Disclosure Of Potential Conflicts Of Interest
S. Sokol has ownership interests in Foundation Medicine. G.M. Frampton has ownership interests in Roche. V.A. Miller is an employee of Foundation Medicine and Revolution Medicines. L.A. Albacker has ownership interests at Roche. H.L. McLeod has ownership interests at Cancer Genetics and Interpares Biomedicine, reports receiving speakers bureau honoraria from Illumina and Genentech, and is a consultant/advisory board member for Pharmazam and Admera Health. Z. Eroglu is a consultant/advisory board member for Array and Regeneron. N.I. Khushalani has ownership interests at Bellicum Pharmaceuticals, Amarin Corp., Mazor Robotics, and TransEnteriz is a consultant/advisory board member for Bristol-Myers Squibb, HUA, Merck, EMD Serono, Array, Regeneron, Immunocore, and Genentech reports receiving commercial research grants to his institute from Bristol-Myers Squibb, Merck, HUYA Bioscience, GlaxoSmithKline, Amgen, Regeneron, Celgene, and Novartis and has been on the Data and Safety Monitoring Board for AstraZeneca. V.K. Sondak is a consultant/advisory board member for Merck, Bristol-Myers Squibb, Regeneron, Pfizer, Novartis, Array, Genentech/Roche, and Polynoma. J.A. DeCaprio is a consultant/advisory board member for Merck Sharp & Dohme and reports receiving commercial research grants from Constellation Pharmaceuticals. K.Y. Tsai is a consultant/advisory board member for Merck. No potential conflicts of interest were disclosed by the other authors.
Stages Of Merkel Cell Carcinoma
After receiving a cancer diagnosis, your doctor will run tests to find out if the cancer has spread to other parts of your body. This is referred to as staging. Staging is important for determining what types of treatment are needed.
In general, a higher number stage means the further a cancer has spread. There are five main stages in MCC :
- stage 0: the cancer is only in the epidermis and hasnt spread to the lymph nodes
- stage 1: the cancer is less than 2 centimeters across and hasnt grown into the lymph nodes
- stage 2: the cancer is more than 2 cm across and hasnt spread to the lymph nodes
- stage 3: the cancer has grown into lymph nodes as well as nearby tissues
- stage 4: the cancer has spread to nearby tissues, the lymph nodes, and distant sites, such as the lungs, bones, or brain
The main symptom of Merkel cell carcinoma is the appearance of a single lump or nodule on the skin. The lump is typically:
- red or violet in color
- firm to the touch
- fast-growing
- painless
The nodule can form anywhere on the body, but most often appears on areas regularly exposed to sunlight, such as the:
- face
- neck
- arms
If the cancer spreads to the lymph nodes, the nodes may grow large enough to be seen as lumps under the skin.
Merkel cell carcinoma can look like many other types of skin cancer at first, so a definitive diagnosis usually isnt made until after a biopsy. Other types of skin cancers often present with:
Is Skin Cancer Genetic
40-50% of Americans who live to the age of 65 will have skin cancer at least once. The most common types of skin cancer in the United States are basal cell carcinoma and squamous cell carcinomas. These are referred to as non-melanoma skin cancers and are generally the result of sun exposure. Learn more about the effects of UV exposure.
Approximately one in 60 people will develop invasive, cutaneous melanoma during their lifetime. Malignant melanoma is a cancer that begins in the melanocytes, the pigment-producing cells in the skin. In fair-complexioned individuals worldwide, the majority of melanoma cases are related to environmental factors such as excessive ultraviolet radiation . However, about 5-10% of melanoma cases are inherited in an autosomal dominant fashion. In other words, parents with a defined genetic mutation have a 50/50 chance to pass on the susceptibility to each of their children regardless of gender. Learn more about melanoma.
Learn more about genetic testing or make an appointment with our experts at the Skin Cancer Program.
Recommended Reading: What Does Stage 3b Melanoma Mean
Read Also: Large Cell Carcinoma Definition
What We Do Know
UV exposure creates a double threat for MCC
Not only does UV exposure cause damage that increases your skin cancer risk it also suppresses your immune system, reducing its ability to repair damage and fight skin cancers and other diseases. No matter the source of UV radiation, there is a clear and dangerous correlation between exposure and MCC.
Immunosuppression and MCC are strongly linked.
If your immune system is persistently weakened or suppressed, you are about 15 times more likely to develop MCC than people with healthy immune systems. However, more than 90 percent of MCC cases arise in people with no known immune problems. Immunosuppression can be caused by:
- Diseases such as HIV and certain cancers including chronic lymphocytic leukemia and lymphomas.
- Immunosuppressant medications used for transplant recipients and for autoimmune diseases including lupus, psoriasis, Crohns disease and rheumatoid arthritis.
Immunosuppressed MCC patients often develop the disease at a far younger age about half of MCCs in these patients occur before age 50.
If your immune system is suppressed, talk to your doctors about your chances of developing MCC, and be sure to protect yourself against other risk factors, especially UV exposure.
A history of skin cancer is also highly associated with Merkel cell carcinoma. If youve had melanoma, squamous cell carcinoma, basal cell carcinoma or Bowens disease skin cancers frequently caused by UV exposure you are more likely to develop MCC.
What Does Mcc Look Like
MCC tumors often, but not always, appear on sun-exposed areas of the body. The tumors are not nearly as distinctive as other skin cancers and can appear as a pearly pimple-like lump, sometimes skin-colored, red, purple or bluish-red, though they are rarely tender to the touch. The rapid speed at which they grow is what often causes patients and doctors to take notice.
A recurrence of Merkel cell carcinoma on the forehead.
Merkel cell carcinoma on the lower leg.
Please note: Since not all Merkel cell carcinomas have the same appearance, these photos serve as a general reference for what MCC can look like. If you see something new, changing or unusual on your skin, schedule an appointment with your doctor. Photos courtesy of Paul Nghiem, MD, PhD
Read Also: Invasive Ductal Breast Cancer Prognosis
What Complications Are Associated With Merkel Cell Carcinoma
Left untreated, Merkel cell carcinoma may quickly metastasize to other tissues and organs. Generally, MCC is much more difficult to treat if it has spread. In addition, MCC often does come back after treatment. MCC can be fatal. The mortality rate associated with MCC ranges from approximately 33 to 46 percent.
Is Merkel Cell Cancer Hereditary & Is Carcinoma Worse Than Melanoma
Merkel cell cancer or MCC is an aggressive but rare type of skin cancer, which mainly develops in the form of a painless and single bump on the skin often exposed to the sun. The bump, in this case, maybe of red-violet or skin color and grows rapidly within a period of few weeks to months. Even cancer spreads quickly to surrounding lymph nodes and tissues, along with large numbers of distant body parts. A history related to extensive exposure to the sun, chronic immune suppression, fair skin, age and polyomavirus associated with Merkel cells is prime factors related to the development of Merkel cell cancer.
You May Like: What Is The Survival Rate For Invasive Lobular Carcinoma
Iii Small Cell Carcinoma Of Gynecologic Tract
The SmCC of gynecologic tract is one of the common EPSmCCs, representing up to 2% of all gynecologic malignancies . Reported gynecologic sites include the cervix, endometrium, ovary, fallopian tube, vagina and vulva.
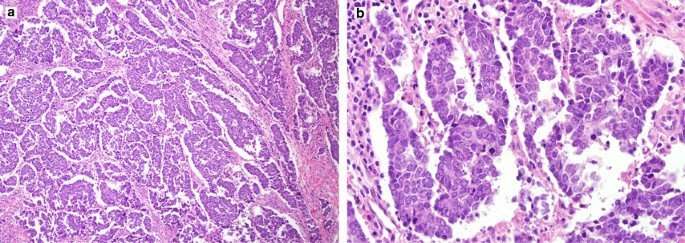
1. Small cell carcinoma of the uterine cervix
The uterine cervix is the most common gynecologic tract site involved with EPSmCCs. However, SmCCC is a very rare disease, representing only 1% to 3% of all uterine cervical cancers. SmCCC often coexists with conventional squamous cell carcinoma or adenocarcinoma. Depending on the series analyzed and the selection criteria employed, between 11% and 64% of SmCCC cases present admixed histology . Immunohistochemical studies have further revealed that the majority of cases show diffuse nuclear and cytoplasmic p16 positivity .
The critical role of human papillomaviruses in the carcinogenesis of conventional cervical cancer is well established. The prevalence of the different high-risk HPV types in SmCCC has been preliminarily established and reported to range from 50% to 100% . It has been found that unlike in squamous cell carcinoma of the cervix, HPV 18 may be the most prevalent type of SmCCC . Given this evidence, SmCCC, like other types of cervical cancer, seems to be associated with high-risk HPV infection. For the purpose of differential diagnosis, HPV is specific for SmCC of cervical origin other than ovary or lung, but p16 immunohistochemistry is not useful for this purpose .
2. Small-cell carcinoma of the ovary
Massively Parallel Sequencing Of Patient Samples
Adequate tissue for DNA extraction was available from 4 archival patient specimens, and the blocks were selected for further analysis utilizing the Ion AmpliSeq CCP on Ion Proton instrumentation to assess somatic mutational spectra. The CCP is a multiplex PCR-based 409 gene-targeted panel with rapid high-throughput assessment of mutations based on the Wellcome Trust Sanger Institute’s Cancer Gene Census. Within our data set, we called an average of 4,606 variants per patient . One sample was found to maintain elevated variants at 12,226 called variants . This is not unexpected as this specimen which was processed in higher-concentration formalin had been archived for a prolonged period of time of > 10 years . However, concomitant variants and deleterious mutations were detected within all genes that were interrogated within synonymous loci.
You May Like: Metastatic Melanoma Cancer Life Expectancy
What You Can Do
- Examine your skin head-to-toe every month.
- See your dermatologist every year for a professional skin exam. If you are newly diagnosed with MCC, seek a consultation with a multidisciplinary expert. Find a specialist here.
- If youve had an MCC, follow up regularly with your dermatologist once treatment is complete. Follow the exam schedule your doctor recommends its the best way to quickly detect a recurrence. Consider getting the AMERK biomarker blood test that can help detect recurrences early. Learn more here.
- Safeguard your skin and avoid unprotected UV exposure. It is the single most effective way to reduce your risk of developing MCC.
- Practice sun-safe habits, such as seeking shade and wearing protective clothing, a wide-brimmed hat and UV-blocking sunglasses. Use a broad-spectrum sunscreen every day. Sunscreen is a good defense against premature aging and skin cancer. Its never too late to start wearing it!
Reviewed by:
Sitc : How Genetic Reprogramming Of Merkel Cell Carcinoma May Impact Mhc
Jordan Green, PhD, of Johns Hopkins University, Baltimore, Maryland, and colleagues attempted to genetically reprogram cells of Merkel cell carcinoma to express their own immunostimulatory cytokines and co-stimulatory molecules. Their findings, presented during the 2021 Society for Immunotherapy of Cancer Annual Meeting , concluded that signal 2/3 nanoparticles have the potential to reprogram these cells, achieving immune response and increased major histocompatibility complex -I expression.
Biodegradable poly nanoparticles were used to co-deliver plasmids that encoded a signal 2 and two signal 3 molecules into cancer cells. In vitro evaluation used two patient-derived cell lines of Merkel cell carcinoma that had low baseline expression of MHC-I: MCC13 and UISO. In vivo evaluation was performed by implanting subcutaneous melanoma tumors into C57BL/6J mice and injecting nanoparticles into the tumor.
Compared with controls, MHC-I expression was increased 1.6- and 5.0-fold in MCC13 and UISO cell lines, respectively MHC-II expression was increased 1.6- and 6.3-fold. When co-cultured with human peripheral blood mononuclear cells, signal 2/3 particles demonstrated significantly reduced viability of Merkel cell carcinoma as well as increased leukocyte proliferation.
Disclosure: No disclosure information was provided.
You May Like: Prognosis Of Skin Cancer
Cancer May Spread From Where It Began To Other Parts Of The Body
When cancer spreads to another part of the body, it is called metastasis. Cancer cells break away from where they began and travel through the lymph system or blood.
- Lymph system. The cancer gets into the lymph system, travels through the lymph vessels, and forms a tumor in another part of the body.
- Blood. The cancer gets into the blood, travels through the blood vessels, and forms a tumor in another part of the body.
The metastatic tumor is the same type of cancer as the primary tumor. For example, if Merkel cell carcinoma spreads to the liver, the cancer cells in the liver are actually cancerous Merkel cells. The disease is metastatic Merkel cell carcinoma, not liver cancer.
What Is A Merkel Cell
Merkel cells are located deep in the top layer of skin. Merkel cells are connected to nerves, signaling touch sensation as touch receptors. MCC was named after Merkel cells due to the similar microscopic features however, recent research suggests that it is unlikely that MCC originates directly from normal Merkel cells.
Normal Merkel cells in the skin: In this illustration of a cross-section of the skin, normal Merkel cells are shown in red and connect to nerves shown in yellow. The structures drawn include the epidermis , dermis , and deeper adipose layer containing the fatty tissue. Arteries are depicted in red and veins are blue. Figure copyright by Paul Nghiem & Quade Medical Group.
Recommended Reading: What Does Stage 3b Melanoma Mean
Recommended Reading: What Is Stage 2 Squamous Cell Carcinoma
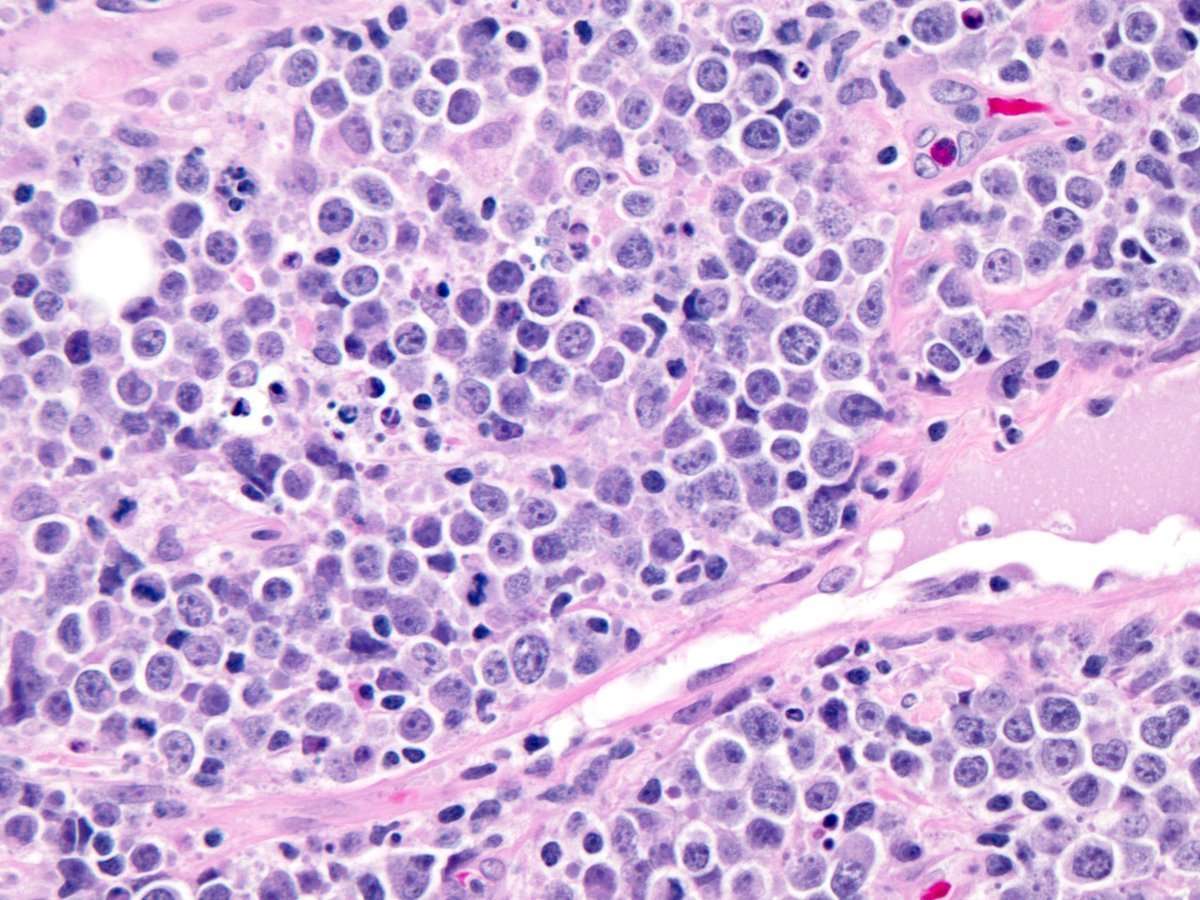
V The Origin Of Small Cell Carcinoma
The identification of the cell type from which small cell carcinoma originates is critical in the development of methods for early diagnosis and treatment.
1. The cell of origin for small cell lung cancer
The usage of cell type-restricted Adeno-Cre vectors to distinct cell populations in the lung of adult mouse showed that loss of TP53 and RB1 can efficiently transform neuroendocrine and Surfactant Protein C -expressing cells to SCLC, albeit SPC-expressing cells at a lesser efficiency. In contrast, Clara cells were largely resistant to transformation. These results indicate that although neuroendocrine cells serve as the predominant cell of origin for SCLC, a subset of SPC-expressing cells may also be endowed with this ability .
2. The cell of origin for EPSmCCs
Other theories of histogenesis include metaplasia from other high-grade malignancies. Neuroendocrine cells are detected by IHC in some in-situ cervical adenocarcinomas, and these may be the origin of cervical NE carcinomas . Further support for this theory comes from a study where identical loci with loss of heterozygosity were demonstrated in mixed adenocarcinoma and EPSmCC of the appendix, and an additional locus was found in the EPSmCC component . Similarly, additional loci with loss of heterozygosity were noted in breast EPSmCC compared with adjacent ductal carcinoma in situ.
How Is Merkel Cell Carcinoma Treated
Your treatment plan depends on how early your doctor diagnoses the cancer, your overall health, and whether cancer cells have spread to other tissues in your body. Treatment for MCC usually involves one or a combination of therapies, including:
- Immunotherapy, which uses specific medications to help your immune system fight cancer. Immune agents in use for MCC include avelumab , nivolumab, and pembrolizumab .
- Surgery, which is a procedure that cuts out cancerous tissues. This type of therapy often involves a type of surgery called Mohâs micrographic surgery, a layer-by-layer skin removal method. Mohâs allows doctors to assess tissue under a microscope during the treatment and to save skin appearance and function. This is especially beneficial to people who have cancer on their faces.
- Radiation therapy, which uses highly charged particles to kill cancer cells. This method is often combined with Mohâs surgery to improve results.
- Chemotherapy, which uses drugs to kill cancer. This method of treatment was previously used more often, but was not found to give lasting results.
Read Also: Invasive Ductal Breast Cancer Survival Rate
The Genomic Landscape Of Merkel Cell Carcinoma And Clinicogenomic Biomarkers Of Response To Immune Checkpoint Inhibitor Therapy
Corresponding Authors:Corresponding Authors:
Note: Supplementary data for this article are available at Clinical Cancer Research Online .
T.C. Knepper and M. Montesion contributed equally to this article.
Corresponding Authors:
Clin Cancer Res 2019 25:596171
- H. Lee Moffitt Cancer Center & Research Institute
- Award Id:
Clin Cancer Res
Todd C. Knepper, Meagan Montesion, Jeffery S. Russell, Ethan S. Sokol, Garrett M. Frampton, Vincent A. Miller, Lee A. Albacker, Howard L. McLeod, Zeynep Eroglu, Nikhil I. Khushalani, Vernon K. Sondak, Jane L. Messina, Michael J. Schell, James A. DeCaprio, Kenneth Y. Tsai, Andrew S. Brohl The Genomic Landscape of Merkel Cell Carcinoma and Clinicogenomic Biomarkers of Response to Immune Checkpoint Inhibitor Therapy. Clin Cancer Res 1 October 2019 25 : 59615971.
Patient Demographics And Clinical Course
Retrospective chart reviews conducted from 1993 to 2013 identified 5 patients treated at our institution and diagnosed with MCC. Patients fell within the typical diagnostic criteria with all being Caucasian males > 60 years of age . Patients were referred to the clinic following the identification of characteristic MCC nodules. Interestingly, 80% patients presented with a past history of colon adenocarcinoma and actinic keratosis . One patient was incidentally diagnosed and treated with wide-band excision of the forehead. Three patients underwent direct biopsy with subsequent subtotal resection and 4/5 patients underwent gross total salvage resection. Postoperative scans demonstrated marked disease reduction. Two patients completed follow-up radiation therapy while 1 patient underwent chemotherapy alone. Eighty percent of patients presented with a history of skin cancer and dermatological disorders at diagnosis .
Table 1
Patient demographics, pathology, treatment parameters, and relevant clinical comorbidities
Also Check: What Is The Survival Rate Of Invasive Ductal Carcinoma
Validation Of Single Nucleotide Variants By Sanger Sequencing
Selected single-nucleotide variations affecting AKT1, PIK3CA, RB1, TP53, EZH2, PTCH1, TSC1, and BAP1 were validated by PCR amplification using new or previously reported primer pairs ,, , followed by Sanger sequencing at the University of Michigan Sequencing Core. Chromatograms were visualized using Sequence Scanner 2 software.