Skin Cancer In Victoria
Over the past 30 years, UV protection programs like the SunSmart program have educated Victorians about the importance of sun protection at every age.
Although the incidence of melanoma and non-melanoma skin cancer has increased since 2000, recent data from the Victorian Cancer Registry shows rates are stabilising or declining in all age groups under 60 years. Those who have grown up with the SunSmart program for a greater part of their life are benefiting the most with lower rates of melanoma.
Read more about skin cancer.
Risk Of Getting Melanoma
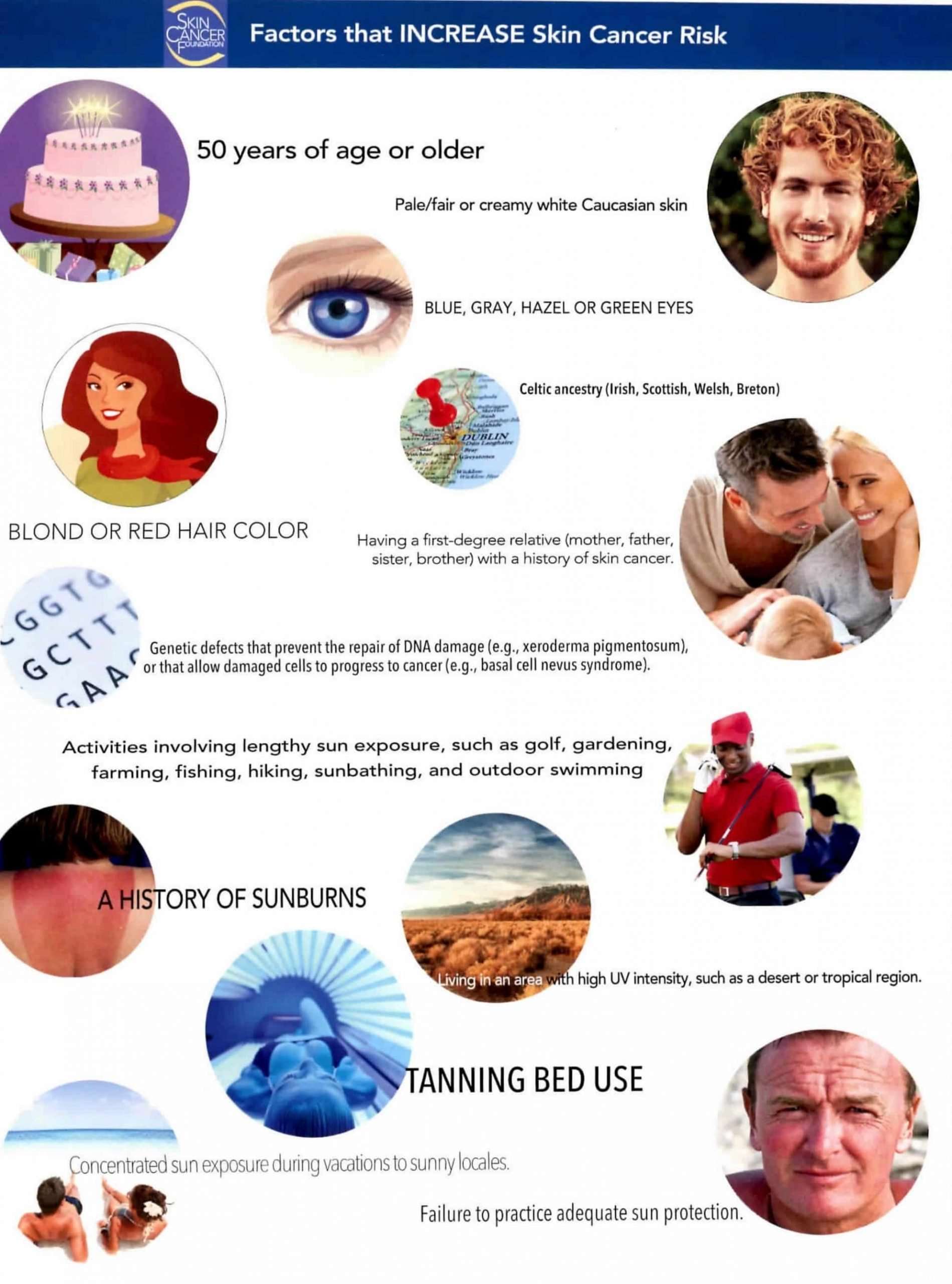
Melanoma is more than 20 times more common in whites than in African Americans. Overall, the lifetime risk of getting melanoma is about 2.6% for whites, 0.1% for Blacks, and 0.6% for Hispanics. The risk for each person can be affected by a number of different factors, which are described in Risk Factors for Melanoma Skin Cancer.
Melanoma is more common in men overall, but before age 50 the rates are higher in women than in men.
The risk of melanoma increases as people age. The average age of people when it is diagnosed is 65. But melanoma is not uncommon even among those younger than 30. In fact, its one of the most common cancers in young adults .
Skin Cancer Awareness Month: Assessing Cancer Risk Associated With Immunosuppressive Therapies
- May 14, 2021
Over the past few decades, the dermatologic care of inflammatory skin conditions has been transformed through the growing use of small molecules disease-modifying anti-rheumatic drugs and targeted biologic therapies. However, alongside the tremendous benefits offered by these therapeutic agents are concerns regarding potential adverse effects, in particular associated risks of cancer development. The controversial relationship between immunosuppressive medications frequently used in dermatologic practice and increased cancer risk is a concern which emerging research aims to mitigate. According to data recently published in Dermatologic Therapy, these agents are not significantly associated with certain cancer subtypes yet warrant caution as there is not enough research in the field.;
Examining Cancer Risk and Immunosuppressant Use
A team of researchers conducted a systematic review of online trial databases including studies focused on the evaluation of cancer risk among patients being treated with immunosuppressant agents for inflammatory cutaneous conditions. Their research aims to improve current guidance and the counseling of patients with dermatologic diseases who are considering these therapeutics as treatment pathways.
Cancer Risk and Numbers Needed to Harm
Clinical Implications
Recommended Reading: Can Basal Cell Carcinoma Be Fatal
Observed And Expected Age Of Diagnosis
We compared the observed and expected ages of diagnosis in the validation set. The expected ages of diagnosis in Fig.; were computed for each DRS-DL curve, by deriving the yearly incidence rates from the lifetime risks associated to each curve. To model the age distribution in the US population, we extracted the estimated yearly survival rates produced by the CDC for white Americans . The expected mean and SD of age of diagnosis was obtained with:
Andme Cohort And Data Collection
All participants were drawn from the customer base of 23andMe, Inc., a consumer genetics company. Participants provided informed consent and participated in the research online, under a protocol approved by the external AAHRPP-accredited IRB, Ethical & Independent Review Services . Over the course of approximately thirteen months from May 2016 to June 2017, more than 210,000 research participants responded to questions from an in-house designed cancer survey . The baseline survey contains 34 questions regarding personal history of skin cancer , 12 questions regarding the family history of skin cancer , and 23 questions regarding risk factors and exposures . The list of candidate risk factors and exposures has been compiled from two recent systematic reviews of thousands of epidemiological studies that have evaluated risks associated with a wide range of environmental and phenotypic factors,. Only participants who completed the full survey were included in the analysis. The geographical distribution of collected skin cancer across USA territory is shown in Supplementary Fig.;.
Each participant received a yearly health follow-up survey in 2018 and 2019. The survey asked if the participants received treatments or were diagnosed for the three skin cancers during the last twelve months.
Recommended Reading: What Is Squamous Cell Carcinoma
Living The Commuter Lifestyle
Do you commute to work daily? Are your car windows treated with UVB reducing tint? If not, you may be at increased risk of developing skin cancer. According to a 2010 study from St. Louis University School of Medicine, theres good reason why over three-quarters of early stage skin cancers diagnosed in the U.S. are located somewhere on the bodys left hand side.
Thats the arm you dangle out the window or prop up on the window like an arm rest! And while window glass in most North American vehicles is able to efficiently protect against UVB radiation, most car windows arent treated to block UVA rays, allowing over 60-percent to penetrate the skin on your dangly left arm. Only front windows block UVAs the material used gives resistance to shattering.
- Related
Identifying Skin Cancer Risk Factors
The demographic characteristics of the training and validation sets are described in Supplementary Table;, and the participants geographical provenance is shown in Supplementary Fig.;. We restricted analyses to participants with current age between 30 and 90 years. The sex ratio of participants was biased toward females , and close to 50% of participants reported a current age between 50 and 70 years. The age distribution and sex ratio were in line with the general characteristics of the 23andMe research cohort. The training set used to select factors and to train the predictive models contained 14,898 BCC, 7479 SCC, and 3998 melanoma cases .
We identified 32 risk factors that contributed to at least one type of skin cancer, following the procedure described in Fig.; . As the three skin cancers share common risk factors, and in order to enable comparisons, we included all 32 identified factors in each skin cancer final model. The 32-factor models explained 21.6%, 20.0%, and 19.8% of phenotypic variance of BCC, SCC, and melanoma, respectively . The following section describes the main risk factors included in these models, and their contribution to each skin cancer risk. We separated factors commonly used in skin cancer prediction models, from factors that are generally not included .
Fig. 2: Variance explained and risk factor effects in the final 32-factor models.
Don’t Miss: What Is Non Small Cell Carcinoma
Determining If The Cancer Has Spread
As part of your diagnosis, your doctor will also determine what stage the cancer is in. The different stages refer to whether and how far the cancer has spread in your body, on a Roman numeral scale of I to IV. A stage I cancer is small and contained to the body part where it originated, whereas a stage IV cancer has spread aggressively to other parts of the body.
Depending on the type of skin cancer that a person has, it may be more or less likely that it has spread through the body. For instance, basal cell skin cancer rarely spreads beyond the skin where it starts. However, melanomas and large squamous cell carcinomas are more likely to spread into other regions of the body. Cases of melanoma, in particular, may call for further tests to determine the specific stage theyre in.
Your doctor may evaluate multiple factors in order to stage the cancer. Using biopsies and imaging tests, your doctor may take a look at:
-
The size and thickness of the tumor, and whether it has grown into surrounding tissues
-
Nearby lymph nodes, to check for signs of cancer spread
Preparing For Your Appointment
If you have any concerns about the health of your skin, it is important to share them with your doctor. After making an appointment, there are steps you can take to prepare yourself and make the most of your time with your doctor.
Here are some things to consider and be prepared to discuss before visiting the clinic or hospital:
-
What symptoms are you experiencing ?
-
When did you first notice your symptoms?
-
Have there been any major changes or stressors in your life recently?
-
What medications and/or vitamins are you taking?
-
What questions do you have for your doctor?
Recommended Reading: Is Melanoma The Same As Skin Cancer
Can I Lower My Risk Of Cancer Coming Back Or Getting New Skin Cancers
If you have skin cancer, you probably want to know if there are things you can do that might lower your risk of the cancer coming back, or of getting a new skin cancer.
People who have had skin cancer are at higher risk for developing another skin cancer. Because of this, its important to limit your exposure to UV rays Rays?) and to examine your skin every month for signs of possible new skin cancers. Seeing your doctor regularly for skin exams is also important. Skin cancers that are found early are typically much easier to treat than those found at a later stage.
Smoking has been linked to an increased risk of squamous cell skin cancer, as well as to many other types of cancer. If you smoke and are thinking about quitting, call the American Cancer Society for information and support at 1-800-227-2345.
Adopting other healthy behaviors such as eating well, being active, and staying at a healthy weight might help as well, but no one knows for sure. However, we do know that these types of changes can have positive effects on your health, including lowering your risk for many other types of cancer, as well as other diseases.
Ibd And The Risk Of Skin Cancer
It’s no surprise that skin cancer is a public health problem, particularly in sunnier areas of the world. In the United States, the rate of nonmelanoma skin cancer has been on the rise. Almost everyone has had a bad sunburn or two in their lives, especially when taking a vacation to a beach or to a destination with a tropical climate. What some people with inflammatory bowel disease might not know, however, is that they are at an increased risk of developing skin cancer simply because they have IBD.
The good news is that we know about the risk, which means much can be done to avoid being exposed to too much sun. Don’t stay home and avoid travel or fun activities because of the sun! Sunscreens are a great way to limit exposure, but for those that don’t like to use them, there is UV-blocking clothing available in a wide variety of styles. Hats and umbrellas or even going into the shade are also helpful. Taking a few minutes every day to think about ultraviolet protection will go a long way to preventing future issues. Most people who develop skin cancer will be able to get treatment and avoid serious complications, especially if it is found early.
Also Check: Can Merkel Cell Carcinoma Be Cured
Melanoma: The Deadliest Skin Cancer
Melanoma is the most serious type of skin cancer, because it tends to spread if its not treated early.
This cancer starts in the melanocytes cells in the epidermis that make pigment.
About 100,350 new melanomas are diagnosed each year.
Risk factors for melanoma include:
- Having fair skin, light eyes, freckles, or red or blond hair
- Having a history of blistering sunburns
- Being exposed to sunlight or tanning beds
- Living closer to the equator or at a higher elevation
- Having a family history of melanoma
- Having many moles or unusual-looking moles
- Having a weakened immune system
Melanoma can develop within a mole that you already have, or it can pop up as a new dark spot on your skin.
This cancer can form anywhere on your body, but it most often affects areas that have had sun exposure, such as the back, legs, arms, and face. Melanomas can also develop on the soles of your feet, palms of your hands, or fingernail beds.
Signs to watch out for include:
- A mole that changes in color, size, or how it feels
- A mole that bleeds
RELATED: The Difference Between Chemical and Mineral Sunscreen
Causes Of Skin Cancer

One of the main causes of skin cancer is being exposed to UV rays. UV rays are invisible, and are produced by the sun, and tanning equipment.
UV rays cause skin cancer by creating changes in the cells of your skin. In some cases, the UV rays cause direct damage to your cells. Tans and sunburns, for example, are both signs that UV rays have damaged your skin. In other cases, UV rays cause skin cancer indirectly, by weakening the immune system.
Many studies on skin cancer show that people who have suffered many severe sunburns in childhood are at greater risk of developing skin cancer. Family history, some chemical exposures, and immune dysfunction conditions can also create a greater risk of developing skin cancer.
Recommended Reading: How Do You Know If You Have Melanoma
What Is The Uv Index
In order to address the growing concern by Canadians regarding changes in UVR resulting from ozone depletion, Environment Canada rates the UV intensity as UV Index on a scale of 0 to 11+ . It can go to the mid-teens at midday in the tropics. In Canada the UV Index is categorized into low , moderate , high , very high and extreme .
The human health effects and precautions relating to the UV Index are summarized in the following table.
| Table 3 | ||
|---|---|---|
| Very High |
|
|
| 11+ | Extreme |
|
Sun Protection Messages, Environment and Climate Change Canada
Global Solar UV Index: A Practical Guide. A joint recommendation of the World Health Organization, World Meteorological Organization, United Nations Environment Programme, and the International Commission on Non-Ionizing Radiation Protection.
Basal Cell Skin Cancer
Basal cell cancer can occur anywhere on the body, but it typically develops on areas regularly exposed to the sun. This type of cancer may appear on your face, neck, or other body parts in the form of:
-
Flat patches of spots, or lesions, which may be red, purple, or brown in color
-
Slightly raised, brown or reddish lesions
-
Fully raised, bumpy lesions with a red or brown color
If you think you may be experiencing any of the symptoms of different skin cancers described above, you should call a doctor to discuss your symptoms. You may find that you simply have a large, non-cancerous mole, and can have your concerns put to rest by a professional. On the other hand, your doctor may be able to diagnose your condition and recommend treatment sooner rather than later. Either way, it is best to be on the side of caution and speak with your doctor about what youve noticed.
Don’t Miss: How Common Is Renal Cell Carcinoma
Major Types Of Skin Cancers And Their Distribution In People Of Color
Skin cancer is mainly divided into two main categories as Non melanoma Skin Cancer and Melanoma Skin Cancer . Non-Melanoma Skin Cancer includes basal cell carcinoma and squamous cell carcinoma . Each of these most common cancers viz. Basal cell carcinoma , squamous cell carcinoma , and melanoma is named after the type of skin cell from which it arises and has been linked to the varying degree of sun exposure .
NMSC greatly outnumber melanomas in incidence but fortunately most are much easier to treat and have much better long-term prognosis . They are less deadly than melanoma mainly due to their tendency to remain confined to their primary site of disease which makes their management much more straightforward. The devastating majority of keratinocyte malignancies progress in the areas of skin most exposed to UV such as on the face and arms . The BCC and the SCCs often carry a UV-signature mutation indicating that these cancers are caused by UV-B radiation via the direct DNA damage . Although Asians display relative protection from basal cell carcinoma and squamous cell carcinoma, incidence rates of these non melanoma skin cancers have been increasing over 3 to 8 percent annually in the past three decades . Features of different types of skin cancers are listed in .
Nevoid Basal Cell Carcinoma Syndrome
Nevoid basal cell carcinoma syndrome, also known as Gorlin syndrome, is an autosomal dominant cancer syndrome in which the risk of basal cell carcinoma is very high. The disease is characterized by basal cellnevi, jaw keratocysts and skeletal abnormalities. Estimates of nevoid basal cell carcinoma syndrome prevalence varies, but is approximately 1 in 60000. The presence of basal cell carcinoma is much higher in white than black individuals; 80% and 38%, respectively. Odontogenic keratocysts are found in approximately 75% of individuals with the disease and often occur early in life. The most common skeletal abnormalities occur in the head and face, but other areas are often affected such as the rib cage. The causative genetic mutation of this disease occurs in the PTCH gene, and the product of PTCH is a tumor suppressor involved in cell signaling. Although the exact role of this protein in nevoid basal cell carcinoma syndrome is not known, it is involved in the hedgehog signaling pathway, known to control cell growth and development.
Recommended Reading: Can You See Skin Cancer