow-growing skin lesions. The lesions may ulcerate and cause scarring of the tongue. It may be difficult to eat, swallow food, or even to speak
- The treatment of choice is a surgical excision with clear margins followed by radiation therapy or chemotherapy, as decided by the healthcare provider. In majority of the cases, the prognosis is good with appropriate treatment
- Nevertheless, the prognosis of Squamous Cell Carcinoma of Tongue depends upon many factors including the stage of the tumor and health status of the affected individual. There is a possibility of local or regional metastasis, which can involve the lymph nodes. This may dictate the course of the condition
Don’t Miss: What Does Stage 3b Melanoma Mean
What Is The Significance Of The Stage Of The Cancer
The stage of the cancer is a measurement of the extent of cancer growth, including its spread to other parts of the body. To know the stage of a lung cancer, you need information on the size of the tumor in the lung and if the cancer is growing into any nearby organs or structures. You also need to know if the cancer has spread to any nearby lymph nodes or to distant sites.
Each of these pieces of information is represented by a letter:
- T stands for the main tumor.
- N stands for spread to nearby lymph nodes.
- M is for metastasis to distant parts of the body.
Once the T, N, and M categories are determined, they are combined to create an overall stage, which is given a number of I to IV , with a higher number meaning larger extent or spread of disease.
Staging information cannot usually be given for a biopsy specimen, because the pathologist needs to have the entire tumor and nearby lymph nodes to evaluate.
When this information is obtained by removing the tumor and nearby lymph nodes at surgery, a lower-case letter âpâ is put before the T and N. So, in your pathology report, pT would be followed by numbers and letters based on the size of the tumor and some other information about it. The larger the number, the more advanced the cancer. pN followed by numbers and letters is based on the extent of spread to nearby lymph nodes that may have been removed at the same time as the lung tumor.
Discuss how the stage of your tumor will affect your treatment with your doctor.
Looking After Your Skin After Treatment
After treatment, you may need follow-up appointments with your dermatologist or GP to see if you need any further treatment.
If you had surgery, you may need to have any stitches removed at your GP surgery a few weeks later.
After treatment:
- see a GP if an existing patch starts to bleed, change in appearance or develops a lump do not wait for your follow-up appointment
- see a GP if you notice any worrying new patches on your skin
- make sure you protect your skin from the sun wear protective clothing and use a sunscreen with a high sun protection factor of at least 30
Page last reviewed: 21 May 2019 Next review due: 21 May 2022
| Other names | Cutaneous squamous cell carcinoma , epidermoid carcinoma, squamous cell epithelioma |
|---|---|
| SCC of the skin tends to arise from pre-malignant lesions, actinic keratoses surface is usually scaly and often ulcerates . | |
| 51,900 |
Squamous-cell skin cancer, also known as cutaneous squamous-cell carcinoma , is one of the main types of skin cancer along with basal cell cancer, and melanoma. It usually presents as a hard lump with a scaly top but can also form an ulcer. Onset is often over months. Squamous-cell skin cancer is more likely to spread to distant areas than basal cell cancer. When confined to the outermost layer of the skin, a precancerous or in situ form of cSCC is known as Bowenâs disease.
Recommended Reading: Lobular Breast Cancer Survival Rates
What Is Squamous Dysplasia
Dysplasia is an early form of pre-cancer. It is often separated into different categories based on how abnormal the cells and tissue appear under the microscope:
- When it is the least abnormal, it is called mild dysplasia.
- When it is most abnormal, it is called severe dysplasia.
- Moderate dysplasia is in between the other two.
The more severe the dysplasia is, the more similar it is to squamous cell carcinoma in situ, which is a pre-cancer. If squamous dysplasia is seen on a biopsy, it might mean that there is something more serious, like in-situ or invasive carcinoma, somewhere else in the lung that wasnât sampled on this biopsy.
What Is Squamous Cell Cancer
Squamous cell carcinoma of the skin is a common skin cancer that typically develops in chronic sun-exposed areas of your body. This type of skin cancer is usually not nearly as aggressive as melanoma and is uncontrolled growth of cells in the epidermis of your skin.
It can become disfiguring and sometimes deadly if allowed to grow. Squamous cell carcinomas are at least twice as frequent in men as in women. They rarely appear before age 50 and are most often seen in individuals in their 70s.
An estimated 700,000 cases of SCC are diagnosed each year in the United States, resulting in approximately 2,500 deaths.
Also Check: Can You Die From Basal Cell Skin Cancer
How Can You Prevent Squamous Cell Carcinoma
Practicing sun safety is the best way to prevent SCC and other skin cancers. Here are some tips:
- Avoid being in the sun from 10 am to 4 pm.
- Avoid tanning beds.
- Use a broad spectrum sunscreen with an SPF of 15 or higher each day. If you will be outside for longer periods of time, use a broad spectrum sunscreen that is water-resistant and has an SPF of 30 or higher. Put the sunscreen on 30 minutes before going outside. Put sunscreen on again every two hours, or more frequently if you have been swimming or sweating a lot.
- Use protective clothing that has built-in sun protection, which is measured in UPF. Also, use broad-brimmed hats and sunglasses.
- Do your own skin self-exam about once per month, and see a dermatologist about one time per year for a professional skin exam.
- Have any skin changes examined as soon as possible by a healthcare provider.
How Common Is Squamous Cell Carcinoma
Over 1 million people are diagnosed with SCC in the US each year. The incidence of SCC has risen about 200 percent over the past 30 years. There are more than 15,000 deaths each year in the US from SCC. Excluding head and neck SCC and CSCC in situ, about 200,000-400,000 new cases of SCC are diagnosed in the US every year, resulting in about 3,000 deaths.
Men are about two times more likely than women to develop SCCs. People over the age of 50 are most likely to get SCCs, but the incidence has been rising in younger people.
Don’t Miss: Invasive Mammary Carcinoma Survival Rate