How Will I Know Whether Immunotherapy Is Working
You will have regular check-ups with your cancer specialist, blood tests and different types of scans to check whether the cancer has responded to the treatment. It may take some time to know if immunotherapy has worked because people often have a delayed response. In some cases, the cancer may appear to get worse before improving.
You may wonder whether having side effects means the immunotherapy is working. Side effects are a sign that the treatment is affecting your immune system in some way, but this may or may not mean the treatment is affecting the cancer. Many people with mild side effects have still seen improvements.
A good response from immunotherapy will make the cancer shrink or disappear. In some cases, the cancer remains stable, which means it does not grow but also does not shrink or disappear. People with stable disease often continue to have a good quality of life.
Will Immunotherapy Be The End Of Cancer
Immunotherapy has been called a great hopeand a great hype. As a patient facing devastating odds, our writer bet her life on it.
In September of 2011, I did the worst Google search of my life. A year after a seemingly manageable melanoma diagnosis and surgery, I learned that my cancer had appeared again, this time moving aggressively into my lungs and soft tissue. Naturally, the first thing I did was open my laptop and type “stage 4 melanoma life expectancy.” Then I cried. The results were terrifying.
On the website of MD Anderson, one of the most prestigious cancer centers in the world, I found a January 2011 article on metastatic melanoma. There was a telling quote from Michael Davies, MD, of the centers Melanoma Medical Oncology Department: “The average survival for patients with stage 4 metastatic melanoma is 6 to 10 months, and this hasnt changed for 30 years.”
I still get chills when I recall my prognosis not so very long ago, a prognosis that looked likely to wipe my presence from my two young daughters childhoods. Yet a month after my diagnosis, I became one of the first dozen patients in a new clinical trial at the Memorial Sloan Kettering Cancer Center in New York City, receiving a type of treatment known as immunotherapy, which harnesses the bodys natural defenses to fight cancer. Three months later, I was declared cancer-free, and I have been ever since. I had not only been granted a futureI had seen a glimpse of it. Welcome to the next era of medicine.
The Future Of Immunotherapy
Terry’s story shows the powerful effects, as well as the challenges, associated with immunotherapy. It is a relatively new treatment, and we continue to refine it and use it in new ways. Weve seen how it works against melanoma, as well as kidney cancer and lung cancer.
And while immunotoxicities are not what we want, there is some data to suggest that patients who get them are more likely to respond to the treatment. We dont know exactly why, and through clinical trials we are working to prevent side effects while continuing to reap the benefits of immunotherapy.
Clinical trials offer gold standard of care plus the newest available treatments, often at little to no cost to patients. These studies help us advance treatment options for more patients.
If you or a loved one is diagnosed with metastatic melanoma, ask your doctor about immunotherapy. Find an academic medical center that has teams of experts in place not only to manage your care, but also the potential side effects of treatment.
Weve only scratched the surface of what immunotherapy can offer cancer patients. But at UT Southwestern and Simmons Cancer Center we are determined to continue improving it to help more patients like Terry beat this disease and lead longer, healthier lives.
To find out whether you or a loved one might benefit from immunotherapy, call or request an appointment online.
Recommended Reading: Stage 3 Basal Cell Carcinoma Survival Rate
How Long Does Opdivo Take To Work
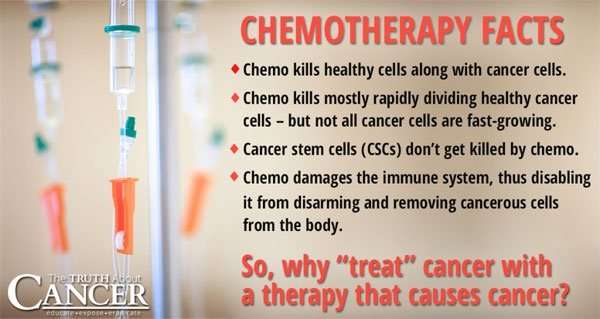
Immunotherapy works differently to traditional chemotherapeutics and can take longer to work because once Opdivo starts helping the immune system to uncover the cancer cells, it takes time for the immune system to identify and attack them.
During clinical trials of Opdivo researchers measure the time to response, which provides a time frame in which youd expect to see a patients cancer show signs that it is responding to treatment and Opdivo is starting to work.
Time to response is the time taken from the day a patient is assigned to receive a particular therapy until the first day that the patient has a partial or complete response to the treatment. The time to response observed in a number of clinical trials used to gain approval of Opdivo are reported in the table below.
Time to response following treatment with Opdivo
| Cancer Type |
How Often Do You Receive Immunotherapy
How often and how long you receive immunotherapy depends on:
- your type of cancer and how advanced it is
- the type of immunotherapy you get
- how your body reacts to treatment
You may have treatment every day, week, or month. Some types of immunotherapy given in cycles. A cycle is a period of treatment followed by a period of rest. The rest period gives your body a chance to recover, respond to immunotherapy, and build new healthy cells.
Read Also: Does Amelanotic Melanoma Blanch When Pressed
Not A Cure But An Extension: How Immunotherapy Works For Advanced Lung Cancer
May 3, 2018
For nearly five decades, doctors have usedvarious forms of immunotherapy to treat certain cancers. These treatmentsstimulate the patients own immune system to attack a disease, much like itwould a virus or another foreign invader. Promising data have emerged toindicate its effectiveness against many cancers, including lung, kidney,melanoma, and some colon cancers.
Most recently, lung cancer has receivedattention for data released from a studypublished in The New England Journal ofMedicine and featured in The New York Times. In the study,the immunotherapy drug pembrolizumab was combined with chemotherapyto determine whether the dual approach was more effective than chemotherapyalone for metastatic nonsquamous non-small cell lung cancer.
The results are encouraging: Patients whoreceived the dual therapy lived longer than those who received onlychemotherapy. In fact, the findings suggest that earlier introduction ofimmunotherapy for certain patients might one day become the standard treatment.
But while the data are promising, we must notbe too eager to declare victory. Todays immunotherapy is not a cure forlate-stage lung cancer. However, it can give certain patients more precioustime with family and friends. To provide that, we must carefully selectpatients who will benefit most and determine the most appropriate availabletreatment. Recent developments havefocused on immune checkpoint inhibitors and on CAR-T cell therapy.
What Do Healthcare Professionals Need To Know When I’m Sick
If you go to urgent care or the emergency room, tell health professionals about your cancer treatment. What type of cancer was diagnosed? When and where were you treated? What type of immunotherapy and other therapies did you receive? Also, ask your primary care doctor to include important information like this in your medical records. Remind health care providers about it if youre sick. You can use health apps to log the information, so youll always have it handy if you need it.
To learn more about immunotherapy or join a clinical trial, talk to your cancer care team. You can also search for clinical trials on the National Cancer Institute website, or call 1-800-422-6237.
Follow me on Twitter @sonpavde
Read Also: Osteomyoma
Does Immunotherapy Have Serious Side Effects
Immunotherapy with PD1/PD-L1 inhibitors is generally well tolerated, but serious side effects may occur. This happens in about 20% of people given PD1/PD-L1-inhibitors. It occurs in 40% to 60% of people given a combination of PD1-inhibitor and CTLA4-inhibitor immunotherapies.
Most side effects appear around two to three months after therapy starts. However, close monitoring, early recognition, and prompt therapy can help control side effects. Because immunotherapy drugs unleash immune cells, inflammation may occur in organs such as the colon , lungs , skin , liver , thyroid gland , and other areas of the body.
Immunotherapy Side Effects: What To Know
If youve researched cancer treatment options, youve probably heard of immunotherapy, which trains the immune system to attack cancer, rather than attacking the cancer directly. You also might have heard that immunotherapy doesnt have side effects.
But thats not always the case. With the most common type of immunotherapy — immune checkpoint therapies — about 5-10% of patients experience side effects, and theyre life-threatening in about 1-2% of those cases, says Vivek Subbiah, M.D. Examples of immune checkpoint drugs include: pembrolizumab , nivolumab , atezolizumab , ipilimumab , avelumab and durvalumab .
Immunotherapy side effects often differ from those commonly seen with other types of cancer treatment. Heres what patients should know.
Fatigue, inflammation top common side effects
As with many cancer therapies, fatigue tends to be one of the most common, says Van Morris, M.D.
But immunotherapy drugs also can cause inflammation throughout the body. For example, patients may experience skin inflammation as pigment changes, a rash and feeling itchy, sometimes even without a rash. Inflammation in the lungs can cause a cough and chest pains. The colon may also become inflamed, causing abdominal pain and diarrhea.
Side effects often show up early in treatment or months or years later
Side effect management depends on the severity
Patients who develop diabetes may require insulin or a period of time off the immunotherapy.
Watch for changes in your body
Read Also: Does Amelanotic Melanoma Blanch When Pressed
Stop Tumors In Their Tracks
Every melanoma has the potential to become deadly, but the difference between an in situ melanoma and one that has begun to metastasize cannot be overstated. There is a drastic change in the survival rate for the various stages of tumors, highlighting the importance of detecting and treating melanomas before they have a chance to progress. Its impossible to predict exactly how fast a melanoma will move from stage to stage, so you should be taking action as soon as possible.
To be sure youre spotting any potential skin cancers early, The Skin Cancer Foundation recommends monthly skin checks, and scheduling an annual total-body skin-exam with a dermatologist. These skin exams can help you take note of any new or changing lesions that have the potential to be cancerous, and have them biopsied and taken care of before they can escalate.
Trust your instincts and dont take no for an answer, Leland says. Insist that a doctor biopsy anything you believe is suspicious.
How Long Does Immunotherapy Last
Cancer cells adapt, building resistance to targeted therapies. When a tumor responds to immunotherapy, the remission tends to last a long time , unlike a response to chemotherapy . Also, with immunotherapy, tumors initially may swell as immune cells engage with the cancer cells, then later shrink as cancer cells die. The early swelling is called psuedoprogression.
You May Like: Etiology Of Basal Cell Carcinoma
Which Cancers Are Treated With Immunotherapy
Immunotherapy drugs have been approved to treat many types of cancer. However, immunotherapy is not yet as widely used as surgery, chemotherapy, or radiation therapy. To learn about whether immunotherapy may be used to treat your cancer, see the PDQ® adult cancer treatment summaries and childhood cancer treatment summaries.
What If Immunotherapy Doesnt Work
Unfortunately, checkpoint inhibitors do not work for everyone. Some cancers will not respond to the treatment at all, or the cancer cells can become resistant to the treatment even if it works at first.
This can be very disappointing, but your cancer specialist will help you explore other treatment options if this happens.
You May Like: Soderstrom Skin Cancer Screening
Monoclonal Antibodies Monoclonal Antibodies Are Made In The Lab Like The Antibodies That Your Immune System Makes Their Job Is To Trigger An Immune System Reaction Some Monoclonal Antibodies Work By Finding A Specific Antigen On A Cancer Cell And Then Attaching To It The Immune System Then Knows To Attack And Destroy Those Cells One Example Of This Type Of Monoclonal Antibody Is Rituximab Rituximab Is Used To Treat Some Types Of Non
Immune checkpoint inhibitors
The immune system normally stops T cells from attacking normal cells in the body by using proteins called checkpoints. Checkpoints are part of a pathway that the immune system uses to slow down or put the brakes on an immune system response. Some cancer cells can send signals that confuse T cells by turning on a checkpoint pathway and stopping them from attacking cancer cells. This lets the cancer continue to grow because the cancer cells hide from the immune system.
Immune checkpoint inhibitors are monoclonal antibodies that work by blocking checkpoint proteins so that immune system cells can attack and kill the cancer cells. They are used to treat melanoma skin cancer, nonsmall cell lung cancer, kidney cancer and Hodgkin lymphoma.
There are 2 immune checkpoint pathways that can be blocked to allow the immune system to fight cancer. PD-1 is an immune checkpoint that stops T cells from attacking other cells in the body. It does this by attaching to PD-L1, a protein found on some normal and cancer cells. Some cancer cells have a lot of PD-L1, which helps protect them from being attacked by T cells. Monoclonal antibodies such as atezolizumab , pembrolizumab and nivolumab target PD-1 or PD-L1 to help boost the immune systems response to attack cancer cells and destroy them.
CTLA-4 is another immune checkpoint on T cells that the monoclonal antibody ipilimumab can target. This helps boost the immune systems response against cancer cells.
How Is Immunotherapy Given
Checkpoint inhibitors are usually prescribed by a medical oncologist or haematologist. They are given as a liquid through a drip inserted into a vein . Sometimes two or more drugs may be given together, such as two checkpoint inhibitors, or a checkpoint inhibitor with one or two chemotherapy drugs or a targeted therapy drug.
You will usually have immunotherapy as an outpatient, which means you visit the hospital or treatment centre for the infusion and then go home again. Checkpoint inhibitors are commonly given in repeating cycles, with rest periods of 26 weeks in between.
How often and how long you have the treatment depends on:
- the type of cancer and how advanced it is
- the type of checkpoint inhibitor
- how the cancer responds to the treatment
- what side effects you experience.
Many people stay on immunotherapy for up to two years. Clinical trials are now testing if the treatment can be given for a shorter period of time once it has started working or whether ongoing treatment is needed.
Checkpoint inhibitors can take weeks or months to start working, depending on how your immune system and the cancer respond. Sometimes they keep working long after treatment stops, but this varies from person to person.
Like many other cancer treatments, immunotherapy drugs are often not safe to use if you are pregnant or breastfeeding. Ask your doctor for advice about contraception. If you become pregnant, let your medical team know immediately.
Don’t Miss: Squamous Cell Carcinoma Skin Metastasis
Which Lung Cancer Patients Canbenefit
A small number of patients have a very high levelof PD-L1, a biomarker that indicates a tumor is especiallysusceptible to immunotherapy drugs. Non-small cell lung cancer accounts for 85percent of cases. Of those, about 25 percent have a high enough PD-L1 level bytodays standards to benefit from the initial use of immunotherapy as opposedto chemotherapy alone.
How PD-L1 levels will be used to plantreatment is not fully clear. Immunotherapy drugs might work in patients evenif the PD-L1 level is very low. Also, adding pembrolizumab tochemotherapy appears to offer benefit regardless of tumor PD-L1 level.
To consider giving immunotherapy alone as theinitial treatment of lung cancer, we must perform tissue testing of PD-L1levels. For lung cancer, this may present several complexities, which canresult in additional time between testing and treatment:
The ability to biopsy the tumorand assess PD-L1 levels is dependent upon the location of the cancer.
Some patients dont have enoughtissue to test for PD-L1.
The test might not have beenordered before the patient saw the oncologist, which would result in asubsequent visit.
The biopsy was performed at adifferent medical center and would need to be redone to ensure the care team ison the same page.
Is Immunotherapy Right For Me
These drugs donât work for everyone with melanoma. Scientists are hard at work to figure out why and pinpoint the differences between patients who respond and those who donât.
One reason why they may work better for some people than others: Doctors think tumors that have the most DNA damage are more likely to respond to these drugs. This makes sense: The mutant molecules stick out on the surface of the tumor cell, making it easier for the immune system to recognize them as foreign.
This means the drugs may work best with melanomas caused by too much DNA-damaging UV radiation. These findings could lead to diagnostic tests that identify which patients are most likely to benefit from these therapies.
Then again, there isnât a direct cause and effect at play. Generally, the more mutations you have, the better your response will be. But not always. Some people donât have a lot of genetic mutations but respond well. Scientists believe that other — and as yet undiscovered — checkpoints may be the cause.
Or your immune system may need a little more help spotting cancer cells so it can destroy them. Pairing these immune-based anti-cancer drugs, like a mix of ipilimumab and pembrolizumab, might work better. Studies showed a good response rate, and doctors got the FDAâs OK to use the combo in 2015.
American Cancer Society: âImmune checkpoint inhibitors to treat cancer,â âIf You Have Melanoma Skin Cancer,â âImmunotherapy for melanoma skin cancer.â
Recommended Reading: Does Skin Cancer Itch And Burn