What Do Squamous Cell Carcinomas Look Like
Squamous cell carcinomas often appear as a raised, crusty, non-healing sore.
They may also appear as a:
- flat sore with or without a scaly crust
- new sore or raised area on an existing scar or ulcer
- rough, scaly patch on your lip that may evolve to an open sore
- red sore or rough patch inside your mouth
- red, raised patch or wart-like sore on or in your anus or on your genitals.
Help Getting Through Cancer Treatment
People with cancer need support and information, no matter what stage of illness they may be in. Knowing all of your options and finding the resources you need will help you make informed decisions about your care.
Whether you are thinking about treatment, getting treatment, or not being treated at all, you can still get supportive care to help with pain or other symptoms. Communicating with your cancer care team is important so you understand your diagnosis, what treatment is recommended, and ways to maintain or improve your quality of life.
Different types of programs and support services may be helpful, and can be an important part of your care. These might include nursing or social work services, financial aid, nutritional advice, rehab, or spiritual help.
The American Cancer Society also has programs and services including rides to treatment, lodging, and more to help you get through treatment. Call our National Cancer Information Center at 1-800-227-2345 and speak with one of our trained specialists.
Symptoms And Signs Of Oral Squamous Cell Carcinoma
Oral lesions are asymptomatic initially, highlighting the need for oral screening. Most dental professionals carefully examine the oral cavity and oropharynx during routine care and may do a brush biopsy of abnormal areas. The lesions may appear as areas of erythroplakia or leukoplakia and may be exophytic or ulcerated. Cancers are often indurated and firm with a rolled border. As the lesions increase in size, pain, dysarthria, and dysphagia may result.
This photo shows a close-up of the inside of the mouth in a patient with squamous cell carcinoma of the oral mucosa.
CLINICA CLAROS/SCIENCE PHOTO LIBRARY
Erythroplakia is a general term for red, flat, or eroded velvety lesions that develop in the mouth. In this image, an exophytic squamous cell carcinoma on the tongue is surrounded by a margin of erythroplakia.
Image provided by Jonathan A. Ship, DMD.
Leukoplakia is a general term for white hyperkeratotic plaques that develop in the mouth. About 80% are benign. However, in this image, squamous cell carcinoma is present in one of the leukoplakic lesions on the ventral surface of the tongue .
Image provided by Jonathan A. Ship, DMD.
Don’t Miss: What Is The Survival Rate For Invasive Ductal Carcinoma
How Is Squamous Cell Carcinoma Treated
Although squamous cell carcinomas usually grow slowly, it is important to see a dermatologist quickly. “The sooner you see your doctor and the cancer is diagnosed and treated, the less complicated the surgery to remove it will be, and the faster you will make a complete recovery, Dr. Leffell explains. The treatment for squamous cell cancer varies according to the size and location of the lesion. The surgical options are the same as those for basal cell cancer:
- Surgical excision: Removing a squamous cell lesion is a simple procedure that typically takes place in the dermatologist’s office. After numbing the cancer and the area around it with a local anesthetic, the doctor uses a scalpel to remove the tumor and some of the surrounding skin to make sure all cancer is eliminated. Estimating how much to take requires skill and expertise, Dr. Leffell notes. The risk of taking too little tissue is that some cancer remains taking too much leaves a larger scar than is necessary. Shaped like a football, the wound is stitched together, using plastic surgery techniques. If dissolvable stitches are used, they will disappear on their own as the area heals. Though the procedure leaves some redness and a small scar, it tends to become less noticeable over time. “The cure rate for this type of excision is typically about 90 to 93 percent,” says Dr. Leffell. But, of course, this is dependent on the skill and experience of the doctor.”
Genomic Alterations And Key Pathways

There is a tremendous need to identify molecular biomarkers that can be used to predict progression of premalignant HNSCC lesions, prognosticate survival, reveal new targets for intervention and predict response to therapeutic agents. The search for biomarkers has focused on defining the molecular abnormalities that characterize HNSCC. In this section, we highlight findings regarding genetic and epigenetic alterations, as well as dysregulation of cellular signalling pathways, which occur during HNSCC development.
Two additional members of the TP53 gene family, TP63 and TP73, are frequently altered in HNSCC. TP63 encodes two major isoforms, Np63 and TAp63 domain, respectively), and is overexpressed in a majority of HNSCC tumours. Np63 promotes HNSCC tumour growth by multiple mechanisms, including suppression of apoptosis and p16INK4A expression and induction of mitogenic signalling. By contrast, TAp73, a major isoform encoded by TP73, exhibits tumour suppressor activity and the function of TAp73 is commonly abrogated in HNSCC. For example, stimulation of HNSCC cells with TNF results in the induction of c-REL oncoprotein that binds to Np63, displacing TAp73 from Np63TAp73 complexes and inactivating TAp73,. Phosphorylation of Tap73 by casein kinase 2 or Polo-like kinase 2 also leads to TAp73 inactivation and results in induction of NANOG, SOX2 and OCT4, promoting the stem cell-like properties of HNSCC tumour cells,.
You May Like: Lobular Breast Cancer Stage 3
What Survival Rates Mean
The survival rate is the percentage of people who live for a certain period of time with this cancer. The number is based on research done on large groups of people with the same stage of cancer.
Experts dont know the exact survival numbers for late-stage SCC, because cancer registries dont track statistics for this cancer. However, your doctor may be able to give you an estimate of your prognosis.
When it comes to surviving cancer, everyone is different. Your outcome will depend on the specific treatments you have and how well you respond to them. Talk to your doctor about your outlook and what it means.
Diagnosing Squamous Cell Carcinoma
The main way to diagnose squamous cell carcinoma is with a biopsy. This involves having a small piece of tissue removed from the suspicious area and examined in a laboratory.
In the laboratory, a pathologist will examine the tissue under a microscope to determine if it is a skin cancer. He or she will also stage the cancer by the number of abnormal cells, their thickness, and the depth of penetration into the skin. The higher the stage of the tumor, the greater the chance it could spread to other parts of the body.
Squamous cell carcinoma on sun-exposed areas of skin usually does not spread. However, squamous cell carcinoma of the lip, vulva, and penis are more likely to spread. Contact your doctor about any sore in these areas that does not go away after several weeks.
You May Like: What Is Large Cell Carcinoma
Factors Affecting Squamous Cell Carcinoma Prognosis
There are a handful of factors that can affect a patients prognosis, including:
- Having a weakened immune system
- The location of the tumortumors found on the face, scalp, fingers and toes spread more easily, as do tumors that arise in an open wound
- If the cancer has recurred
- Larger tumors and those that are growing deep in the skin
Altered Radiation Fractionation Schedules
Conventional radiotherapy consists of one daily treatment Monday to Friday for three to seven weeks, varying between centres in the United Kingdom. Total doses vary from 50 Gy to 70 Gy. In the United States and Europe 60 Gy to 70 Gy are standard. These schedules are assumed to have the same overall radiobiological effect, which depends on the relation between overall time, total dose, and the number of fractions. They developed through clinical experience and training, however, randomised controlled trials have never been used to compare these different conventional fractionation schedules.
In the 1980s focus centred on time-fractionation schedules low doses per fraction could give reduced late morbidity. This led to trials of hyperfractionation in which the dose per fraction was smallthat is, divided up into two or three treatments per day instead of one. With increasing overall treatment time the total dose had to be increased to achieve the same effect. Accelerated regimens with shortened overall duration were therefore investigated, with the aim of reducing the time in which tumour cell repopulation could occur. These regimens have been studied by groups at Mount Vernon, United Kingdom, the Danish head and neck cancer group, radiation therapy, and oncology group in the United States, the European Organization for Research and Treatment of Cancer, and others with improvements in disease specific survival and locoregional control .
You May Like: How Fast Does Cancer Spread Without Treatment
New Treatments For Squamous Cell Cancer
For early and limited Squamous Cell Cancer, Aldara cream can be used to eliminate the cancer. This saves patients from surgery and leads to an excellent cosmetic result. For more information about Aldara nonsurgical treatments, please inquire about this at your next appointment.
For more information on Squamous Cell Carcinoma or to set up a consultation, click here. Thank you and we look forward to helping you.
Factors That Could Affect Your Prognosis
Certain aspects of your health or cancer could affect your outlook. For example, people who have a weakened immune system from a disease like HIV or a medication they take tend to have a less positive outlook.
The location of the tumor also matters. Cancers on the face, scalp, fingers, and toes are more likely to spread and return than those on other parts of the body. SCC that starts in an open wound is also more likely to spread.
Larger tumors or ones that have grown deep in the skin have a higher risk of growing or returning. If a cancer does recur after treatment, the prognosis is less positive than it was the first time around.
Ask your doctor if you have any risk factors that can be managed or controlled. You may need more aggressive treatment, or to be monitored more closely for recurrence.
You May Like: Prognosis Of Skin Cancer
Organ Preservation In Operable Disease
In two large studies, chemotherapy and then radiotherapy for responding patients or surgery for non-responding patients gaves equal results for locoregional control compared with immediate surgery and then radiotherapy. Survival rates did not differ between the two groups, but this approach allowed a number of patients to retain their larynx.,
These results have led to a trend towards preserving organs by giving chemotherapy during radiotherapy in advanced disease. Mostly, these strategies have scheduled chemoradiotherapy to the primary and neck, followed by a neck dissection six weeks later provided there is a complete response of the primary tumour. An alternative for an inoperable primary tumour or potentially functionally debilitating surgery is neck surgery followed by chemoirradiation to the primary. A prime example of this is in advanced tongue base tumours, where surgical management would involve a total glossolaryngectomy.
Squamous Cell Carcinoma Risk Factors
Certain things make you more likely to develop SCC:
- Older age
- Blue, green, or gray eyes
- Blonde or red hair
- Spend time outside, exposed to the sun’s UV Rays
- History of sunburns, precancerous spots on your skin, or skin cancer
- Tanning beds and bulbs
- Long-term exposure to chemicals such as arsenic in the water
- Bowens disease, HPV, HIV, or AIDS
Your doctor may refer you to a dermatologist who specializes in skin conditions. They will:
- Ask about your medical history
- Ask about your history of severe sunburns or indoor tanning
- Ask if you have any pain or other symptoms
- Ask when the spot first appeared
- Give you a physical exam to check the size, shape, color, and texture of the spot
- Look for other spots on your body
- Feel your lymph nodes to make sure they arent bigger or harder than normal
If your doctor thinks a bump looks questionable, theyll remove a sample of the spot to send to a lab for testing.
Continued
Read Also: Ductal Invasive Carcinoma Survival Rate
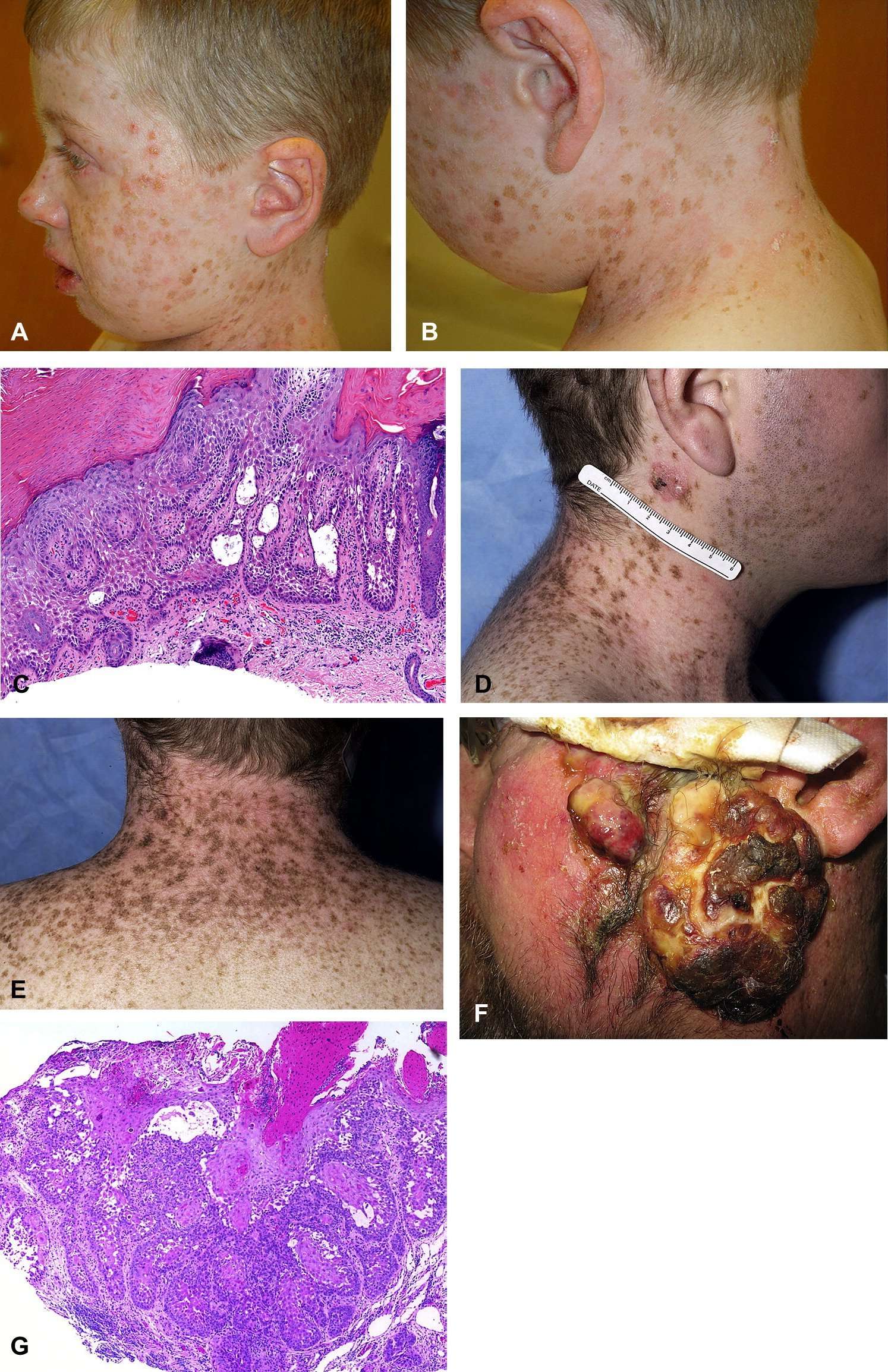
Initiating And Early Events
HPV-negative HNSCC.
Tobacco consumption is the primary risk factor for development of HPV-negative HNSCC. Tobacco consists of over 5,000 different chemicals, of which dozens have been shown to have carcinogenic activity. The chemicals thought to be most responsible for the cancer-causing effects of tobacco are polycyclic aromatic hydrocarbons , including benzopyrene, and nitrosamines, including 4–1–1-butanone and N-nitrosonornicotine ,. In smokeless tobacco, nitrosamines are the dominant carcinogen, whereas the carcinogens in areca nut and betel quid are poorly defined. Tobacco-derived carcinogens, including PAHs and nitrosamines, undergo metabolic activation, with detoxication enzymes and pathways promoting excretion . However, many of the reactive metabolites of these carcinogens can also form covalent DNA adducts, which, if not properly repaired, lead to mutations and other genetic abnormalities. The propensity for tobacco carcinogens to promote genetic changes and neoplastic transformation likely depends on the balance between metabolic activation versus detoxification and DNA repair . The use of tobacco products is also associated with inflammation in the exposed tissues. Coincident with inflammation is the local production of cytokines, chemokines and growth factors that can have an important role in promoting proliferation, angiogenesis and, ultimately, carcinogenesis.
Development of carcinogen-associated, HPV-negative HNSCC.
HPV-positive HNSCC.
Squamous Cell Carcinoma Remedies
Just diagnosed with SCC. Have extensive swelling in neck and arm. Biopsy was done showing SCC but could not pinpoint the primary source of the cancer. Did PET scan which showed the source being in the sinuses and the femor of left leg. Was told that there is no cure, the only option is Radiation and Chemo treatments which can shrink the multiple tumors and if it works would only give me more time and this would have to be repeated as the tumors start growing again. Started the radiation treatments last week and they will continue for several weeks and then chemo for several weeks. They say the most I can even hope for is a max of 18 months. Is there anything that I can do? Please help, willing to try anything.
Also Check: Melanoma Stage 2 Treatment
Different Types Of Cancer Start In The Skin
Skin cancer may form in basal cells or squamous cells. Basal cell carcinoma and squamous cell carcinoma are the most common types of skin cancer. They are also called nonmelanoma skin cancer. Actinic keratosis is a skin condition that sometimes becomes squamous cell carcinoma.
Melanoma is less common than basal cell carcinoma or squamous cell carcinoma. It is more likely to invade nearby tissues and spread to other parts of the body.
This summary is about basal cell carcinoma, squamous cell carcinoma of the skin, and actinic keratosis. See the following PDQ summaries for information on melanoma and other kinds of cancer that affect the skin:
What Are The Risk Factors For Squamous Cell Carcinoma
Risk factors for squamous cell carcinoma include:
- Unprotected exposure to ultraviolet rays
- Light-colored hair, skin, or eyes
- History of skin cancer
- The pathologists report
- Recurrence after treatment
Treatment for squamous cell carcinoma usually involves surgery to remove the lesion. The surgical options include:
- Excision: The physician cuts out the tumor with a scalpel, along with a small margin of healthy skin around the tumor.
- Curettage and electrodesiccation: Used in small lesions, the physician scrapes away cancer cells, then cauterizes the skin to prevent bleeding.
- Mohs surgery: The surgeon removes layers of skin and examines them under a microscope to determine if cancer is present. This process continues until no cancer cells are visible.
Rarely, squamous cell carcinoma is treated with chemotherapy , radiation therapy , and immunotherapy when it has metastasized to other areas of the body.
Recommended Reading: Invasive Ductal Carcinoma Grade 2 Survival Rate
Stage Iii Squamous Cell Carcinoma
The tumor cells may be of any size at the original site. A stage III SCC has begun to invade the nearby lymph nodes on the side of the body of the original cancerous growth. This new growth is still under 3 cm in size. It may also have grown into the facial bones like the bones surrounding the eye or your jaw bone.9 It has not affected any other organs.10
Surgery Radiation And Chemotherapy
Pathological features indicative of increased risk of occurrence include extra-nodal extension, close or involved surgical margins, or perineural invasion when these are present, administration of high-dose cisplatin chemotherapy concurrent with radiation further improves disease-free survival and impacts survival in the highest risk groups,. The use of tri-modality therapy is known to increase the late toxicities of radiation, including chronic dysphagia and aspiration, and might increase the risk of non-cancer mortality in survivors. For this reason, it is considered important to accurately predict the extent of disease, including the presence of extra-nodal extension, prior to initiation of definitive therapy, to avoid the need to add CRT after what was initially projected to be single modality surgical therapy, as currently happens in 65% of node-positive HPV-associated oropharyneal cancer that are managed primarily with resection. Deep-learning neural networks, other radiomics approaches and functional imaging with PET offer promise in improving pre-operative diagnostic accuracy,. Furthermore, there is a > 50% likelihood of distant metastases in patients with HPV-positive oropharyngeal cancer and > 5 nodes involved such patients are also poor candidates for initial surgical management, given the potential positive impact of chemotherapy on micro-metastases.
Also Check: Untreated Cancer Symptoms
How Can Squamous Cell Carcinoma Of Oral Cavity Be Prevented
A few methods to prevent Squamous Cell Carcinoma of Oral Cavity include:
- Maintain proper oral hygiene
- Avoid chewing tobacco and smoking
- Avoid prolonged and chronic exposure to the sun
Regular medical screening at periodic intervals with blood tests, scans, and physical examinations, are mandatory, due to its high metastasizing potential and possibility of recurrence. Often several years of active vigilance is necessary.