Immunotherapy For Metastatic Melanoma
Immunotherapy is now considered a promising new approach for the treatment of metastatic melanoma , even if its role is a relatively late discovery for this malignancy. One of the main characteristics of immunotherapy is the resistance to radiation therapy and cytotoxic chemotherapy. In the past, the key drug for melanoma was Dacarbazine, with an overall response rate of 10-20% however, there were no differences between Dacarbazine monotherapy and a combined chemotherapy. No better results have been reported for radiotherapy. Despite the poor clinical results, these approaches have been the main drivers in melanoma treatment for decades .
An Exception: Autoimmune Disorders
If you have an autoimmune disorder, you may be unable to tolerate immunotherapy even if you would otherwise qualify for treatment. With an autoimmune disease, such as lupus, rheumatoid arthritis, Crohns disease or ulcerative colitis, your immune system mistakenly attacks healthy cells. Autoimmune diseases are treated with drugs that suppress the immune system. Immunotherapy, on the other hand, revs up the immune system and stimulates T-cells. So, immunotherapy may cause your autoimmune disease to flare up, or it may produce other toxic side effects. A potent immune response may even cause your T-cells to start attacking your organs.
Symptoms of an autoimmune response to immunotherapy may include diarrhea, inflammation of the liver, a skin rash or inflammation of the lung. Sometimes, we may be able to successfully treat the flare-up and continue immunotherapy. For example, if you develop symptoms of hypothyroidism, but you respond to treatment for the condition, we may be able to continue immunotherapy.
A new clinical trial, sponsored by the National Cancer Institute , is testing the use of an immunotherapy drug on cancer patients who have a preexisting autoimmune disease when the risks of cancer outweigh the potential harms of an autoimmune response. So, while having a known autoimmune disease may disqualify you from receiving immunotherapy, advances in treatment research may eventually change that.
Neoantigen Expression Improves B16 Tumor Recognition By Pmel
Melanoma has been a source of intensive study in cancer immunology for many years because it often gives rise to endogenous T cells with antitumor activity . The mechanisms underlying melanomas susceptibility to immune-based therapies are due in part to the demonstrable fact that melanomas express large numbers of neoantigens and tumor-infiltrating lymphocytes that are reactive to their unique mutations . T cells recognize antigens when they are presented on an MHC molecule. B16, a mouse melanoma line, is commonly used to model human melanoma and cancer immunotherapy. B16 is poorly immunogenic and expresses low levels of MHC-I. Furthermore, the mouse autoantigen gp100EGS has a low affinity to the class I MHC restriction element H-2Db.
We sought to examine whether B16 tumors expressing a neoantigen were more immunogenic and better recognized by pmel-1 T cells. We previously found that when the autoantigen gp100EGS and neoantigen gp100KVP peptides were exogenously pulsed onto EL-4 cells, pmel-1 cells recognized gp100KVP a thousandfold better than the gp100EGS epitope . We thus constructed a control vector encoding the full-length WT mouse gp100 and a vector encoding the full-length mouse gp100 but with amino acids at positions 2527 changed from EGS to KVP .
Modified B16 cell lines and their recognition by pmel-1 T cells.
Read Also: Stage 5 Cancer Symptoms
Keytruda Active Against Brain Metastases
Brain metastases are a common cause of disabling neurologic complications and death in patients with metastatic melanoma and occur in up to 40% of patients. A recently reported clinical study in 23 patients with melanoma and one or more asymptomatic, untreated 5- to 20-mm brain metastases treated with Keytruda monotherapy found that 26% of the patients treated with Keytruda responded for an average of 24 months.
Cancer in the brain and the rest of the body responded in a similar manner suggesting the brain metastases were of similar biology to the rest of the cancer. The average overall survival was 17 months and ~ 50% of the patients survived 2 years or longer.
Doctors are now evaluating the use of dual immunotherapy as treatment for metastatic melanoma that has spread to the brain. Patients with brain metastases should discuss these options with their treating physician and explore newer combinations of immunotherapy being evaluated in clinical trials.4
Treating Stage 4 Melanoma
If melanoma comes back or spreads to other organs it’s called stage 4 melanoma.
In the past, cure from stage 4 melanoma was very rare but new treatments, such as immunotherapy and targeted treatments, show encouraging results.
Treatment for stage 4 melanoma is given in the hope that it can slow the cancer’s growth, reduce symptoms, and extend life expectancy.
You may be offered surgery to remove other melanomas that have grown away from the original site. You may also be able to have other treatments to help with your symptoms, such as radiotherapy and medicine.
If you have advanced melanoma, you may decide not to have treatment if it’s unlikely to significantly extend your life expectancy, or if you do not have symptoms that cause pain or discomfort.
It’s entirely your decision and your treatment team will respect it. If you decide not to receive treatment, pain relief and nursing care will be made available when you need it. This is called palliative care.
Read Also: Does Amelanotic Melanoma Blanch When Pressed
Keytruda Treament Of Stage Ii Melanoma
The Phase 3 KEYNOTE-716 clinical trial evaluated Keytruda treatment in 954 patients with stage IIB and IIC melanoma that had been surgically resected. Following surgery half of the patients received Keytruda and half did not. At the interim analysis it was determined that Keytruda treatment improved the duration of remission without cancer recurrence. Fewer patients treated with Keytruda experienced recurrence and at 12 months 90.5% of Keytruda treated patients survived cancer free compared to only 83% of those not treated with Keytruda.
Using Digital Technology To Track And Report Symptoms Improves Patients Quality Of Life
Who does this study affect: People receiving active treatment for metastatic cancer.
What did this study find: Researchers from the PRO-TECT clinical trial found that having patients fill out online surveys about their symptoms during cancer treatment helped their health care teams find and treat symptoms earlier and improved the patients quality of life.
This study was conducted across 52 cancer clinics in the United States and included 1,191 people with metastatic cancer who were receiving systemic treatment with medications. The median age of the participants was 63 years, and more than half were women. Most of the people in this study were white , and 17% were Black. About 1 of every 4 people in this study lived in a rural location, and nearly 4 in 10 reported high school as their highest level of education. There were 201 participants who had never used the internet before.
If the survey results indicated that someones symptoms were severe or worsening, they were emailed information about how to manage their symptoms at home. In addition, an email alert was sent to nurses at their treatment centers. The nurses were then able to reach out to the patients and help them manage their symptoms and get additional care, if necessary. The patients oncologist also received a report with data about their symptoms.
You May Like: Treatment For Stage 3 Melanoma
Immunotherapy For Melanoma Skin Cancer
Some people with melanoma skin cancer have immunotherapy. Immunotherapy helps to strengthen or restore the immune systems ability to fight cancer. Immunotherapy is sometimes called biological therapy or targeted therapy depending on how it works.
You may have immunotherapy to:
- lower the risk that the cancer will come back
- stop or control the growth and spread of cancer cells
- shrink metastatic melanoma skin cancer
Your healthcare team will consider your personal needs to plan the drugs, doses and schedules of immunotherapy. You will probably receive other treatments.
No New Safety Concerns
Brain metastases can hinder brain function by destroying healthy brain cells and by causing swelling in the brain. Because immunotherapies can cause inflammation, there were concerns that these treatments might trigger brain swelling and more neurological issues, Dr. Tawbi explained.
However, only seven participants had a serious neurological side effect, such as swelling or bleeding in the brain. In total, 55% of participants had a serious adverse event related to the treatment, most commonly an immune response in the liver . One participant died from inflammation of the heart muscles , which was related to the treatment.
The safety profile in this population was consistent with that reported in studies involving patients without brain metastases, noted Drs. Turajlic and Larkin.
It appears theres no increased safety risk in patients with melanoma brain metastases, said Dr. Sharon. I think that was the most interesting finding.
Don’t Miss: Invasive Ductal Carcinoma Grade 1 Survival Rate
Targeting Neoantigen With Act Increases B16 Tumor Regression
We sought to elucidate whether enhanced T cell recognition in our model using the gp100KVP neoantigen translated to increased tumor regression in vivo. Having observed significant recognition of B16KVP tumors by pmel-1 cells, we examined the efficacy of neoantigen-targeted ACT therapy involving lymphodepletion , recombinant vaccination, and IL-2 administration to treat tumor-bearing mice .
Mechanisms Of Response And Nonresponse To Pd
Approximately 50% of all patients with advanced melanoma presenting for treatment will demonstrate primary or acquired resistance to antiPD-1based therapies . At the time of presentation, melanoma metastases have coevolved with the antimelanoma immune response for long periods, possibly many years. The immune response to tumor is shaped by the tumor but also by host genetic factors and environmental factors such as prior pathogen exposures and the microbiome. The immune response itself is complex and involves the interaction of many types of immune cells, many molecular interactions between the cells, and includes stimulatory and inhibitory signals and actions. It is within this complex and heterogenous hosttumor immune relationship that physicians apply relatively narrow therapeutic interventions in the hope of altering the threshold for productive antitumor immune reaction. Given the relatively limited access to human tissue at baseline and after an intervention, and the technological limitations in measuring the many variables simultaneously, critical mechanisms for response and nonresponse are difficult to define, particularly for individual patients.
You May Like: What Is Large Cell Carcinoma
Who Is A Good Candidate For Immunotherapy
Whether you may be a candidate for immunotherapy depends on the specific type and stage of your cancer, biomarkers that your cancer expresses, and whether current cancer treatment guidelines and data support immunotherapy for certain situations.
You may be a candidate for immunotherapy if:
- Genomic testing reveals biomarkers that are positive for PD-L1 expression, high microsatellite instability or high tumor mutational burden.
- You have advanced cancer. Generally, if youve exhausted your options for conventional treatment, you may be accepted into a clinical trial studying the effectiveness of an immunotherapy drug on your cancer type or on the genetic markers identified in its DNA.
- You have non-small cell lung cancer, especially if its metastatic or at an advanced stage. Genomic testing is now part of the guidelines for this type of cancer. Studies show that patients with advanced non-small cell lung cancer who respond to immunotherapy are living longer than those who didnt get access to immunotherapy. Some have been on maintenance doses for a long period of time.
Immunotherapy may be used in some cases to reduce the risk of relapse in those who have had a cure of their non metastatic cancer. This is more common in lung cancer and in some melanomas.
Depending on the type of cancer, immunotherapy may also be used in conjunction with chemotherapy.
Sentinel Lymph Node Biopsy
A sentinel lymph node biopsy is a procedure to test for the spread of cancer.
It may be offered to people with stage 1B to 2C melanoma. It’s done at the same time as surgical excision.
You’ll decide with your doctor whether to have a sentinel lymph node biopsy.
If you decide to have the procedure and the results show no spread to nearby lymph nodes, it’s unlikely you’ll have further problems with this melanoma.
If the results confirm melanoma has spread to nearby nodes, your specialist will discuss with you whether further surgery is required.
Additional surgery involves removing the remaining nodes, which is known as a lymph node dissection or completion lymphadenectomy.
Read Also: What Is The Survival Rate For Invasive Ductal Carcinoma
Treating Stage 1 To 2 Melanoma
Treating stage 1 melanoma involves surgery to remove the melanoma and a small area of skin around it. This is known as surgical excision.
Surgical excision is usually done using local anaesthetic, which means you’ll be awake, but the area around the melanoma will be numbed, so you will not feel pain. In some cases, general anaesthetic is used, which means you’ll be unconscious during the procedure.
If a surgical excision is likely to leave a significant scar, it may be done in combination with a skin graft. However, skin flaps are now more commonly used because the scars are usually less noticeable than those resulting from a skin graft.
Read more about flap surgery.
In most cases, once the melanoma has been removed there’s little possibility of it returning and no further treatment should be needed. Most people are monitored for 1 to 5 years and are then discharged with no further problems.
Challenges In Targeting Ctla
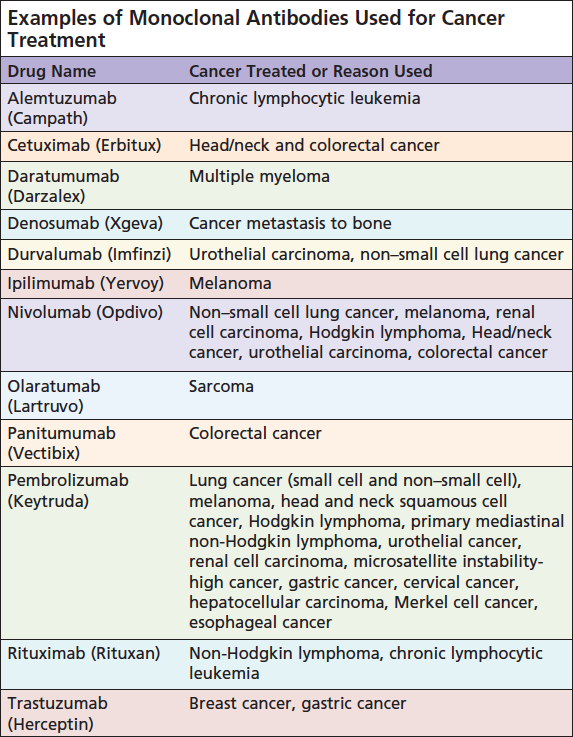
The Allison laboratory reported in 1996 that antibody targeting CTLA-4 induced rejection of established tumors in the mice . These observations inspired Medarex Inc to generate anti-human CTLA-4 antibody for treatment of melanoma. After a decade-long clinical testing, the anti-CTLA-4 antibody Ipilimumab was shown to improve survival of melanoma patients in a large phase III clinical trial . This antibody has taken a historical significance as it is the first T-cell targeting antibody that activates host immunity against cancer. Another longstanding effort to develop a different anti-CTLA-4 antibody, the Tremelimumab by Pfizer, Inc and AstraZeneca Inc, however, has not reached statistical endpoint in phase III trials . Therefore, clinical performance of CTLA-4 targeting is mainly based on a single antibody. In contrast, PD-1/PD-L1 targeting has been validated by a large cohort of clinical products in multiple cancers.
Read Also: What Is The Most Aggressive Skin Cancer
Immunotherapy Combinations For Treating Metastatic Melanoma And Using Technology To Find And Treat Symptoms Early: The Asco Plenary Series
The pace of progress in cancer research keeps getting faster and faster. However, the results of this research can take time to reach the medical community. The ASCO Plenary Series is a new program developed by the American Society of Clinical Oncology to help speed the delivery of high-impact cancer research. In this new series, cancer care providers will now gather online to learn about new, carefully selected research and discuss the study results with their colleagues.
Follow the discussion about research from the ASCO Plenary Series by using the #ASCOPlenarySeries hashtag on Twitter.
How Does Immunotherapy Work Against Cancer
As part of its normal function, the immune system detects and destroys abnormal cells and most likely prevents or curbs the growth of many cancers. For instance, immune cells are sometimes found in and around tumors. These cells, called tumor-infiltrating lymphocytes or TILs, are a sign that the immune system is responding to the tumor. People whose tumors contain TILs often do better than people whose tumors dont contain them.
Even though the immune system can prevent or slow cancer growth, cancer cells have ways to avoid destruction by the immune system. For example, cancer cells may:
- Have genetic changes that make them less visible to the immune system.
- Have proteins on their surface that turn off immune cells.
- Change the normal cells around the tumor so they interfere with how the immune system responds to the cancer cells.
Immunotherapy helps the immune system to better act against cancer.
Recommended Reading: Ductal Breast Cancer Survival Rates
What Is Immunotherapy
The immune system protects the body against illness and infection. Immunotherapies are treatments that use the immune system to recognise and kill cancer cells.
Your doctor may suggest having immunotherapy after surgery. They will only suggest it if the surgeon was able to remove the melanoma, and if the melanoma has only spread to the nearby area or lymph nodes.
This is to help reduce the risk of the melanoma coming back. This is called adjuvant treatment.
If the melanoma cannot be removed, your doctor may suggest immunotherapy treatment to help slow the growth and help you live longer.
There are different types of immunotherapy that work in different ways. They are sometimes known as checkpoint inhibitors. The main drugs used are:
- Ipilimumab
What Are The Risks
Immunotherapy holds a lot of promise as a cancer treatment. Still, it can cause some problems.
You might have a bad reaction. The area where the medication goes into your body could hurt, itch, swell, turn red, or get sore.
There are side effects. Some types of immunotherapy rev up your immune system and make you feel like you have the flu, complete with fever, chills, and fatigue. Others could cause problems like swelling, weight gain from extra fluids, heart palpitations, a stuffy head, and diarrhea. Most of the time, these ease up after your first treatment.
It can harm organs and systems. Some of these drugs can cause your immune system to attack organs like your heart, liver, lungs, kidneys, or intestines.
It isnât a quick fix. In some cases, immunotherapy takes longer to work than other treatments. Your cancer may not go away quickly.
It doesnât work for everyone. Right now, immunotherapy works for less than half the people who try it. Many people only have a partial response. This means your tumor could stop growing or get smaller, but it doesnât go away. Doctors arenât sure yet why immunotherapy helps only some people.
Your body could get used to it. Over time, immunotherapy may stop having an effect on your cancer cells. This means that even if it works at first, your tumor could start to grow again.
You May Like: What Is Braf Testing In Melanoma