What Are The Risk Factors For Squamous Cell Carcinoma
Risk factors for squamous cell carcinoma include:
- Unprotected exposure to ultraviolet rays
- Light-colored hair, skin, or eyes
- History of skin cancer
- The pathologists report
- Recurrence after treatment
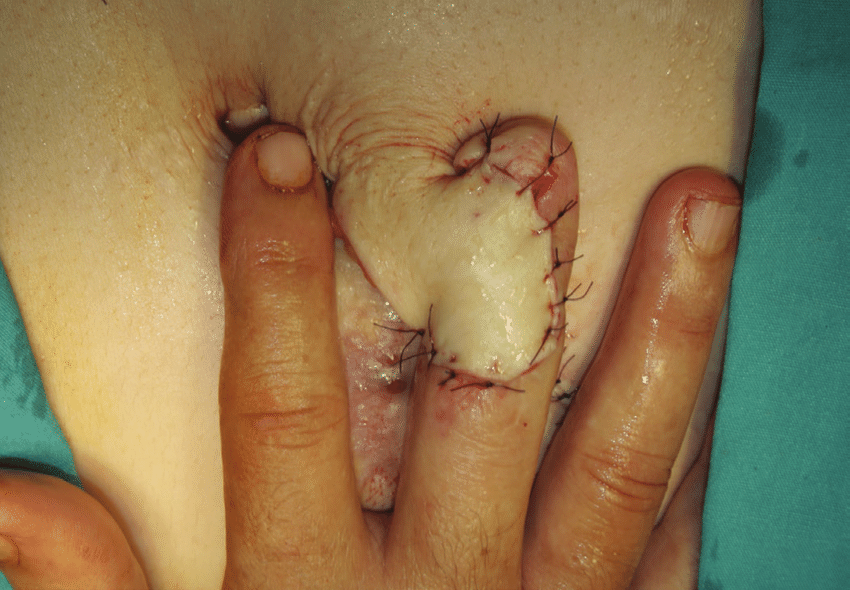
Treatment for squamous cell carcinoma usually involves surgery to remove the lesion. The surgical options include:
- Excision: The physician cuts out the tumor with a scalpel, along with a small margin of healthy skin around the tumor.
- Curettage and electrodesiccation: Used in small lesions, the physician scrapes away cancer cells, then cauterizes the skin to prevent bleeding.
- Mohs surgery: The surgeon removes layers of skin and examines them under a microscope to determine if cancer is present. This process continues until no cancer cells are visible.
Rarely, squamous cell carcinoma is treated with chemotherapy , radiation therapy , and immunotherapy when it has metastasized to other areas of the body.
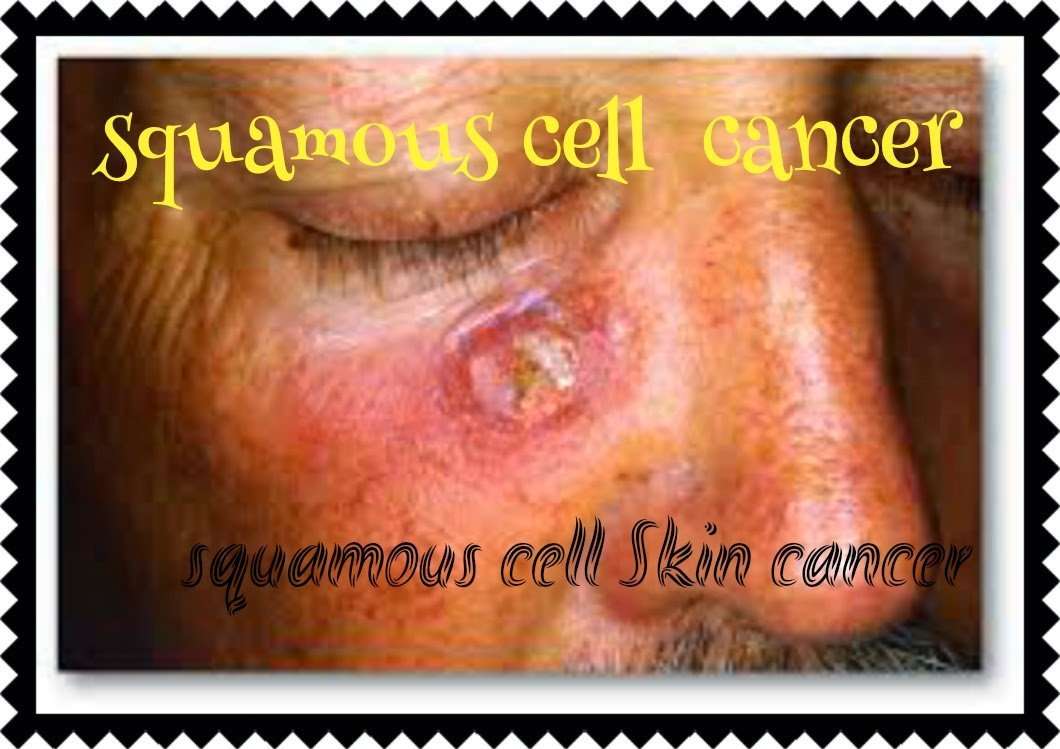
What Does Early Stage Squamous Cell Carcinoma Look Like
Squamous cell carcinoma initially appears as a skin-colored or light red nodule, usually with a rough surface. They often resemble warts and sometimes resemble open bruises with raised, crusty edges. The lesions tend to develop slowly and can grow into a large tumor, sometimes with central ulceration.
What Happens If Squamous Cell Carcinoma Spreads
Untreated squamous cell carcinoma of the skin can destroy nearby healthy tissue, spread to the lymph nodes or other organs, and may be fatal, although this is uncommon. The risk of aggressive squamous cell carcinoma of the skin may be increased in cases where the cancer: Is particularly large or deep.
You May Like: What Does Well Differentiated Mean
Squamous Cell Carcinoma Prevention
Anyone who has had one Squamous Cell Carcinoma has an increased chance of developing another, especially in the same skin area or nearby. That is usually because the skin has already suffered irreversible sun damage.
Thus, it is crucial to pay particular attention to any previously treated site, and any changes noted should be shown immediately to your Doctor at the Bondi Junction Skin Cancer Clinic.
Squamous Cell Carcinomas on the nose, ears, and lips are especially prone to recurrence.
Even if no suspicious signs are noticed, regularly scheduled follow-up visits including total-body skin exams are an essential part of post-treatment care every 6 months.
To prevent Squamous Cell Carcinoma make sure you follow the recommendations below:
What Percentage Of Squamous Cell Skin Cancers Metastasize
Summary. The reported risk for metastasis in squamous cell carcinomas ranges from 0.5% to 16%, a wide spread that can probably be explained by differences in patient populations. Identifying the characteristics associated with a high risk for metastasis would help in determining the need for adjuvant treatment.
Recommended Reading: Well Differentiated Squamous Cell Carcinoma Prognosis
What Are The Causes Of Metastatic Squamous Cell Carcinoma Of Skin
Metastatic Squamous Cell Carcinoma of Skin is caused by the delayed diagnosis and/or appropriate early treatment of squamous cell carcinoma of skin. Some forms of cutaneous squamous cell carcinomas are more aggressive than other forms, and these are more prone to metastasis.
- SCC of skin develops when skin cells are burnt or damaged from prolonged exposure to the ultraviolet component of the sun, over many decades
- The source of UV may be from lamps and other such devices, apart from the sun, and their effect on the skin may cumulatively add-up
- Sometimes, individuals working in certain industries may be exposed to chemicals or x-rays for a long duration. This may also contribute to the formation of the skin cancer
- Scientific research has indicated that the human papillomavirus along with other risk factors, such as sun-exposure, skin color, and an advancing age, seem to greatly multiply the chance of an individual being affected by SCC of Skin. Nevertheless, the reason behind how the virus is responsible for influencing the conditions development is not well-established
What Are The Risk Factors For Metastatic Squamous Cell Carcinoma Of Skin
Metastatic Squamous Cell Carcinoma of Skin is the advanced form of SCC of skin. The chief contributing factors for squamous cell carcinoma of skin include:
- Exposure to intense sun for long periods during the course of work or due to regular participation in outdoor sports activities
- Frequent use of tanning beds, tanning parlors
- People living in geographical regions where hot-dry, desert-like climatic conditions prevail
- Radiation therapy
- Coal tar exposure
- Smoking, tobacco chewing
- Individuals with weak immune system, which could be due to cancer treatment, AIDS, or those on immunosuppressant drugs after receiving an organ transplant
- Those with sensitive skin, who get easily sunburned
- Caucasians are more vulnerable compared to other darker-toned individuals
SCC of skin in certain locations has higher chances of metastasis and they include:
- On the lips
- In the region of radiation scar
- In the region of scar due to burns
- Vulvar skin
- Perianal skin
The following subtypes are the more aggressive forms of SCC of skin, and hence, there is a greater possibility of metastasis:
- Acantholytic squamous cell carcinoma of skin
- Spindle cell squamous cell carcinoma of skin
- Pseudovascular squamous cell carcinoma of skin
- Adenosquamous carcinoma of skin
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
Don’t Miss: Small Blue Cell Tumor Prognosis
Advanced Pathological And Molecular Diagnosis For Identifying Primary Sites
In North America and Western Europe in recent years the majority of oropharyngeal cancers are HPV-related and the incidence of oropharyngeal cancer has increased significantly. The percentage of other anatomic subsites that are HPV related are much smaller and may not carry the same implications of improved prognosis .
The diagnosis of an HPV related tumor may be suspected based on the IHC, the presence of cystic metastases, or the identification of basaloid cytology or histology, and IHC stains, particularly for p16. Once this diagnosis is suspected or proven, it immediately directs the head and neck surgeon toward the oropharynx at the time of either office examination or direct laryngoscopy.
The presence of p16-negative cancer in the node on the other hand, will lead the head and neck surgeon to consider the entire upper aerodigestive tract at risk. The lymphoid tissue of Waldeyers ring, because it is a site of frequent anatomic irregularity, remains a site to be sampled, but the head and neck surgeon will also give extra attention to the larynx , nasal cavity, oral cavity , hypopharynx, and cervical esophagus.
Squamous Cell Carcinoma Diagnosis
Occasionally a punch or shave biopsy may be required to confirm the diagnosis and to guide effective treatment.
This diagnostic process involves a Doctor taking a tissue sample for biopsy by removing a portion of the lesion with a biopsy punch or by scraping the lesion with a curette .Usually a biopsy is sufficient to establish the diagnosis of a Squamous Cell Carcinoma. In the rare case of suspected metastatic Squamous Cell Carcinoma, lymph nodes may be examined by the Doctor to see if the cancer has spread or by the use of imaging technologies like ultrasound, CT, or PET scanning.
You May Like: Osteomyoma
Read Also: How Do Carcinomas Spread
Are You At Risk
The skin is the largest organ of the body. It is also our bodys first line of defense. There are numerous factors which may increase your risk of skin cancer:
- Genetics: Individuals with fair complexions are at the greatest risk. Your risk is also increased if your parents, children, or siblings have had skin cancer.
- Sun Exposure: Over the course of a lifetime, exposure to the sun can lead to a higher risk of skin cancer. Tanning beds and other false sunlight are no exception.
- Immunosuppression: Immunosuppression therapy following organ transplants, chemotherapy, AIDS, and other treatments can put you at a significant risk for skin cancer.
- Lifespan: Human life expectancy has increased from forty-two years in 1904 to close to eighty years today. As a result, the number of skin cancers being seen around the world is increasing.
Read Also: Does Skin Cancer Itch And Burn
The Role Of Fine Needle Aspiration Biopsy Core Biopsy And Open Biopsy
If a primary site is not identified on clinical examination, the next step will be FNA of the neck mass for cytological examination, preferably under ultrasound guidance . For patients with solid masses that harbor squamous cell carcinoma, FNA will be positive in 80% or more and repeated FNA can yield an additional increment. With cystic neck masses the percentage is lower, but still, if ultrasound assisted and directed toward the most solid parts of the lesion, in the majority of patients with a suspicious neck mass, the FNA will correctly diagnose malignancy if present.
In those cases which are not squamous cell carcinomas, and in particular when a primary below the clavicles is suspected, sophisticated diagnostic approaches, including immunocytochemistry or immunohistochemistry and molecular techniques are available to help direct a search for a primary site, based on the biopsy, and this is covered in more detail later.
The possibility of applying additional cytopathological and molecular techniques to the cytologic aspirate, to provide an estimate regarding the risk of malignancy relative to a benign branchial cleft cyst, is an area that is open for further study. If a few non-diagnostic cells are encountered, IHC or in-situ hybridization Epstein Barr Virus , P53 mutations , cytokeratin and other markers can be performed, depending on the viral prevalence in the region and level of suspicion.
Read Also: Idc Breast Cancer Survival Rate
Symptoms Of Basal Cell Carcinoma
There are several types of basal cell carcinomas.
The nodular type of basal cell carcinoma usually begins as small, shiny, firm, almost clear to pink in color, raised growth. After a few months or years, visible dilated blood vessels may appear on the surface, and the center may break open and form a scab. The border of the cancer is sometimes thickened and pearly white. The cancer may alternately bleed and form a scab and heal, leading a person to falsely think that it is a sore rather than a cancer.
Other types of basal cell carcinomas vary greatly in appearance. For example, the superficial type appears as flat thin red or pink patches, and the morpheaform type appears as thicker flesh-colored or light red patches that look somewhat like scars.
You May Like: Invasive Ductal Carcinoma Survival
Metastatic Squamous Cell Carcinoma To The Cervical Lymph Nodes From An Unknown Primary Cancer: Management In The Hpv Era
Background: Patients with metastases in the lymph nodes of the neck and no obvious primary tumor, neck cancer with unknown primary , represent a management challenge. A majority of patients have metastatic squamous cell carcinoma , although other histologies do occur.
Methods: We comprehensively reviewed the literature, compared available guidelines, and conferred with an international team of experts.
Results: Positron emission tomography-computed tomography and fine needle aspiration under ultrasound guidance increase accuracy of diagnosis. Immunohistochemistry , determination of human papilloma virus status, by p16 staining or by in situ hybridization , and next-generation gene sequencing can guide us regarding probable primary sites and tumor biology. Narrow Band Imaging has been introduced for the early detection of subtle mucosal lesions. Direct laryngoscopy and tonsillectomy have long been procedures used in the search for a primary site. More recently, TransOral Robotic Surgery or Transoral LASER Microsurgery have been introduced for lingual tonsillectomy.
Also Check: Merkel Cancer Prognosis
Stages And Grades Of Skin Cancer
The stage of a cancer tells you how big it is and whether it has spread. It helps your doctor decide which treatment you need.
The grade of a cancer tells you how much the cancer cells look like normal cells.
You might have tests to stage your cancer. This depends on your type of skin cancer.
Most basal cell cancers don’t need staging because it’s very rare for them to spread. You only need staging if your cancer is very large.
You are more likely to have staging if you have squamous cell skin cancers . This is because SCCs can spread, although this is still rare.
Doctors can use a numbers system or sometimes the TNM system to stage your cancer.
Can Squamous Cell Carcinoma Be Misdiagnosed
Skin cancer is increasingly misdiagnosed by physicians. In many cases, skin cancer is incorrectly diagnosed as eczema or another less serious disease. Misdiagnoses, failure to diagnose, and delayed diagnosis can all be very dangerous for the patient, as the cancer continues to progress without treatment.
Read Also: How Fast Does Squamous Cell Carcinoma Spread
What Does Stage 4 Squamous Cell Carcinoma Look Like
Symptoms of stage 4 squamous cell carcinoma usually begin with some kind of skin lesion or growth. Often, the tumors of squamous cell carcinoma look like a scaly red patch of skin that won’t heal. These tumors are often crusty and raised, and they may cause sores or ulcers that last for several weeks.
Metastatic Squamous Cell Carcinoma
Squamous cell carcinoma – a very common form of nonmelanoma skin cancer that originates in the squamous cells – becomes metastatic when it spreads beyond the primary cancer site and affects other areas of the body. Metastatic squamous cell carcinoma is uncommon but can develop if the primary cancer is not surgically removed or treated in a timely manner.
You May Like: How Long Does It Take For Melanoma To Spread
Squamous Cell Carcinoma Stages
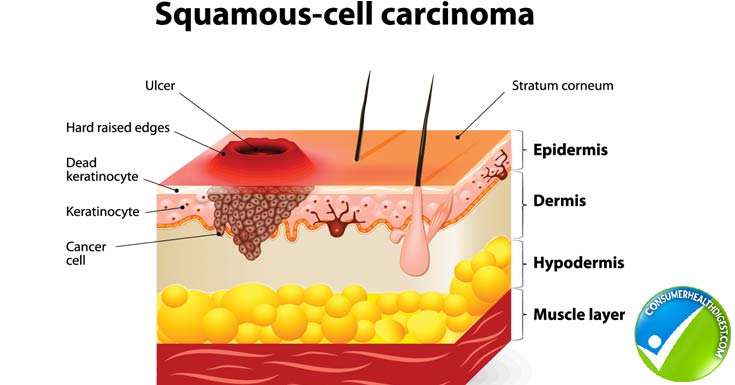
There are certain features that are considered to make the cancer at higher risk for spreading or recurrence, and these may also be used to stage squamous cell carcinomas. These include:
- Greater than 2 mm in thickness
- Invasion into the lower dermis or subcutis layers of the skin
- Invasion into the tiny nerves in the skin
- Location on the ear or on a hair-bearing lip
After the TNM components and risk factors have been established, the cancer is assigned to one of the five squamous cell carcinoma stages, which are labeled 0 to 4. The characteristics and stages of squamous cell cancer are:
Stage 0: Also called carcinoma in situ, cancer discovered in this stage is only present in the epidermis and has not spread deeper to the dermis.
Stage 1 squamous cell carcinoma: The cancer is less than 2 centimeters, about 4/5 of an inch across, has not spread to nearby lymph nodes or organs, and has one or fewer high-risk features.
Stage 2 squamous cell carcinoma: The cancer is larger than 2 centimeters across, and has not spread to nearby organs or lymph nodes, or a tumor of any size with 2 or more high risk features.
Stage 3 squamous cell carcinoma: The cancer has spread into facial bones or 1 nearby lymph node, but not to other organs.
Stage 4 squamous cell carcinoma: The cancer can be any size and has spread to 1 or more lymph nodes which are larger than 3 cm and may have spread to bones or other organs in the body.
What Will Happen After Treatment
Youll be glad when treatment is over. Your doctor will want you to check your skin at least once a month. It will be very important to protect yourself from getting too much sun.
For years after treatment ends, you will see your skin cancer doctor. At first, your visits may be every few months. Then, the longer youre cancer-free, the less often the visits are needed. Be sure to go to all of these follow-up visits. Your doctor will ask about symptoms and check you for signs of the cancer coming back or a new skin cancer. Other exams and tests may also be done.
Having cancer and dealing with treatment can be hard, but it can also be a time to look at your life in new ways. You might be thinking about how to improve your health. Call us at 1-800-227-2345 or talk to your cancer care team to find out what you can do to feel better.
You cant change the fact that you have cancer. What you can change is how you live the rest of your life making healthy choices and feeling as good as you can.
Don’t Miss: Melanoma On Face Prognosis
How Is Cancer Treated In Horses
Treatment of Cancer in Horses
It has been determined that many of the same treatments used in humans for cancer work for horses diagnosed with cancer. This includes surgical removal of the mass, chemotherapy, and radiation. Depending on the location and size of the mass, surgical removal may be an option.
What Are The Signs And Symptoms Of Metastatic Squamous Cell Carcinoma Of Skin
The signs and symptoms of Metastatic Squamous Cell Carcinoma of Skin include:
- There may be a primary skin lesion and secondary metastasized tumors at other locations of the body
- The signs and symptoms of the condition may depend upon the affected organ or body part
- The skin lesions may appear as crusted ulcer, plaques, and nodules
- It may ulcerate and bleed. Occasionally, after the ulcer heals, it may become ulcerated again
- These lesions or tumors are common in sun-exposed areas , but can appear in non-sun exposed areas too
- The size of the lesions are frequently over 2 cm
- In some cases, the squamous cell carcinoma may appear more pigmented than surrounding skin
- Individuals with immunocompromised states have more aggressive tumors
You May Like: Melanoma Forearm
More Information About Basal Cell Carcinoma
The following are some English-language resources that may be useful. Please note that THE MANUAL is not responsible for the content of these resources.
See the following sites for comprehensive information about basal cell carcinoma, including detection, prevention, treatment options, and other resources:
My Appointment With A Plastic Surgeon
Unfortunately, when they started showing up, I had a really terrible health insurance policy so I was unable to get them treated. Once I got better insurance and had built up some vacation time at work so I could be off for recovery, I made an appointment with my plastic surgeon.
As I was showing him the areas, he commented wryly that I must have been saving them up for him. In all, there were 22 areas he determined needed to be removed. He had a printout of a body map and marked each area for removal on the paper, which he would bring with him the day of surgery.
Recommended Reading: Invasive Ductal Carcinoma Survival