How Is Basal Cell Carcinoma Diagnosed
BCC is diagnosed clinically by the presence of a slowly enlarging skin lesion with typical appearance. The diagnosis and histological subtype is usually confirmed pathologically by a diagnostic biopsy or following excision.
Some typical superficial BCCs on trunk and limbs are clinically diagnosed and have non-surgical treatment without histology.
Basal Cell Carcinoma Prognosis
Most basal cell carcinoma causes are preventable diagnosis at sufficiently early stages is associated with a high cure rate. This means that BCC is rarely fatal. Similarly, rodent ulcers are rare as most treatments are curative.
Mohs micrographic surgery has the highest cure rate only 2.5% of patients experience recurrence after a term of five years, although not all tumors are eligible for this procedure. High-heat treatments are associated with a 7.7% five-year recurrence rate.
Patients who refuse surgery or have tumors in difficult-to-reach areas can expect control of tumor growth in 85% 95% of cases with radiotherapy. This option is usually only recommended for frailer, older patients.
In cases that have not metastasized, basal cell cancer is 100% curable. When metastasis occurs , basal cancer cells are most likely to settle in the lungs.
Metastatic basal cell carcinoma prognosis is poor with death occurring within four and a half years for most patients. However, it is extremely rare to find cases of advanced BCC. Today, targeted therapies can increase overall survival rates even for locally advanced and metastatic BCCs.
Risk Factors For Melanoma
This section focuses on risk factors in individuals at increased hereditary risk of developing melanoma.
Sun exposure
Sun exposure is well established as a major etiologic factor in all forms of skin cancer, although its effects differ by cancer type. The relationship between sun exposure, sunscreen use, and the development of skin cancer is complex. It is complicated by negative confounding . These subjects are genetically susceptible to the development of skin cancer by virtue of their cutaneous phenotype and thus may develop skin cancer regardless of the amount of sunlight exposure or the sun protection factor of the sunscreen.
Pigmentary characteristics
Clinically, several pigmentary characteristics are evaluated to assess the risk of melanoma and other types of skin cancer. These include the following:
- Fitzpatrick skin type. The following six skin phenotypes were defined on the basis of response to sun exposure at the beginning of summer.
- Type I: Extremely fair skin, always burns, never tans.
- Type II: Fair skin, always burns, sometimes tans.
- Type III: Medium skin, sometimes burns, always tans.
- Type IV: Olive skin, rarely burns, always tans.
- Type V: Moderately pigmented brown skin, never burns, always tans.
- Type VI: Markedly pigmented black skin, never burns, always tans.
- Number of nevi or nevus density.
- Abnormal or atypical nevi.
- Freckling.
Nevi
Family history
Personal history of melanoma
Personal history of BCC or SCC
Recommended Reading: Invasive Ductal Breast Cancer Prognosis
Nevoid Basal Cell Carcinoma Syndrome
Title
- Abnormal deposits of calcium in the brain
- Skeletal abnormalities
- Skin pits on the hands and feet
- Large head size
- of the heart
- Noncancerous tumors of the ovary
This table lists symptoms that people with this disease may have. For most diseases, symptoms will vary from person to person. People with the same disease may not have all the symptoms listed. This information comes from a database called the Human Phenotype Ontology . The HPO collects information on symptoms that have been described in medical resources. The HPO is updated regularly. Use the HPO ID to access more in-depth information about a symptom.
|
| 80%-99% of people have these symptoms | |
| Cerebral calcification | |
| 30%-79% of people have these symptoms | |
| Abnormality of the neck | |
| Increased breadth of bridge of nose Increased breadth of nasal bridge Increased width of bridge of nose Increased width of nasal bridge Nasal bridge broad | |
| 5%-29% of people have these symptoms | |
| Abnormality of the sense of smell | Abnormal sense of smell |
| Clouding of the lens of the eye Cloudy lens | |
| Increased projection of lower jaw Increased size of lower jaw Large lower jaw | |
| Percent of people who have these symptoms is not available through HPO | |
| Abnormal sternum morphology | |
| Short distal phalanx of the thumb | Short outermost bone of the thumb |
- Cardiologist
Patient Health And Supportive Care
Given the complex nature of everyday functions within the head and neck area, the inherent consequences of HNSCC and its treatment and the increasing choices of treatments have a large effect on the health-related QOL of patients with HNSCC.
The wide array and combinations of treatments all have their specific sequelae, including physical, emotional, functional, social, and occupational dysfunction, as well as a profound effect on the families of patients with HNSCC. Furthermore, HRQOL is significantly associated with survival,. For example, a clinically meaningful association exists between HRQOL scores measured at diagnosis and overall survival of patients after treatment . Depending on the primary tumour site, patients with HNSCC might be confronted with specific symptoms, such as oral dysfunction and swallowing and speech problems, during treatment, which often improve 6 months after treatment. However, long-term reduction in QOL in HNSCC survivors is common. On average, overall HRQOL deteriorated by 11% when compared with pre-treatment, and by 15% when compared with years 1 and 2 post-treatment.
Read Also: Does Skin Cancer Make You Lose Hair
What Role Do Genetics Play In Skin Cancer
While we know that exposure to ultraviolet rays from the sun and tanning beds increase your risk for skin cancer, your genetics, or family history, can also be a factor for developing certain kinds of skin cancer.
According to the Skin Cancer Foundation, about 10 percent of all people who are diagnosed with melanoma have a family member who has had melanoma at some point in their lifetime.
So if one of your close biological relatives, such as a parent, sister, or brother, has had melanoma, youre at an increased risk.
Additionally, if you have a family history of melanoma and you also have a lot of unusual moles, youre at a higher risk for developing this type of cancer.
Moles that are considered unusual or atypical tend to have one or more of the following characteristics:
- asymmetrical
- an irregular or jagged border
- the mole is different shades of brown, tan, red, or black
- the mole is more than 1/4 inch in diameter
- the mole has changed size, shape, color, or thickness
The combination of unusual moles and a family history of skin cancer is known as familial atypical multiple mole melanoma syndrome .
People with FAMMM syndrome are 17.3 times more likely to develop melanoma versus people who dont have this syndrome.
Researchers have also discovered that certain defective genes can be inherited. This can increase your risk for developing skin cancer.
Initiating And Early Events
HPV-negative HNSCC.
Tobacco consumption is the primary risk factor for development of HPV-negative HNSCC. Tobacco consists of over 5,000 different chemicals, of which dozens have been shown to have carcinogenic activity. The chemicals thought to be most responsible for the cancer-causing effects of tobacco are polycyclic aromatic hydrocarbons , including benzopyrene, and nitrosamines, including 4–1–1-butanone and N-nitrosonornicotine ,. In smokeless tobacco, nitrosamines are the dominant carcinogen, whereas the carcinogens in areca nut and betel quid are poorly defined. Tobacco-derived carcinogens, including PAHs and nitrosamines, undergo metabolic activation, with detoxication enzymes and pathways promoting excretion . However, many of the reactive metabolites of these carcinogens can also form covalent DNA adducts, which, if not properly repaired, lead to mutations and other genetic abnormalities. The propensity for tobacco carcinogens to promote genetic changes and neoplastic transformation likely depends on the balance between metabolic activation versus detoxification and DNA repair . The use of tobacco products is also associated with inflammation in the exposed tissues. Coincident with inflammation is the local production of cytokines, chemokines and growth factors that can have an important role in promoting proliferation, angiogenesis and, ultimately, carcinogenesis.
Development of carcinogen-associated, HPV-negative HNSCC.
HPV-positive HNSCC.
Recommended Reading: Can You Die From Basal Cell Skin Cancer
What To Look For
Although skin cancers can occur in non-sun-exposed areas, the most common location for BCC is the face.
- A persistent, non-healing sore that persists for 3+ weeks, bleeds, oozes or crusts
- A reddish patch or irritated area that frequently seen on chest, shoulders, arms, or legs. This patch can be itchy, painful and/or crusted
- A shiny bump or nodule that is pearly or translucent, pink, red, or white in colour. Can be tan, brown or black, especially on dark-haired people
- A pink growth that is slightly elevated, and might have a rolled border, crusted indentation in the centre and/or tiny blood vessels that may develop on the surface
- A scar-like area that is white, yellow or waxy, often has poorly defined borders, and appears shiny and taut. Note: This can indicate the presence of an aggressive tumour
Frequently, two or more features are present in one tumour. In addition, basal cell carcinoma sometimes resembles non-cancerous skin conditions such as psoriasis or eczema.
Structure Of The Skin
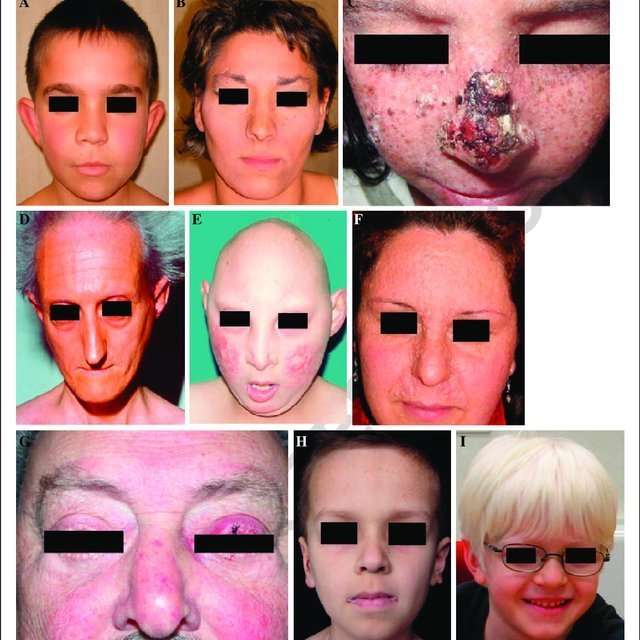
The genetics of skin cancer is an extremely broad topic. There are more than 100 types of tumors that are clinically apparent on the skin many of these are known to have familial components, either in isolation or as part of a syndrome with other features. This is, in part, because the skin itself is a complex organ made up of multiple cell types. Furthermore, many of these cell types can undergo malignant transformation at various points in their differentiation, leading to tumors with distinct histology and dramatically different biological behaviors, such as squamous cell carcinoma and basal cell cancer . These have been called nonmelanoma skin cancers or keratinocyte cancers.
Figure 1 is a simple diagram of normal skin structure. It also indicates the major cell types that are normally found in each compartment. Broadly speaking, there are two large compartmentsthe avascular epidermis and the vascular dermiswith many cell types distributed in a connective tissue matrix, largely created by fibroblasts.
The true cytologic origin of BCC remains in question. BCC and basal cell keratinocytes share many histologic similarities, as is reflected in the name. Alternatively, the outer root sheath cells of the hair follicle have also been proposed as the cell of origin for BCC. This is suggested by the fact that BCCs occur predominantly on hair-bearing skin. BCCs rarely metastasize but can invade tissue locally or regionally, sometimes following along nerves.
Recommended Reading: What Is Braf Testing In Melanoma
What Is Nevoid Basal Cell Carcinoma Syndrome
Nevoid Basal Cell Carcinoma Syndrome is also known as Gorlin syndrome. NBCCS is a hereditary condition characterized by multiple basal cell skin cancers. Other common signs include jaw cysts, pits on the palms of the hands or soles of the feet, calcium deposits in the brain, developmental disability, and skeletal changes. The appearance of a person with NBCCS may include a larger head size, a prominent forehead, broad bridge of the nose, widely spaced eyes, skin cysts, and small skin bumps called milia. The jaw cysts and basal cell skin cancers may develop in the first 10 years of a persons life, but they may not appear until the teenage years or any time during adulthood. Children with NBCCS may have the appearance features described above, including pits on their hands and feet. There is a small chance for children with NBCCS to develop a type of brain cancer called medulloblastoma. Rarely, benign growths in the ovaries and heart may also be found.
What Is The Treatment For Advanced Or Metastatic Basal Cell Carcinoma
Locally advanced primary, recurrent or metastatic BCC requires multidisciplinary consultation. Often a combination of treatments is used.
- Radiotherapy
- Targeted therapy
Targeted therapy refers to the hedgehog signalling pathway inhibitors, vismodegib and sonidegib. These drugs have some important risks and side effects.
Recommended Reading: What Happens If You Pick At A Basal Cell Carcinoma
Putative Genes For Basal Cell Carcinoma
BRCA1-associated protein 1
Pathogenic variants in the BAP1 gene are associated with an increased risk of a variety of cancers, including cutaneous melanoma and uveal melanoma. Although the BCC penetrance in individuals with pathogenic variants in BAP1 is not known, there are several BAP1 families that report diagnoses of BCC. In one study, pathogenic variant carriers from four families reported diagnoses of BCC. Tumor evaluation of BAP1 showed loss of BAP1 protein expression by immunohistochemistry in BCCs of two germline BAP1 pathogenic variant carriers but not in 53 sporadic BCCs. A second report noted that four individuals from families with BAP1 germline pathogenic variants were diagnosed with a total of 19 BCCs. Complete loss of BAP1 nuclear expression was observed in 17 of 19 BCCs from these individuals but none of 22 control BCC specimens. Loss of BAP1 nuclear expression was also reported in a series of 7 BCCs from individuals with loss of function BAP1 variants, but only in 1 of 31 sporadic BCCs.
Common Skin Cancer Can Signal Increased Risk Of Other Cancers
Frequent skin cancers due to mutations in genes responsible for repairing DNA are linked to a threefold risk of unrelated cancers, according to a Stanford study. The finding could help identify people for more vigilant screening.
Basal cell carcinomas are common. More than 3 million cases a year are diagnosed nationwide.jax10289/Shutterstock.com
People who develop abnormally frequent cases of a skin cancer known as basal cell carcinoma appear to be at significantly increased risk for developing of other cancers, including blood, breast, colon and prostate cancers, according to a preliminary study by researchers at the Stanford University School of Medicine.
The increased susceptibility is likely caused by mutations in a panel of proteins responsible for repairing DNA damage, the researchers found.
We discovered that people who develop six or more basal cell carcinomas during a 10-year period are about three times more likely than the general population to develop other, unrelated cancers, said Kavita Sarin, MD, PhD, assistant professor of dermatology. Were hopeful that this finding could be a way to identify people at an increased risk for a life-threatening malignancy before those cancers develop.
Sarin is the senior author of the study, which was published online Aug. 9 in JCI Insight. Medical student Hyunje Cho is the lead author.
Don’t Miss: What Does Stage 3b Melanoma Mean
Hedgehog Pathway And Cancer
Based on complementary DNA sequence, patched is predicted to encode a large glycoprotein with 12 membrane-spanning domains and two large extracellular loops . The patched gene product has no known homology to any other protein or protein motif but does have some characteristics suggestive of a receptor or transporter. Patched does not resemble any known tumor suppressor genes, although there are several membrane proteins involved in intercellular adhesion and signaling that function as tumor suppressors .
Expression of patched in normal skin, cultured keratinocytes, and six sporadic basal cell carcinomas . Northern blot analysis showed variable expression of the patched transcript in total RNA from tumors. The message was not detected in total RNA from normal skin, but a faint band was detected in total RNA from cultured keratinocytes. The variable expression in tumors probably reflects the relative stability of the mutant message. Reproduced from , with permission from Nature Genetics .
Confirmation Of Each Tumor And Cyst
One male patient met four of the major criteria of the Gorlin syndrome, with the existence of PTCH1 and PTCH2 mutations in his normal oral tissue . Eight tumors were individually removed from skin lesions at different sites to identify additional mutations. Dermal cyst samples were obtained from the third and fifth fingers, and mandibular OKC samples were collected. Genomic DNA samples from the eight tumors and three cyst samples were extracted and evaluated. Four of the eight samples met the next-generation sequencing criteria and were subsequently analyzed using exome sequencing analysis. Three of the four samples were derived from the patient’s back , while the other was derived from the back of the patients lower leg .
Fig. 1
Histologic analysis of the tumors and cysts. a A schema of the positions of the BCCs . b A schema of the positions of the epidermal cysts . c Histologic analysis of the basal cell carcinomas . Each sample is represented in a. d Histologic analysis of the epidermal cysts. Each sample is represented in b. e Histologic analysis of the odontogenic keratinocyte
Based on these results, a common gene mutation was not identified among the simultaneously occurring basal cell carcinomas in the patients with Gorlin syndrome. Furthermore, these mutations were not identified in the skin cysts that occurred concurrently.
Recommended Reading: What Is Nodular And Infiltrating Basal Cell Carcinoma
What Are The Symptoms Of Basal Cell Carcinoma
As the disease progresses, Basal Cell Carcinoma may start showing symptoms. Following are some of the signs and symptoms that may be caused by Basal Cell Carcinoma.
- Scar-like flat, firm, pale or yellow areas
- Itchy raised reddish patches
- Small, pink/red, translucent, shiny, pearly bumps with possibly blue/brown/black areas
- Pink growths with raised edges with abnormal blood vessels spreading out like the spokes of a wheel
- Open sores
Though many of these symptoms may also be caused by various other health conditions, consult your doctor if you experience these symptoms to rule out the possible chances of Basal Cell Carcinoma.