Treatments For Stage Ii Melanoma
As with stage I, stage II melanoma is typically treated with wide excision surgery, which cuts out the melanoma along with a margin of healthy surrounding skin. In the case of stage II melanoma, many doctors will recommend looking for cancer in nearby lymph nodes by performing a sentinel lymph node biopsy, which may necessitate further treatment if cancer cells are found.
What Is The Follow
Most patients with melanoma in situ will be advised to have follow-up examinations with their specialist or general practitioner. The main focus will be a total body skin examination, because patients with a melanoma in situ have eight times the risk of developing another in-situ or invasive primary melanoma compared to matched individuals without melanoma in situ.
What Is The Cause Of Superficial Spreading Melanoma
Superficial spreading melanoma is due to the development of malignant pigment cells along the basal layer of the epidermis. The majority arise in previously normal-appearing skin. About 25% develop within an existing melanocytic naevus, which can be a normal common naevus, an atypical or dysplastic naevus, or a congenital naevus.
What triggers the melanocytes to become malignant is not fully known. Specific genemutations such as BRAFV600E have been detected in many superficial spreading melanomas and these mutations may change as the disease advances.
Damage by ultraviolet radiation results in a degree of immune tolerance, allowing abnormal cells to grow unchecked. This can occur from exposure to natural sunlight, particularly if sunburn has occurred, and artificial sources of ultraviolet radiation from sun beds / solaria.
Read Also: Merkel Cell Carcinoma Immunotherapy
What Is Melanoma In Situ
Melanoma in situ is the very earliest stage of a skin cancer called melanoma. In situ means that the cancer cells have not had the opportunity to spread to anywhere else in the body, they remain in the top layer of the skin and are all contained in the area in which they began to develop. They have not started to spread or grow into deeper layers of the skin and have not become invasive. Some doctors call melanoma in situ a pre cancer.
Melanoma in situ can be cured with surgery. However if not treated appropriately, melanoma in situ can develop into an invasive cancer called melanoma. It is therefore important to have it removed with a border of healthy skin , there are also preventative measures you can take which will lower your risk of this condition occurring in the future.
Can Changing My Diet Help Prevent Melanoma
The American Cancer Society advocates eating a plant-based diet over an animal-based diet as part of a healthy plan to avoid all cancers. Growing evidence suggests that plants pack a powerful punch in any fight against cancer because they’re nutritious, cholesterol-free and fiber-rich.
Theres no doubt that a healthy diet can protect your immune system. Having a strong immune system is important to help your body fight disease. Some research has shown that a Mediterranean diet is a healthy choice that may help prevent the development of cancer. Talk to your healthcare provider about the role food plays in lowering your cancer risks.
Some skin and immune-system healthy foods to consider include:
- Daily tea drinking: The polyphenols in tea help strengthen your immune system. Green tea contains more polyphenols than black tea.
- High vegetable consumption: Eating carrots, cruciferous and leafy vegetables is linked to the prevention of cutaneous melanoma.
- Weekly fish intake: Study participants who ate fish weekly seemed to avoid developing the disease when compared to those who did not eat fish weekly.
Read Also: Invasive Lobular Breast Cancer Survival Rate
What Is Lentigo Maligna
Lentigo maligna is a type of melanoma in situ. It is a slow growing lesion that appears in areas of skin that get a lot of sun exposure, such as the face or upper body. Because it grows slowly it can take years to develop. As with melanoma in situ, the cancer cells have not had the opportunity to spread to anywhere else in the body, they remain in the top layer of the skin and are all contained in the area in which they began to develop. They have not started to spread or grow into deeper layers of the skin and have not become invasive. Like melanoma in situ some doctors call lentigo maligna a pre cancer.
Lentigo maligna can be cured with surgery. However, if not treated appropriately, lentigo maligna may later develop into an invasive cancer called lentigo maligna melanoma.
It is therefore important to have it removed with a rim of normal skin , there are also preventative measures you can take which will lower your risk of this condition occurring in the future.
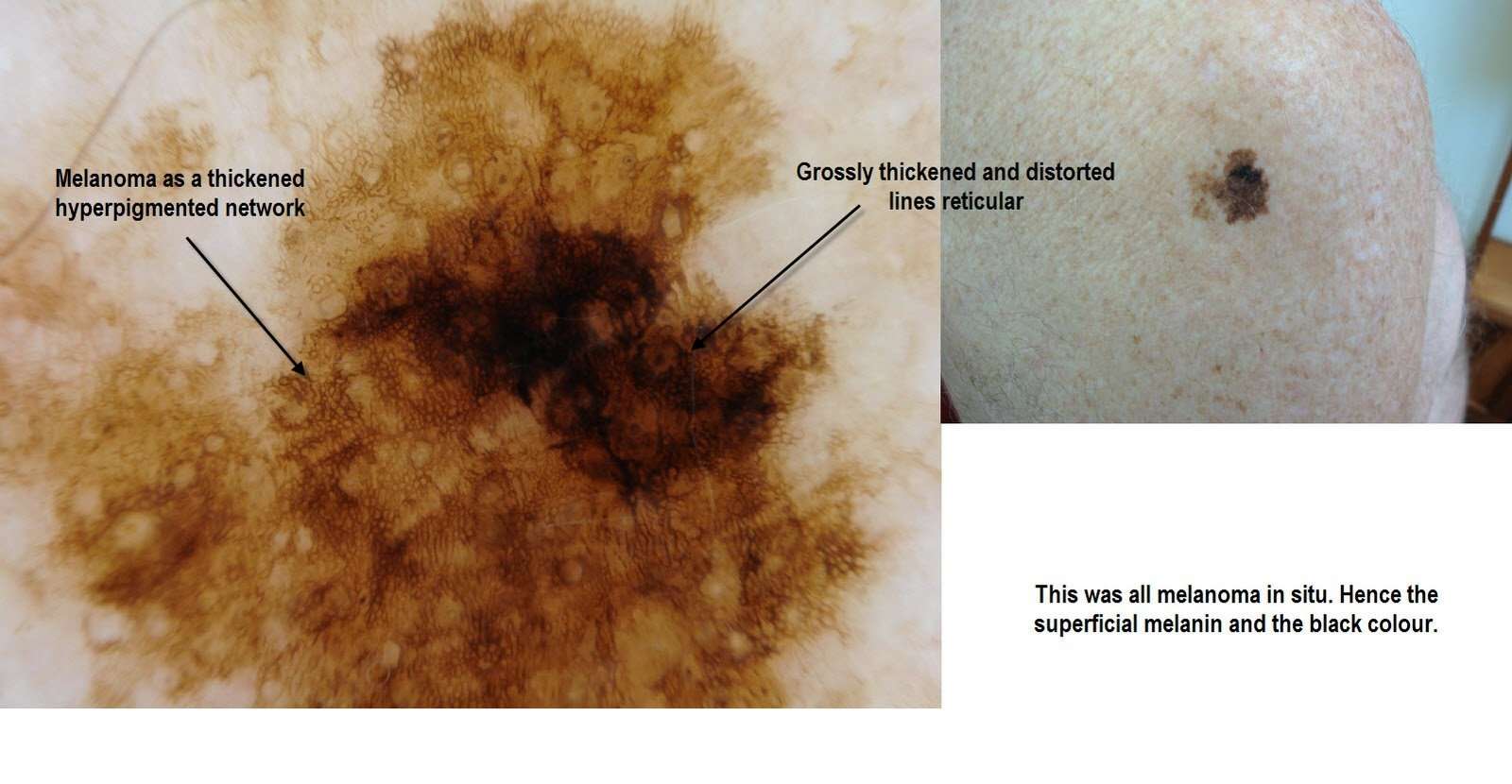
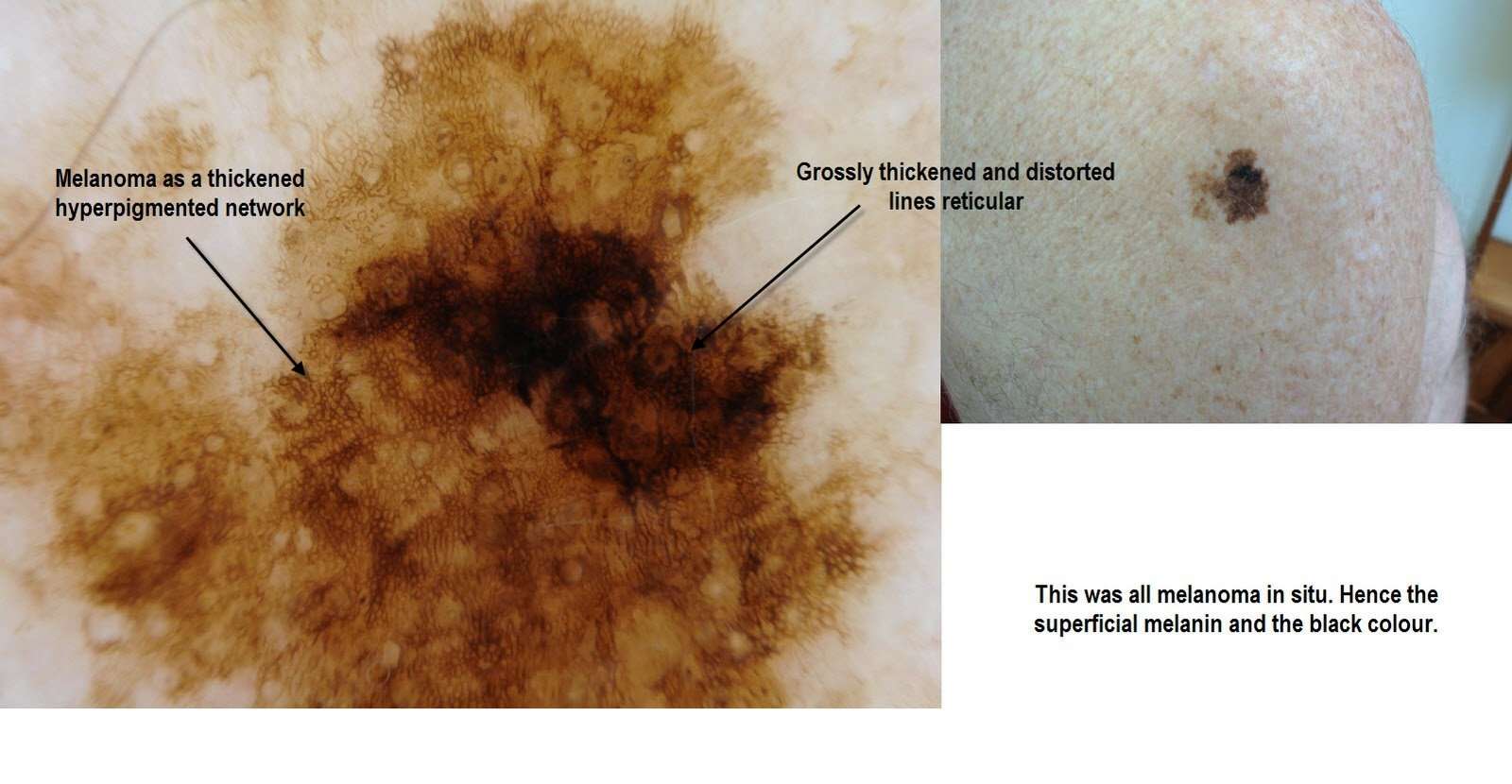
What Are The Clinical Features Of Melanoma In Situ
Typically, melanoma in situ is an irregular pigmentedpatch of skin. It often has the ABCDE criteria:
ABCDE
The body site and other clinical features of melanoma in situ depend on the subtype of melanoma . In general terms, melanoma in situ is macular . However, in about 8% of cases, melanoma in situ is thickened and can be scaly due to reactive thickening of the epidermis .
Don’t Miss: Invasive Breast Cancer Prognosis
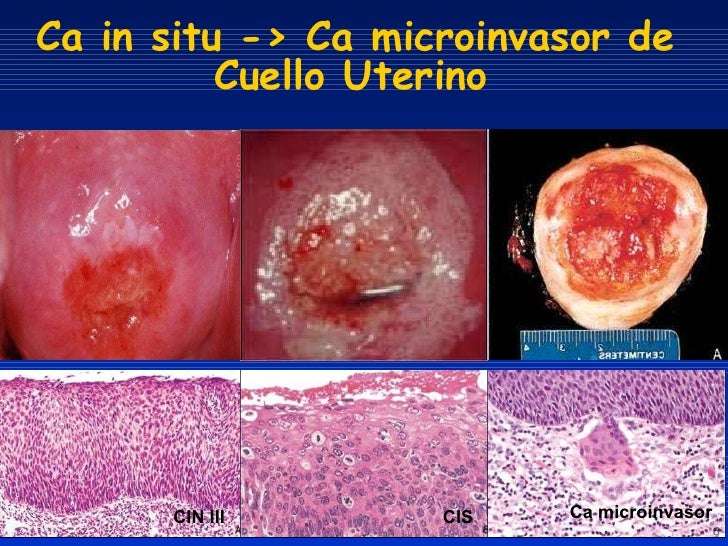
Carcinoma In Situ Vs Cancer
A million-dollar question lately, especially with controversy over the treatment of ductal carcinoma in situ or in situ breast cancer, is whether or not carcinoma in situ is really cancer. The answer is that it depends on who you talk to. Some physicians classify carcinoma in situ as non-invasive cancer and others may prefer calling it pre-cancer. The distinction would lie in knowing whether or not the CIS would progress to invasive cancer, and that, by definition, is not known. Nor are we apt to get answers soon, as it wouldn’t be ethical to simply watch large numbers of carcinoma in situ’s to see if they became invasive cancer and spread.
How Can A Returning Melanoma Appear In A New Place
Melanoma spreads when cancer cells break off from the original melanoma. When the cells break off, they may stay where they are or travel to another part of the body.
Because the cancer cells are from the original melanoma, the cancer is said to have returned. This is true even if the returning melanoma appears far from the original melanoma.
Also Check: Stage 5 Cancer Symptoms
Where Does Melanoma Return
It may come back in the same place or on the same area of your body. This is most common.
Melanoma can also return far from where you had the first one. For example, if you had a melanoma on your back, it could return on your arm.
It can also show up inside your body. If melanoma appears inside the body, its most likely to show up in the lymph nodes, lungs, liver, brain, bone, or gastrointestinal tract.
Recurrence In Other Parts Of The Body
Melanoma can also come back in distant parts of the body. Almost any organ can be affected. Most often, the melanoma will come back in the lungs, bones, liver, or brain. Treatment for these recurrences is generally the same as for stage IV melanoma . Melanomas that recur on an arm or leg may be treated with isolated limb perfusion/infusion chemotherapy.
Melanoma that comes back in the brain can be hard to treat. Single tumors can sometimes be removed by surgery. Radiation therapy to the brain may help as well. Systemic treatments might also be tried.
As with other stages of melanoma, people with recurrent melanoma may want to think about taking part in a clinical trial.
The treatment information given here is not official policy of the American Cancer Society and is not intended as medical advice to replace the expertise and judgment of your cancer care team. It is intended to help you and your family make informed decisions, together with your doctor. Your doctor may have reasons for suggesting a treatment plan different from these general treatment options. Dont hesitate to ask him or her questions about your treatment options.
Read Also: What Does Well Differentiated Mean
What Are Lymph Nodes
Lymph nodes are small structures that filter substances and help fight infection. They are part of a network that runs throughout the body. Cancer that reaches the lymph nodes is concerning because cancer cells can easily spread to other parts of the body through this interconnected system.
Whether or not a melanoma spreads to one or more lymph nodes, it also may affect nearby skin. Such melanoma tumors are called satellite tumors. They’re defined as being within 2 centimeters of the original tumor and can be seen without a microscope.
Melanoma tumors also may spread to lymphatic channels, thin tubes that resemble blood capillaries, through which lymph fluid flows.
Treating Stage 0 Melanoma
Stage 0 melanoma has not grown deeper than the top layer of the skin . It is usually treated by surgery to remove the melanoma and a small margin of normal skin around it. The removed sample is then sent to a lab to be looked at with a microscope. If cancer cells are seen at the edges of the sample, a second, wider excision of the area may be done.
Some doctors may consider the use of imiquimod cream or radiation therapy instead of surgery, although not all doctors agree with this.
For melanomas in sensitive areas on the face, some doctors may use Mohs surgery or even imiquimod cream if surgery might be disfiguring, although not all doctors agree with these uses.
Read Also: Small Blue Cell Tumor Prognosis
Supplement Mohs Surgery And Staged Serial Excision
A large prospective study assessed complete clearance of 1120 melanomas in situ excised by Mohs micrographic surgery with frozen-section examination of the margin. Six millimetre margins were adequate for complete clearance in 86% of all tumours 9 mm margins were adequate for complete clearance in 98.9% of all tumours. A 1.2 cm margin yielded 99.4% clearance, 1.5 cm margin yielded 99.6% clearance, and 3 cm margin yielded 100% clearance. The authors state that the frequently recommended 5 mm margin for melanoma is inadequate. Standard surgical excision of melanoma in situ should include 9 mm of normal-appearing skin, similar to that recommended for early invasive melanoma. This study includes a mixture of cases of melanoma in situ, both LM and non-lentigo maligna type, and it is possible that LM requires a wider margin than other melanomas in situ.
A retrospective review of 192 cases of melanoma in situ found that LM required wider margins for complete excision than did non-lentigo maligna melanoma in situ.
In a study of 51 cases of facial LM and thin LMM, with LMM present in nine lesions , peripheral margin control was performed with repeated margin excision until histological clearance of the lesion. Margins required for clearance of LM and LMM averaged 1.0 and 1.3 cm, respectively. No recurrences were identified with long-term follow-up. Immediate reconstruction was performed in all cases.
You May Like: Is Skin Cancer Usually Raised
About Melanoma In Situ
Melanoma in situ is not a life threatening lesion. The challenge with melanoma treatment is that within some lesions diagnosed as melanoma-in-situ there may be foci of invasive melanoma. This is the essence of why complete surgical excision of melanoma-in-situ is necessary. Ruling out an invasive component within a melanoma-in-situ is the cornerstone of management of these lesions.
The second important reason for treating melanoma-in-situ is the risk of degeneration of an in-situ melanoma into an invasive melanoma. The risk has been estimated from 5-10% over a patients lifetime. Some judge the risk to be 2-3% per decade of life of degeneration into an invasive melanoma.
What is fascinating about melanoma-in-situ developing invasive components, is their relatively low metastatic risk. Unlike de novo invasive melanomas, the invasive melanomas originating in melanoma-in-situ appear to be less aggressive.
Some older studies from Europe have tracked the natural history of a population of melanoma-in-situ. These have shown evidence of transformation into invasive melanomas and evidence of recurrence, but no described incidents of mortality due to invasive melanoma degeneration.
Recommended Reading: Invasive Ductal Carcinoma Grade 3 Survival Rate
What They Look Like
Melanomas in situ tend to be flat and asymmetric with irregular borders. They can be black, brown, tan, gray or even pink if the person has very fair skin. Areas that receive the greatest sun exposure, such as the scalp, face and neck, are more likely to develop melanoma in situ than the arms or legs. However, non-sun exposed areas, such as the buttocks, are also at risk. We dont always understand the causes of these melanomas, though heredity can play a role. To detect melanoma in situ as early as possible, it helps to monitor your own skin. Head-to-toe self-examinations are a good place to start, including the areas where the sun doesnt shine. When evaluating your skin, focus on the ABCDEs of melanoma detection. A stands for asymmetryB for irregular bordersC for more than one colorD for diameter greater than 6mm , or the size of a pencil eraser and E for evolving, meaning any lesion that is new or changing. View helpful photos showing the ABCDEs of melanoma.
Also Check: Are There Stages Of Basal Cell Carcinoma
What Will You Find On A Pathology Report
The report is broken down into a few sections including:
- Some information about the patient.
- Diagnosis if it is known.
- Procedure.
- Description of what the specimen looks like to the naked eye
- Description of what was seen under the microscope
- Where the tissue was taken from.
- Diagnosis of the biopsy.
The pathologist will describe the type of melanoma and some characteristics or features of it that are important for prognosis and treatment. To help you read your report, lets go through what you may find in your report.
Type of Melanoma
Also called the histologic type or cellular type of melanoma. There are four major subtypes, with a few rare subtypes:
- Superficial Spreading Melanoma: most common of the melanomas.
- Nodular Melanoma: are always vertical growth phase present melanomas. Most commonly found on the chest, back, head or neck.
- Acral Lentiginous: most common type in dark skinned and Asian populations. More frequently occur on soles of feet, palms of hands or under nails.
- Lentigo Maligna Melanoma: tends to occur on sun-exposed areas in older people. Often found on the face or neck.
- Rare subtypes: mucosal melanoma, desmoplastic melanoma, nevoid melanoma
Breslow Depth Classification:
- Melanoma in situ or thin invasive tumors: less than 1.0mm in depth.
- Intermediate risk melanoma: 1mm 4mm in thickness.
- High risk melanoma: greater than 4.0mm in depth.
Types of Biopsies :
Also Check: Stage 2 Invasive Ductal Carcinoma Survival Rate
Treating Stage I Melanoma
Stage I melanoma is typically treated by wide excision . The width of the margin depends on the thickness and location of the melanoma. Most often, no other treatment is needed.
Some doctors may recommend a sentinel lymph node biopsy to look for cancer in nearby lymph nodes, especially if the melanoma is stage IB or has other characteristics that make it more likely to have spread. You and your doctor should discuss this option.
If the SLNB does not find cancer cells in the lymph nodes, then no further treatment is needed, although close follow-up is still important.
If cancer cells are found on the SLNB, a lymph node dissection might be recommended. Another option might be to watch the lymph nodes closely by getting an ultrasound of the nodes every few months.
If the SLNB found cancer, adjuvant treatment with an immune checkpoint inhibitor or targeted therapy drugs might be recommended to try to lower the chance the melanoma will come back. Other drugs or perhaps vaccines might also be options as part of a clinical trial.
Understanding Melanoma In Situ And Lentigo Maligna
Introduction
This leaflet has been written to help you understand more about melanoma in situ and lentigo maligna. It will tell you what they are, what causes them, how they are treated and where you can find out more information.
You may need to ask your doctor or nurse for information that is more personal to you please do not hesitate to ask any questions or voice any concerns that you, or your family may have, to your medical team.
Don’t Miss: How Long Does It Take For Melanoma To Metastasize
Diagnosis And Staging What It Means For You
How is melanoma diagnosed?
To diagnose melanoma, a dermatologist biopsies the suspicious tissue and sends it to a lab, where a dermatopathologist determines whether cancer cells are present.
After the disease is diagnosed and the type of melanoma is identified, the next step is for your medical team to identify the stage of the disease. This may require additional tests including imaging such as PET scans, CT scans, MRIs and blood tests.
The stage of melanoma is determined by several factors, including how much the cancer has grown, whether the disease has spread and other considerations. Melanoma staging is complex, but crucial. Knowing the stage helps doctors decide how to best treat your disease and predict your chances of recovery.
Lentigo Maligna And Melanoma In Situ
What are lentigo maligna and melanoma in situ?
Lentigo maligna and melanoma in situ are the very earliest stage of a skin cancer called melanoma.
The word melanoma comes from the Greek word melas, meaning black. Melanin is the dark pigment that gives the skin its natural colour.
Melanin is made in the skin by pigment cells called melanocytes. After our skin is exposed to sunlight, the melanocytes make more melanin, and so the skin becomes darker.
Melanocytes sometimes grow together in harmless groups or clusters, which are known as moles. Most people have between 10 and 50 moles and often they are darker than the surrounding skin.
Melanomas can arise in or near to a mole, but can also appear on skin that looks quite normal. They develop when the skin pigment cells become cancerous and multiply in an uncontrolled way. They can then invade the skin around them and may also spread to other areas such as the lymph nodes, liver and lungs.
In situ means that the cancer cells have not had the opportunity to spread to anywhere else in the body. There are cancer cells in the top layer of the skin but they are all contained in the area in which they began to develop. They have not started to spread or grow into deeper layers of the skin and have not become invasive. This is why some doctors call in situ cancers pre cancer. The prognosis is excellent.
What causes lentigo maligna and melanoma in situ?
Some people are more likely to get a melanoma than others:
Also Check: Stage Iiia Melanoma Prognosis